|
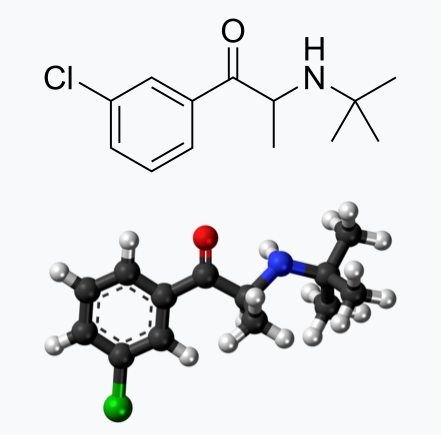
Bupropion, originally named Amfebutamone, sold under the brand name Wellbutrin, is a medication commonly prescribed for the treatment of major depressive disorder (MDD), as is often used off-label for attention deficit hyperactivity disorder (ADHD), anxiety, obesity, and bipolar disorder. While it has demonstrated efficacy in addressing certain mental health issues, it is essential to examine the potential harms associated with its use, particularly considering its modulation of neurotransmitters like norepinephrine (NE) and dopamine. This article aims to shed light on the risks of Wellbutrin use, with a focus on its implications for pregnant or lactating women. Additionally, we'll explore the idea that the indications for Wellbutrin may stem from underlying nutrition and lifestyle factors rather than a deficiency of the medication. prescription trendsAs of 2021, Bupropion, maintained its position as the 18th most prescribed drug in the United States. With an estimated 29,099,445 prescriptions filled, it remains a widely utilized medication in the realm of psychiatric pharmaceuticals. This notable figure underscores the prevalence of its use in addressing various conditions, including depression and smoking cessation. The estimated number of patients in the United States receiving Bupropion in 2021 reached 6,412,363. This statistic reflects the significant impact and reach of Bupropion across diverse patient populations. Its popularity could be attributed to its purported effectiveness in managing depressive disorders, ADHD, anxiety, and aiding individuals in smoking cessation efforts. descriptionWellbutrin (bupropion hydrochloride), unlike any other antidepressant on the market, is chemically characterized as a monocyclic aminoketone, is chemically unrelated to tricyclic, tetracyclic, selective serotonin re‑uptake inhibitor, or other known antidepressant agents. Its structure closely resembles that of diethylpropion; it is related to phenylethylamines. It is designated as (±)-1-(3-chlorophenyl)-2-[(1,1-dimethylethyl)amino]-propanone hydrochloride. Bupropion hydrochloride powder is white, crystalline, and highly soluble in water. It has a bitter taste and produces the sensation of local anesthesia on the oral mucosa. There is documented interindividual variability - everyone responds differently. Neurotransmitter Modulation: The Double-Edged SwordWellbutrin functions by influencing the levels of neurotransmitters in the brain, primarily inhibiting the breakdown of norepinephrine and dopamine. While this mechanism contributes to its antidepressant effects, it also raises concerns about potential side effects and risks. Altering neurotransmitter levels can lead to a range of adverse effects, with the most common including:
Here are some of the possible harms and common side effects associated with Wellbutrin:
While the approach of inhibiting the reuptake of dopamine and norepinephrine aims to enhance the availability of these neurotransmitters in the brain, an imbalance can lead to adverse effects. Excessive levels or prolonged elevated concentrations of these neurotransmitters may contribute to overstimulation and disrupt normal neural signaling. Norepinephrine is a neurotransmitter involved in the body's "fight or flight" response, influencing heart rate and blood pressure. Medications that impact norepinephrine reuptake can lead to cardiovascular side effects, including increased heart rate and elevated blood pressure. Individuals with pre-existing cardiovascular conditions may be at a higher risk for complications. Altered levels of dopamine and norepinephrine can influence mood and behavior. In some cases, inhibiting reuptake may contribute to psychiatric symptoms such as anxiety, restlessness, or irritability. Balancing the desired therapeutic effects with potential adverse psychological consequences is a delicate consideration. Abruptly discontinuing medications that inhibit dopamine and norepinephrine reuptake can lead to withdrawal symptoms. These symptoms may include mood swings, fatigue, and cognitive disturbances. Additionally, some individuals may develop a dependence on these medications, requiring careful management to taper off gradually. Dopamine and norepinephrine play roles in regulating sleep and appetite. Disrupting these neurotransmitters can lead to sleep disturbances, insomnia, or changes in appetite. Monitoring and addressing these side effects are crucial for maintaining overall well-being during the course of treatment. The response to medications that inhibit dopamine and norepinephrine reuptake can vary widely among individuals. Factors such as genetic predispositions, existing medical conditions, and concurrent medications may influence how the body reacts to these interventions. Individualized treatment plans and close monitoring are essential components of responsible prescribing. Impact on Pregnant or Lactating WomenPregnancy and lactation introduce unique considerations when it comes to medication use. The use of Wellbutrin (bupropion) or any other medication during pregnancy requires careful consideration of potential risks and benefits. While studies on the safety of Wellbutrin during pregnancy are inconclusive, there is evidence suggesting a potential association with adverse outcomes, including preterm birth and low birth weight. Additionally, Wellbutrin and its metabolites are present in human breast milk excretions, raising concerns about its impact on nursing infants including alterations in neurotransmitters. Expectant or breastfeeding mothers should engage in thorough discussions with their healthcare providers to weigh the potential benefits against the risks and explore alternative treatment options. Here are some considerations regarding the potential harms of taking Wellbutrin during pregnancy:
Wellbutrin should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus. It's essential for individuals taking Wellbutrin and considering pregnancy, or those who become pregnant while on the medication, to discuss their situation with healthcare professionals. Abruptly stopping antidepressant medication can lead to a recurrence of depressive symptoms, which may have its own set of risks during pregnancy. Healthcare providers will carefully weigh the potential risks and benefits based on the individual's mental health needs. In some cases, healthcare professionals may recommend continuing the medication, adjusting the dosage, or exploring alternative treatments. Pregnant individuals should inform their healthcare providers about their medication use and work collaboratively to make informed decisions that prioritize both maternal mental health and the well-being of the developing fetus. Inactive IngredientsWellbutrin is supplied for oral administration as 75‑mg (yellow‑gold) and 100‑mg (red) film‑coated tablets. Each tablet contains the labeled amount of bupropion hydrochloride and the inactive ingredients:
While the active ingredient in Wellbutrin plays a significant role in its pharmacological effects, it's important not to overlook the inactive ingredients in the formulation. While they make up a smaller portion of the overall product, their cumulative impact should not be underestimated, especially considering the frequent administration of the medication. Though often considered inert, inactive ingredients can still interact with the body in various ways, potentially influencing drug absorption, metabolism, and overall therapeutic efficacy. Moreover, individual sensitivities or allergic reactions to certain inactive ingredients can occur, further emphasizing the importance of evaluating the entire list of components. Even seemingly minor alterations in inactive ingredients can have profound implications, particularly when considering long-term usage. Over time, repeated exposure to these substances may contribute to cumulative effects or unexpected reactions. Therefore, comprehensive scrutiny of all ingredients, active and inactive alike, is essential for a thorough assessment of the safety profile of Wellbutrin and other pharmaceutical products. Impact of Food coloringThe vibrant hues that adorn our favorite processed foods often come from artificial food colorings, but behind the visual appeal lies a potential risk, particularly for pregnant or lactating women. Artificial food color usually contains petroleum and is manufactured in a chemical process that includes formaldehyde, aniline, hydroxides, and sulfuric acids. Most impurities in the food color are in the form of salts or acids. Sometimes lead, arsenic, and mercury may be present as impurities. The U.S. FDA is yet to study the effects of synthetic dyes on behavior in children. To date, there are numerous scientific articles highlighting the relationship of consumption of food colorings to the following health conditions:
Underlying these conditions are the documented mechanics of action that cause physiologic imbalance, which include:
Research has raised concerns about the consumption of food colorings and their potential adverse effects, including implications for conditions like ADHD, autism, and gastrointestinal dysfunction. There is a substantial amount of data exploring the connection between artificial food colorings and ADHD. Researchers suggest that certain artificial colorings may exacerbate hyperactivity and inattention in children with ADHD. Pregnant women, mindful of their diet's impact on fetal development, may choose to limit the intake of foods containing these colorings. The relationship between food colorings and autism spectrum disorders (and the underlying inflammation in the brain) is a topic of ongoing investigation. Meta-analysis have documented a link, emphasizing the need for caution, especially during pregnancy and lactation. As the developing brain is susceptible to external influences, limiting exposure to artificial additives becomes a consideration for expectant and nursing mothers. Artificial food colorings have been associated with gastrointestinal disturbances, ranging from discomfort to more severe issues. Pregnant women, already navigating changes in digestion due to hormonal shifts, may choose to minimize exposure to food colorings to promote digestive well-being during this crucial period. Potential Harms for Pregnant and Lactating Women:
For pregnant or lactating women concerned about the potential harms of food colorings, opting for a diet rich in whole, unprocessed foods becomes a valuable strategy. Choosing fruits, vegetables, and other naturally colorful sources can provide vibrant flavors without the need for artificial additives. While the connection between food colorings and adverse health outcomes is an area of ongoing research, pregnant and lactating women may choose to err on the side of caution. Prioritizing a diet that minimizes artificial additives and focuses on nutrient-dense, whole foods is a proactive step toward supporting both maternal and fetal health. Always consult with healthcare professionals for personalized guidance based on individual circumstances and health considerations. Impact of PEGPolyethylene glycol (PEG) is considered "generally recognized as safe" (GRAS) when used in specific contexts, but some individuals may experience adverse effects. The concerns that arise with the safety of consuming PEG are multifold, including:
Depending on manufacturing processes, PEGs may be contaminated with measurable amounts of ethylene oxide and 1,4-dioxane. The International Agency for Research on Cancer classifies ethylene oxide as a known human carcinogen and 1,4-dioxane as a possible human carcinogen. Ethylene oxide can also harm the nervous system and the California Environmental Protection Agency has classified it as a developmental toxicant based on evidence that it may interfere with human development. 1,4-dioxane is also persistent. In other words, it doesn’t easily degrade and can remain in the environment long after it is rinsed down the shower drain. 1,4-dioxane can be removed from cosmetics during the manufacturing process by vacuum stripping, but there is no easy way for consumers to know whether products containing PEGs have undergone this process.In a study of personal care products marketed as “natural” or “organic” (uncertified), U.S. researchers found 1,4-dioxane as a contaminant in 46 of 100 products analyzed. While carcinogenic contaminants are the primary concern, PEG compounds themselves show some evidence of genotoxicity and if used on broken skin can cause irritation and systemic toxicity. PEG itself is classified as expected to be toxic or harmful as mentioned on the Environment Canada Domestic Substance List. The industry panel that reviews the safety of cosmetics ingredients concluded that some PEG compounds are not safe for use on damaged skin (although the assessment generally approved of the use of these chemicals in cosmetics). Also, PEG functions as a “penetration enhancer,” increasing the permeability of the skin to allow greater absorption of the ingredients — including harmful ingredients. Researchers have observed that a large percentage of parents, caregivers, and practitioners described an explosion of neurological side effects seemingly correlated to polyethylene glycol administration. Those side effects include:
Commonly found in various products, such as medications, laxatives, and skincare items, PEG may lead to the following potential harms:
People with pre-existing health conditions, especially those affecting the kidneys, should inform their healthcare providers before using PEG-containing products. As with any substance, individual responses to PEG can vary, and people experiencing adverse effects should seek medical attention promptly. It's important to weigh the risks and benefits of using PEG-based products based on individual health conditions and circumstances. Impact of TalcTalc is a mineral commonly used in various products such as talcum powder, cosmetics, and personal care items. While talc is considered GRAS for external use, there have been concerns and controversies regarding potential health risks associated with its use, primarily when used in certain ways or in specific product formulations. Here are some of the concerns related to talc:
Individuals concerned about the potential risks of talc-containing products should consider alternatives. As with any substance, moderation and careful use are advisable, and individuals experiencing adverse effects should seek medical advice. Impact of titanium dioxideTitanium dioxide is a widely used pigment and additive in various products, including cosmetics, sunscreens, paints, and food items. While it is generally recognized as safe when used in approved applications, there are concerns about potential health risks associated with certain forms and uses of titanium dioxide. Here are some considerations:
It's important to note that regulatory agencies, such as the U.S. Food and Drug Administration (FDA) and the European Food Safety Authority (EFSA), have assessed the safety of titanium dioxide in approved uses. The permissible limits and specifications vary depending on the application. Consumers concerned about titanium dioxide can choose products with alternatives or consult with healthcare professionals. As research continues, regulatory agencies may update guidelines to ensure the safe use of titanium dioxide in various products. Root Causes vs. MedicationIt's crucial to recognize that the conditions for which Wellbutrin is prescribed—ADHD, anxiety, obesity, and bipolar disorder—may not be caused by a deficiency of Wellbutrin itself. Rather, these conditions are complex and multifaceted, often influenced by underlying nutrition and lifestyle factors. Addressing these root causes is fundamental to comprehensive and sustainable mental health care. Nutrition and Lifestyle Factors: Unveiling the Roots of DepressionDepression, a complex and pervasive mental health condition, often finds its roots in a myriad of factors, extending beyond the realm of neurochemistry to include nutrition and lifestyle elements. Understanding and addressing these underlying factors can play a pivotal role in comprehensive depression management. Here's a closer look at the nutrition and lifestyle aspects that contribute to this intricate mental health landscape: 1. Dietary Choices:
Nutrition and Lifestyle Factors: Off-Label Uses
DeprescriptionAs with many psychotropic medications, Wellbutrin (bupropion) requires careful consideration when discontinuing to minimize the risk of withdrawal symptoms. Abruptly stopping Wellbutrin, also known as going "cold turkey," can lead to uncomfortable and potentially distressing withdrawal symptoms. It is crucial to approach the discontinuation of Wellbutrin with a gradual tapering process, personalized to individual needs, to ensure a smoother transition. Withdrawal symptoms, often associated with sudden cessation of psychotropic drugs, can manifest as a range of physical and psychological discomforts. These may include dizziness, headaches, irritability, mood swings, insomnia, and flu-like symptoms. The severity and duration of withdrawal symptoms can vary from person to person. To mitigate the risk of withdrawal symptoms, the American Psychiatric Association recommends a tapering approach for all antidepressants, including Wellbutrin. Tapering involves gradually reducing the dosage over a specified period, allowing the body to adjust to the decreasing levels of the medication. It is paramount not to discontinue Wellbutrin without consulting your healthcare provider. Your doctor can create a personalized taper schedule based on factors such as the duration of your medication use, your current dosage, and any specific symptoms you may be experiencing. Tapering is typically done over 6 to 8 weeks to provide a gradual adjustment. Every individual responds differently to medication changes. Your doctor can tailor the taper schedule to your unique needs, ensuring a careful balance between minimizing withdrawal symptoms and maintaining mental health stability. If you begin to experience withdrawal symptoms during the tapering process, it is crucial to communicate promptly with your healthcare provider. They may need to reassess your taper schedule or make adjustments based on your symptoms. Restarting Wellbutrin can often alleviate withdrawal symptoms within a few days. The journey of tapering off Wellbutrin is a collaborative effort between you and your healthcare provider. Open communication about your experiences and any emerging symptoms allows for adjustments that prioritize your well-being throughout the process. In the realm of psychotropic medications, a thoughtful and gradual approach to discontinuation is key. Tapering off Wellbutrin under the guidance of your healthcare provider not only minimizes the risk of withdrawal symptoms but also ensures a smoother transition, prioritizing your mental health. Remember, your doctor is your ally in this process, and together, you can navigate the complexities of tapering to promote your overall well-being. ConclusionWhile Wellbutrin has proven efficacy in certain contexts, it's imperative to approach its use with caution, especially considering its potential impacts on neurotransmitter modulation. Pregnant or lactating women should consult their healthcare providers to make informed decisions based on their unique circumstances. Moreover, recognizing that the indications for Wellbutrin may be rooted in broader lifestyle and nutritional factors encourages a more comprehensive approach to mental health care. Collaborative discussions between patients and healthcare professionals can pave the way for personalized and holistic treatment plans that address the underlying causes of mental health conditions. references“Bupropion - Drug Usage Statistics, ClinCalc DrugStats Database.” Clincalc.com, 2021, clincalc.com/DrugStats/Drugs/Bupropion. Medical Expenditure Panel Survey (MEPS) 2013-2021. Agency for Healthcare Research and Quality (AHRQ), Rockville, MD. ClinCalc DrugStats Database version 2024.01.
“Wellbutrin: Package Insert / Prescribing Information.” Drugs.com, www.drugs.com/pro/wellbutrin.html. Starr P, Klein-Schwartz W, Spiller H, Kern P, Ekleberry SE, Kunkel S. Incidence and onset of delayed seizures after overdoses of extended-release bupropion. Am J Emerg Med. 2009 Oct;27(8):911-5. doi: 10.1016/j.ajem.2008.07.004. PMID: 19857406. Spiller, Henry A., et al. “Bupropion Overdose: A 3-Year Multi-Center Retrospective Analysis.” The American Journal of Emergency Medicine, vol. 12, no. 1, Jan. 1994, pp. 43–45, https://doi.org/10.1016/0735-6757(94)90195-3. Accessed 28 Nov. 2021. Bakthavachalu, Prabasheela, et al. “Food Color and Autism: A Meta-Analysis.” Advances in Neurobiology, vol. 24, 2020, pp. 481–504, pubmed.ncbi.nlm.nih.gov/32006369/#:~:text=Many%20families%20with%20autistic%20children, https://doi.org/10.1007/978-3-030-30402-7_15. Hussain, Sunny Z., et al. “Probable Neuropsychiatric Toxicity of Polyethylene Glycol: Roles of Media, Internet and the Caregivers.” GastroHep, vol. 1, no. 3, May 2019, pp. 118–123, https://doi.org/10.1002/ygh2.336. Sellaturay, Priya, et al. “Polyethylene Glycol–Induced Systemic Allergic Reactions (Anaphylaxis).” The Journal of Allergy and Clinical Immunology: In Practice, Oct. 2020, https://doi.org/10.1016/j.jaip.2020.09.029. “Drugs & Medications.” Webmd.com, 2019, www.webmd.com/drugs/2/drug-17118/polyethylene-glycol-3350-oral/details. Black RE, Hurley FJ, and Havery DC. “Occurrence of 1,4-dioxane in cosmetic raw materials and finished cosmetic products.” Int J PharJ AOAC Int. 84, 3 (May-Jun 2001):666-70. Brashear, A. et al. “Ethylene oxide neurotoxicity: a cluster of 12 nurses with peripheral and central nervous system toxicity.” Neurology 46, 4 (Apr 1996):992-8. California. EPA. Office of Environmental Health Hazard Assessment. Chemicals Known to the State to Cause Cancer or Reproductive Toxicity. February 5, 2010.https://www.oehha.org/prop65/prop65_list/files/P65single020510.pdf Environmental Health Association of Nova Scotia. Guide to Less Toxic Products.Halifax: EHANS, 2004. https://www.lesstoxicguide.ca/index.asp?fetch=personal#commo. OCA (Organic Consumer Association). 2008. Consumer alert. Cancer-causing 1,4-dioxane found in personal care products misleadingly branded as natural and organic. Available: https://www.organicconsumers.org/bodycare/DioxaneRelease08.cfm Wangenheim J and Bolcsfoldi G. “Mouse lymphoma L5178Y thymidine kinase locus assay of 50 compounds.” Mutagenesis 3, 3 (May 1988):193-205. Biondi O, Motta S, and Mosesso P. “Low molecular weight polyethylene glycol induces chromosome aberrations in Chinese hamster cells cultured in vitro.” _Mutagenesis_17, 3 (May 2002):261-4. Lanigan, RS (CIR Expert Panel). “Final report on the safety assessment of PPG-11 and PPG-15 stearyl ethers.” Int J Toxicol.20 Suppl 4 (2001):13-26 Cosmetic Ingredient Review. Ingredient Reports — Quick Reference Table (summarizing publications through Dec 2009). https://www.cir-safety.org/staff_files/PublicationsListDec2009.pdf Epstein, S with Fitzgerald, R. Toxic Beauty. Dallas: BenBella Books, 2009: 158-9. Chen, Tao , et al. “Genotoxicity of Titanium Dioxide Nanoparticles.” Journal of Food and Drug Analysis, vol. 22, no. 1, 1 Mar. 2014, pp. 95–104, https://www.sciencedirect.com/science/article/pii/S102194981400009X, https://doi.org/10.1016/j.jfda.2014.01.008.
0 Comments
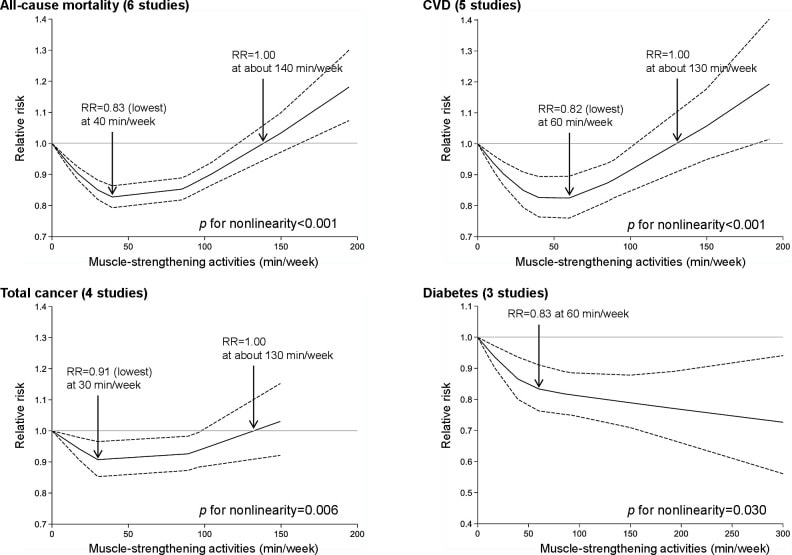
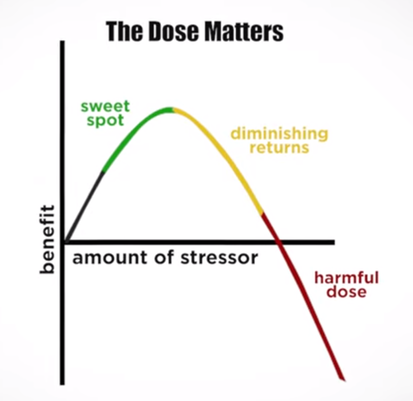
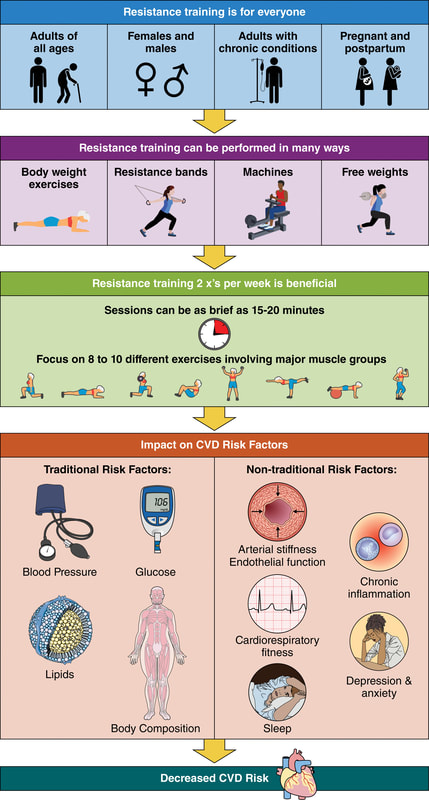
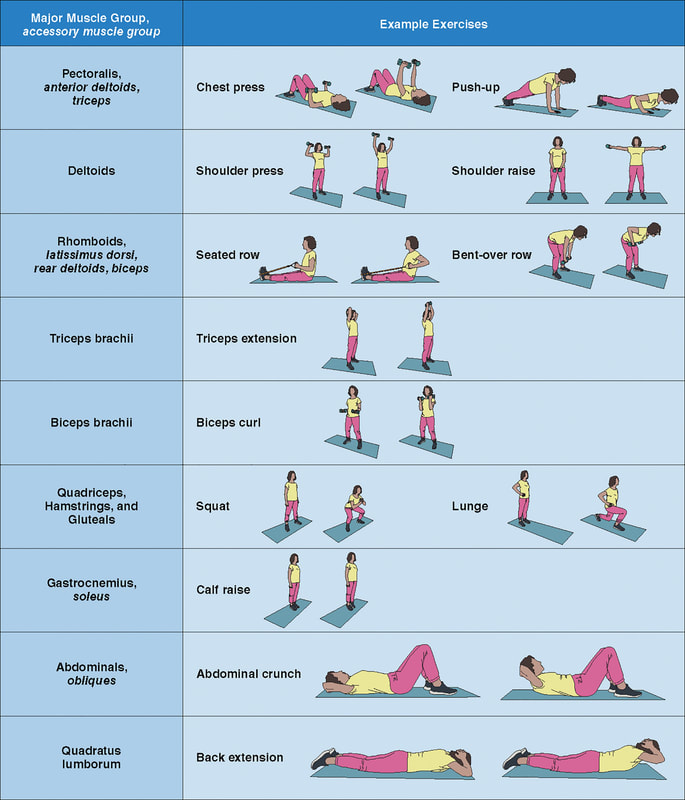
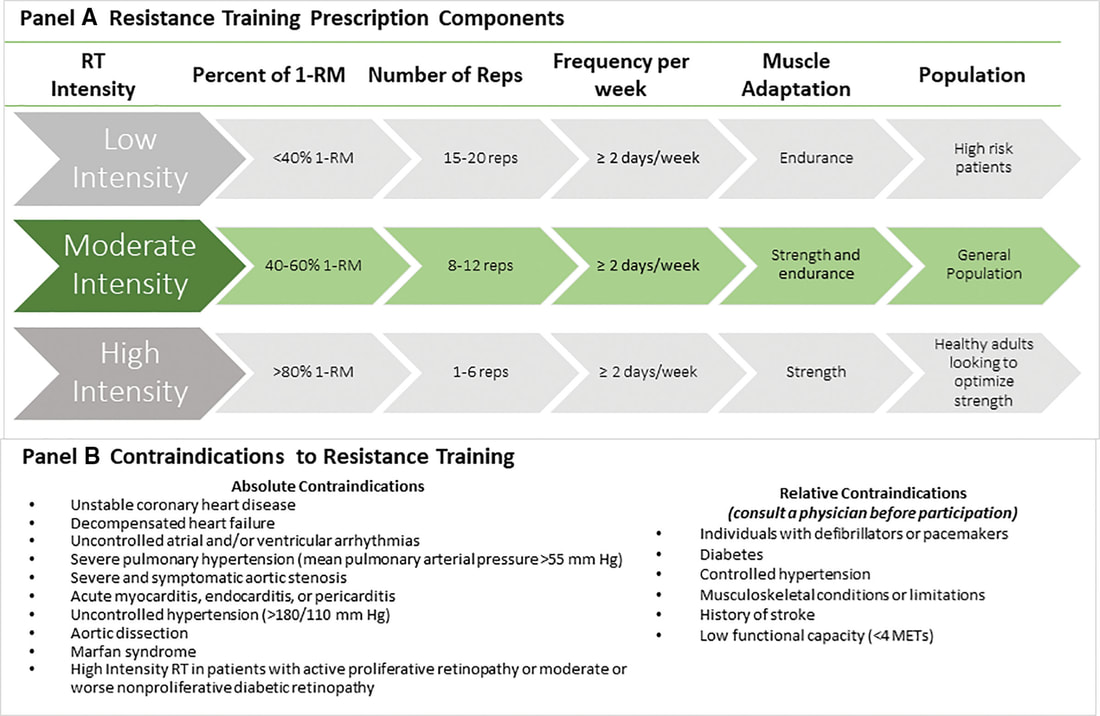
In an update to its 2007 scientific statement, the American Heart Association (AHA) emphasizes the significant and multifaceted benefits of resistance training (RT) on cardiovascular health. Contrary to the misconception that RT solely enhances muscle mass and strength, the statement highlights the favorable physiological and clinical effects of this form of exercise on cardiovascular disease (CVD) and associated risk factors. The scientific statement aims to provide comprehensive insights into the impact of RT, either alone or in combination with aerobic training, on traditional and nontraditional CVD risk factors. More is not always betterEpidemiological evidence suggests that RT is associated with a lower risk of all-cause mortality and CVD morbidity and mortality. Adults who participate in RT have ≈15% lower risk of all-cause mortality and 17% lower risk of CVD, compared with adults who report no RT. Approximately 30 to 60 minutes per week of RT is associated with the maximum risk reduction for all-cause mortality and incident CVD. Notice this "U" shape in the curve when examining the relationship between RT and morbidity and mortality. This curve suggests that some RT is clearly beneficial, but has the volume of RT increases past a certain point the benefits drop and it becomes harmful. The concept of a "biphasic response" is fundamental to understanding hormesis. It describes the characteristic dose-response relationship observed in hormetic processes, where a substance or stressor elicits opposite effects at low and high doses. The response can be visualized as a U-shaped or J-shaped curve, illustrating the beneficial effects at low doses and potential harm at higher doses. Benefits of RT on Traditional CVD Risk FactorsThe AHA's scientific statement underscores the positive influence of RT on traditional CVD risk factors, including blood pressure (BP), glycemia, lipid profiles, and body composition. Numerous studies indicate that engaging in RT is associated with reduced resting BP, improved glycemic control, and favorable alterations in lipid profiles, contributing to a lower risk of all-cause mortality and CVD morbidity. Despite recommendations suggesting 2 days per week of RT, only 28% of U.S. adults adhere to this guideline, highlighting the need for increased awareness and promotion. RT and resting blood pressureRT has demonstrated the ability to reduce resting BP across diverse populations, with notable benefits observed in individuals with prehypertension and hypertension. The mechanisms behind these benefits include enhancements in endothelial function, vasodilatory capacity, and vascular conductance. The reductions in BP achieved through RT are comparable to those achieved with antihypertensive medications. RT and GlycemiaRT shows promise in improving glycemia and insulin resistance, leading to a lower incidence of diabetes. The evidence suggests a nonlinear dose-response association, with up to 60 minutes per week of RT associated with the maximum risk reduction for diabetes. RT and Lipid ProfilesWhile the effect on lipid profiles is modest, RT results in favorable changes in high-density lipoprotein cholesterol, total cholesterol, and triglycerides. These improvements are more pronounced in older adults and those with elevated cardiometabolic risk. Rt, Body composition, and weightRT positively influences body composition by increasing lean body mass and reducing body fat percentage. It is particularly effective in overweight or obese individuals, contributing to increased metabolic rate and mitigating weight gain over time. Benefits of RT on Nontraditional CVD Risk FactorsIn addition to traditional risk factors, the scientific statement highlights the potential mechanisms by which RT positively affects nontraditional CVD risk factors. These include increased cardiorespiratory fitness, improved endothelial function, and potential benefits for sleep quality, psychological health, and well-being. The AHA's updated scientific statement reinforces the pivotal role of resistance training in cardiovascular health, providing a comprehensive overview of its impact on both traditional and nontraditional risk factors. As the evidence supporting RT's benefits continues to grow, the statement serves as a valuable resource for clinicians and public health professionals, offering practical strategies for promoting and prescribing resistance training to enhance cardiovascular health in diverse populations. ReferencesPaluch, Amanda E, et al. “Resistance Exercise Training in Individuals with and without Cardiovascular Disease: 2023 Update: A Scientific Statement from the American Heart Association.” Circulation, 7 Dec. 2023, https://doi.org/10.1161/cir.0000000000001189. Accessed 11 Dec. 2023.
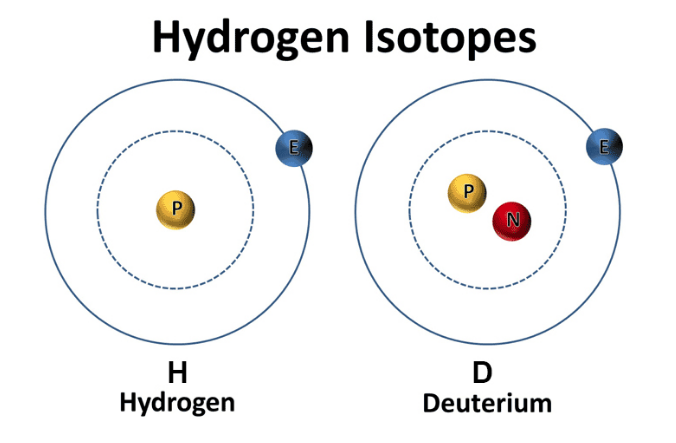
Momma H, Kawakami R, Honda T, Sawada SS. Muscle-strengthening activities are associated with lower risk and mortality in major non-communicable diseases: a systematic review and meta-analysis of cohort studies. Br J Sports Med. 2022 Jul;56(13):755-763. doi: 10.1136/bjsports-2021-105061. Epub 2022 Feb 28. PMID: 35228201; PMCID: PMC9209691. Hydrogen comes in two “flavors”: regular hydrogen, which is actually called protium, and deuterium. Deuterium has all of the same properties as hydrogen, except that it's twice as big and heavy. This is due to an added neutron paired with the proton in the nucleus. Because of this, deuterium is also referred to as "heavy hydrogen," and it actually behaves quite differently from regular hydrogen in chemical reactions and in our bodies. In nature, deuterium helps things grow. For example, deuterium is biologically necessary for growth in babies, teenagers, and developing plants and animals. But once you stop growing, having too much deuterium in your cells can result in mitochondrial dysfunction and lead to premature aging, metabolic problems, and disease. Deuterium is like thick, gluggy oil - when you put thick oil into an engine, the engine sputters, makes strange noises, and eventually breaks. Nature has put systems in place to deplete deuterium and protect the nanomotors, or "little engines," in our cells’ mitochondria from coming into contact with this thick oil. However, the side effects of a modern life - pollution, global warming, processed foods, less healthy lifestyles, etc. - have resulted in many people having way too much deuterium inside their cells. This results in an inability to effectively deplete deuterium and the destruction of our nanomotors. This starts a vicious cycle of deuterium building up and breaking more of our nanomotors. Fewer nanomotors means less energy and more sickness and disease. While deuterium is a natural and essential element, its presence has increased in the modernized environment within the food, atmosphere, and water. Deuterium levels is food will vary based o where that food is grown - deuterium is highest in the equator and in low elevations. Foods high in fat, as well as green plants, including algae and spirulina, which contain high amounts of chlorophyll, are lower in deuterium than fruits, roots, and underground vegetables. As it turns out, GMO foods tainted with glyphosate, as well as processed, synthetically made foods, possess high amounts of deuterium. There are various lifestyle practices that have led to increased deuterium levels including a lack of sleep, particularly deep REM sleep. In addition, breathing shallow and fast via the mouth and chest also contributes to elevated levels of deuterium. Researchers have demonstrated that elevated of deuterium can contribute to:
Learn More About Deuterium Depletion References Understanding Deuterium - The Center for Deuterium Depletion. (2019). Retrieved 24 December 2019, from https://www.ddcenters.com/about-deuterium-2-2-2/
Over the course of the past century, the Western culture has faced numerous health epidemics, from obesity to opioids. Today we are facing an epidemic of a different nature. The epidemic of loneliness. We're more connected than ever, but are we feeling more alone? In the last 50 years, rates of loneliness have doubled in the United States. In a survey of over 20,000 American adults, it was found that almost half of respondents reported feeling alone, left out, and isolated. Further, one in four Americans shared that they rarely feel understood, and one in five people believe they rarely or never feel not close to people. Loneliness is on the rise for Americans regardless of geographic location, gender, race, or ethnicity. Human beings did not evolve to be alone. Sociality plays a fundamental part in the wellbeing of Homo sapiens. Conversely, social isolation and loneliness are known risk factors for premature death, more so than being obese (Holt-Lunstad et al., 2015). Individuals who feel socially isolated and alone also have higher rates of cardiovascular disease, alcoholism and suicidality, physical diseases related to stress and compromised immune function, and in later life, greater risk of degenerative dementia. Even worse, researchers have observed that geriatric individuals who are considered lonely have a 45% increased risk of mortality (Leland, 2012; Perissinotto, Stijacic Cenzer and Covinsky, 2012). Moreover, lonely individuals experience reductions in reasoning and creativity. In addition to these reduced abilities, loneliness affects workplace productivity, as lonely individuals report less job satisfaction and are more likely to face unemployment. Not surprisingly, loneliness is commonly correlated with mental health concerns such as anxiety and depression. Similarly, loneliness is often associated with poor coping mechanisms, such as compulsive technology use, smoking, and self-harm. In other words, loneliness has both physical and psychological implications, many of which could be long term. Alone versus Lonely Before determining yourself as lonely, there is a difference between being alone and feeling lonely. Being alone and feeling lonely are not mutually dependent. Loneliness is a subjective experience, a feeling of sadness stemming from isolation or abandonment. But, a person can be alone without feeling lonely, since alone describes a state of being and lonely describes an emotional response to one's circumstance. For example, most people don't feel sad when they go to the restroom by themselves. A person can be alone in the sense that no other people are present, or alone in the sense that they are unaccompanied, even in a crowd. When assessing loneliness, introverted and extroverted personalities should be taken into account, because some people enjoy the presence of being alone with themselves, whereas others are dependent on others to cope with not being by themselves. Being at either end of the spectrum, whether it is total isolation or complete dependence, is not considered a healthy behavioral pattern. Factors Influencing LonelinessThe predictors of loneliness is the basis for the identification of factors that cause and contribute to loneliness. The are three broad categories that influence the feeling of loneliness:
These categories may be subdivided into multiple factors that increase loneliness:
While it is impossible to avoid loneliness completely, it may be alleviated. It is recommended to investigate the contributory factors towards loneliness because knowledge of these may substantially lessen the impact of loneliness on people's mental health status. Such knowledge will contribute to an improved quality of life, productivity and health. Sleep Deprivation-Induced Loneliness The "loneliness phenotype" can be triggered by sleep deprivation. Researchers have observed that a lack of sleep induces critical changes within the brain, altering behavior and emotions, while also disturbing essential metabolic processes and influencing the expression of immune-related genes. The end result is that people who are sleep-deprived avoid social interaction. This asocial profile is recognizable by other people, who, in turn, shun the sleep-deprived people in a psychosocial loop that perpetuates in a vicious cycle of loneliness and other mental health disorders. Some Solutions to Loneliness REferences Ali, S. (2018). What You Need to Know About the Loneliness Epidemic. [online] Psychology Today. Available at: https://www.psychologytoday.com/us/blog/modern-mentality/201807/what-you-need-know-about-the-loneliness-epidemic [Accessed 1 Sep. 2019].
Harris, R. (2015). Are we lonelier than ever?. [online] The Independent. Available at: https://www.independent.co.uk/life-style/health-and-families/features/the-loneliness-epidemic-more-connected-than-ever-but-feeling-more-alone-10143206.html [Accessed 1 Sep. 2019]. Holt-Lunstad, J., Smith, T., Baker, M., Harris, T. and Stephenson, D. (2015). Loneliness and Social Isolation as Risk Factors for Mortality. Perspectives on Psychological Science, 10(2), pp.227-237. https://doi.org/10.1177/1745691614568352 Leland, K. (2012). Loneliness Linked to Serious Health Problems and Death Among Elderly. [online] UC San Francisco. Available at: https://www.ucsf.edu/news/2012/06/98644/loneliness-linked-serious-health-problems-and-death-among-elderly [Accessed 1 Sep. 2019]. Perissinotto, C., Stijacic Cenzer, I. and Covinsky, K. (2012). Loneliness in Older Persons. Archives of Internal Medicine, 172(14). https://doi.org/10.1001/archinternmed.2012.1993 Ben Simon, E. and Walker, M. (2018). Sleep loss causes social withdrawal and loneliness. Nature Communications, 9(1). https://doi.org/10.1038/s41467-018-05377-0 What is the fastest way to health? It's simply honesty being honest with yourself. We each have four doctors within ourselves: Dr. Happiness, which is what is our concept of what makes us happy (what am you living for?); Dr. Quiet which is how do you create adequate rest to regenerate yourself to have a clear mind and to let my body recover from any stress; Dr. Diet (how do you tune into your body's particular nutritional needs?); and Dr. Movement, which is the difference between Working Out and Working In and putting those movement types to use in your life.
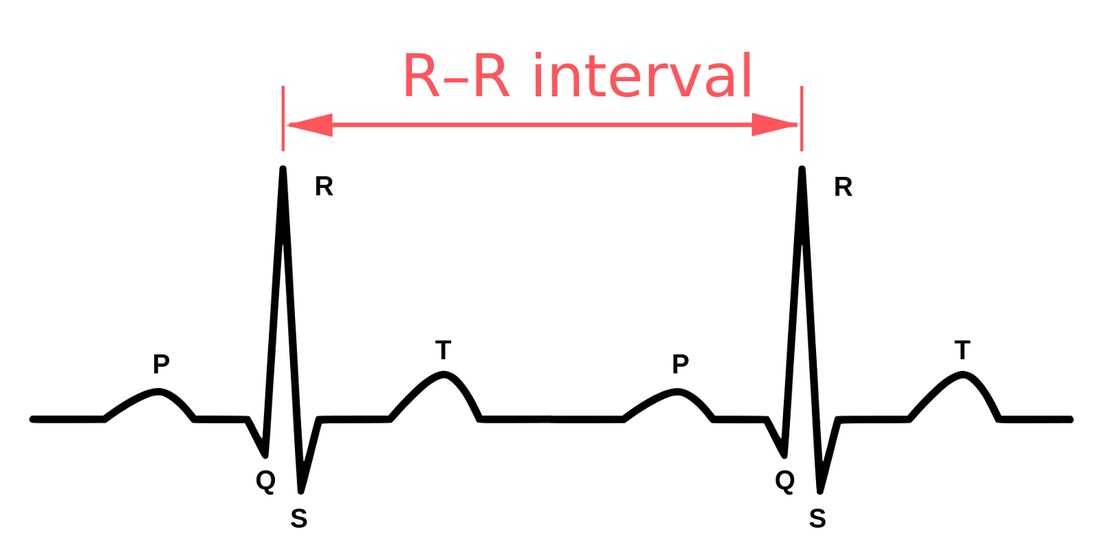
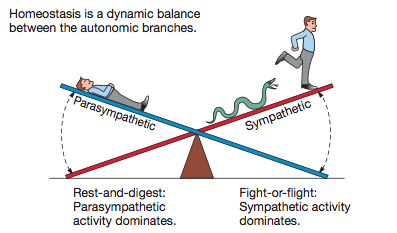
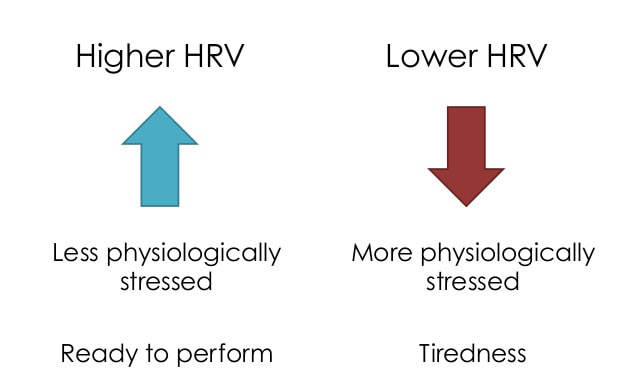
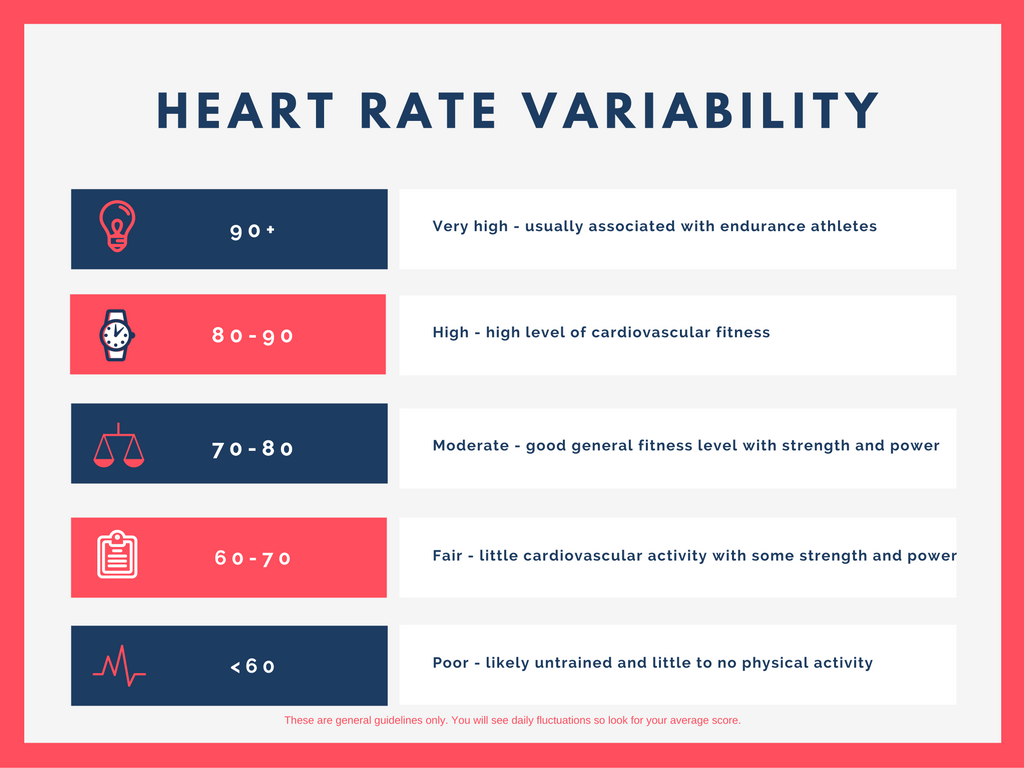
Have you ever wondered what the health impact of a stressful day was? Will you perform well during your long run or training session tomorrow morning? Is there anything you can do today that would improve your ability to have a better day tomorrow? HRV may be a piece of data that could help you answer these questions. What is HRV? HRV is simply a measure of the variation in time between each heartbeat, also known as the RR interval. This variation is controlled by a primitive part of the nervous system called the autonomic nervous system (ANS). The ANS works regardless of our desire and regulates, among other things, our heart rate, blood pressure, breathing, and digestion. The ANS is subdivided into two large components, the sympathetic and the parasympathetic nervous system, also known as the fight-or-flight mechanism and the relaxation response. The brain is constantly processing information in a region called the hypothalamus. The hypothalamus, through the ANS, sends signals to the rest of the body either to stimulate or to relax different functions. It responds not only to a poor night of sleep, or that sour interaction with your boss, but also to the exciting news that you got engaged, or to that delicious healthy meal you had for lunch. Our body handles all kinds of stimuli and life goes on. However, if we have persistent instigators such as stress, poor sleep, unhealthy diet, dysfunctional relationships, isolation or solitude, and lack of exercise, this balance may be disrupted, and your fight-or-flight response can shift into overdrive. Why Monitor HRV? HRV is a noninvasive way to identify these ANS imbalances. If a person’s system is in more of a fight-or-flight mode, the variation between subsequent heartbeats is low. If one is in a more relaxed state, the variation between beats is high. In other words, the healthier the ANS the faster you are able to switch gears, showing more resilience and flexibility. Over the past few decades, research has shown a relationship between low HRV and worsening depression or anxiety. A low HRV is even associated with an increased risk of death and cardiovascular disease (Buccelletti et al., 2009; Tsuji et al., 1994). People who have a high HRV may have greater cardiovascular fitness and be more resilient to stress. HRV may also provide personal feedback about your lifestyle and help motivate those who are considering taking steps toward a healthier life. It is fascinating to see how HRV changes as you incorporate more mindfulness, meditation, sleep, and especially physical activity into your life. For those who love data and numbers, this can be a convenient way to track how your nervous system is reacting not only to the environment, but also to your emotions, thoughts, and feelings. Measuring HRV The gold standard to measure HRV is to analyze a long strip of an electrocardiogram, the test that occurs frequently in medical offices where wires are attached to the chest. But over the past few years, several companies have created heart rate monitors that sync with apps that do something similar. The accuracy of these methods is still under scrutiny, but the technology is improving substantially. A word of caution is that there are no agencies regulating these devices, thus they may not be as accurate as claimed to be. With that said, the easiest and cheapest way to check HRV is to buy a chest strap heart monitor (e.g., Polar H10) and download a free app (e.g., Elite HRV) to analyze the data. The chest strap monitor tends to be more accurate than wrist or finger devices. Check your HRV in the mornings after you wake up, a few times a week, and track for changes as you incorporate healthier interventions. Tracking HRV may be a great tool to motivate behavioral change for some. HRV measurements can help create more awareness of how you live and think, and how your behavior affects your nervous system and bodily functions. While it obviously can’t help you avoid stress, it could help you understand how to respond to stress in a healthier way. While there are questions about measurement accuracy and reliability, if you decide to use HRV as another piece of data, do not get too confident if you have a high HRV, or too scared if your HRV is low. Think of HRV as a preventive tool, a visual insight into the most primitive part of your brain. Increasing HRV Far from the metronome we might assume it to be, the healthiest heart beat follows a fractal pattern, with varying lengths of time separating each pulse (Tapanainen et al., 2002; Yaniv, Y., Lyashkov, A. E., Lakatta, E. G., 2013). A higher HRV suggests a relaxed, low-stress physiological milieu, while a lower HRV indicates a need for recovery, rest, and sleep. Therefore, in order to increase HRV, generally speaking, a more relaxed, low-stress environment is desirable. While there are a number of ways to reduce stress and increase relaxation, here are some examples that have been observed to increase HRV:
References
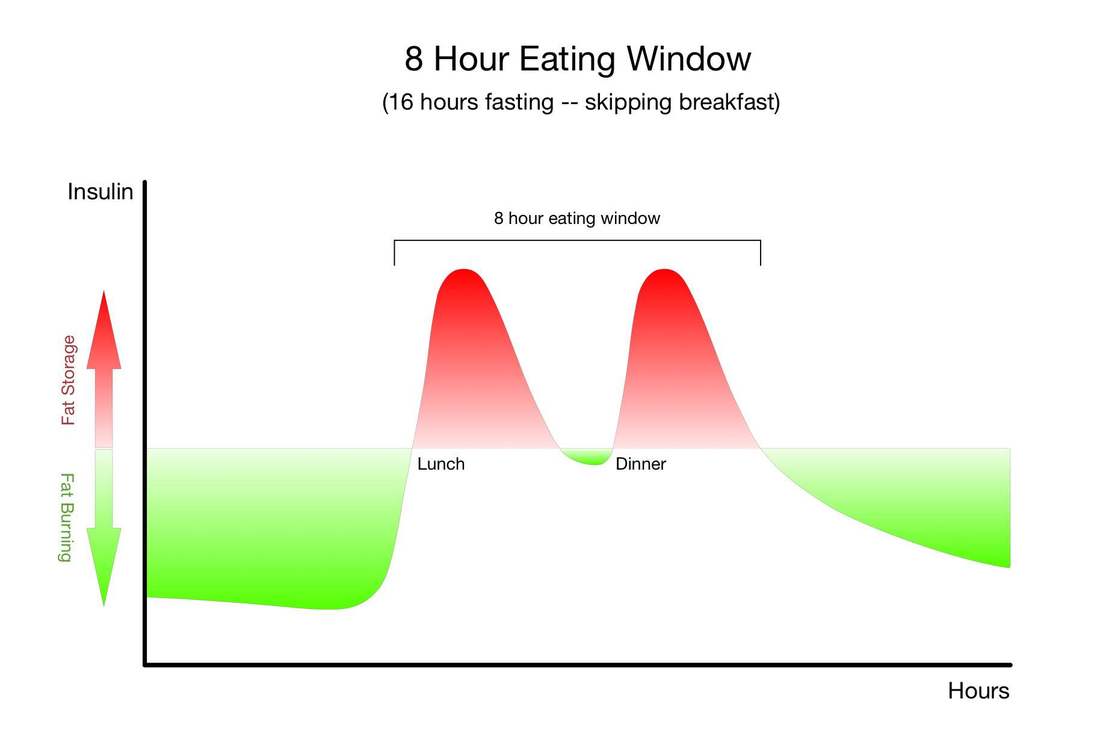
Physiologically, fasting:
The only other strategy that has so many research-baked benefits for longevity is long-term calorie restriction, which requires a significant long-term reduction in the amount of food you eat so that you are essentially living on the brink of starvation. Compliance with calorie-restricted diets is abysmal. Fortunately, there are many ways to fast, and there is likely a form of fasting out there that you will be able to tolerate and incorporate into your life. It's important for you to remember that fasting can provide nearly identical benefits without the pain, suffering, and compliance challenges of calorie restriction. Instead of regulating how much food you eat, as with long-term calorie restriction, you only need to modify when you eat - and of course wisely choose the foods you do eat.Simply cycling between periods of eating and fasting on a daily, weekly, or monthly schedule has been shown to provide many of the same benefits as long-term calorie restriction. Choosing when to eat and when to fast in this way is known as "intermittent fasting." "Don't eat less - eat less often." |
Location |
How Long |
How Often |
Local neighborhood |
<15 minutes |
Daily |
Local park |
1-24 hours |
Weekly |
National Park |
1-3 days |
Monthly |
Remote area |
3-9 days |
Quarterly - Yearly |
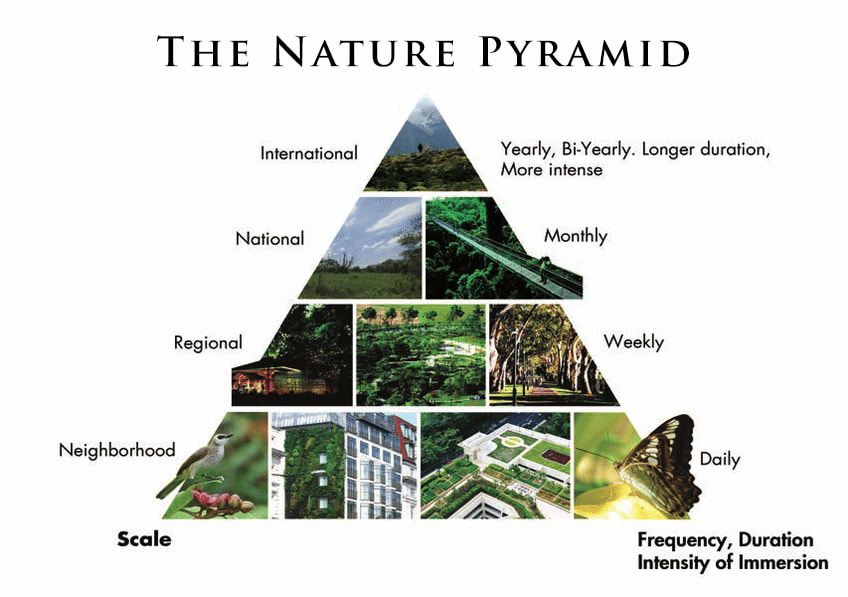
A Solution: Shinrin-yoku (Forest Bathing)
Researchers (Hansen, Jones and Tocchini, 2017) have determined with the healing components of Shinrin-yoku specifically hones in on the therapeutic effects on:
- the immune system function (increase in natural killer cells/cancer prevention);
- cardiovascular system (hypertension/coronary artery disease);
- the respiratory system (allergies and respiratory disease);
- depression and anxiety (mood disorders and stress);
- mental relaxation (Attention Deficit/Hyperactivity Disorder) and;
- human feelings of “awe” (increase in gratitude and selflessness)
How to Forest Bath
- Get Outside - Find a forest or a peaceful outdoor space where you can take a walk or just relax.
- Keep It Simple - Go alone, or with a friend who’s willing to keep conversation to a minimum. Forest bathing isn’t the time to catch up about work etc. It’s meant for relaxation and breathing in the scent of pine or eucalyptus. It’s meant for unwinding.
- Clear Your Mind - Walk on a path or sit in an area where you don’t have to worry about getting lost and you can just empty your mind. A lot of people have compared forest bathing to meditation, which is essentially what it is. Don’t spend the whole time optimizing your mental to-do list. Just take a break and have a look around. Wild and remote places are some of the best to get in your first forest bathing experience.
References
Hansen, M., Jones, R. and Tocchini, K. (2017). Shinrin-Yoku (Forest Bathing) and Nature Therapy: A State-of-the-Art Review. International Journal of Environmental Research and Public Health, 14(12), p.851. https://doi.org/10.3390/ijerph14080851
Kotera, Y., Richardson, M. & Sheffield, D. (2022). Effects of Shinrin-Yoku (Forest Bathing) and Nature Therapy on Mental Health: a Systematic Review and Meta-analysis. Int J Ment Health Addiction 20, 337–361. https://doi.org/10.1007/s11469-020-00363-4
Li, Q. (2009). Effect of forest bathing trips on human immune function. Environmental Health and Preventive Medicine, 15(1), pp.9-17. https://doi.org/10.1007/s12199-008-0068-3
Li Q. (2022). Effects of forest environment (Shinrin-yoku/Forest bathing) on health promotion and disease prevention -the Establishment of "Forest Medicine". Environ Health Prev Med. doi: 10.1265/ehpm.22-00160. PMID: 36328581; PMCID: PMC9665958.
Louv, R. (2012). The Nature Principle: Reconnecting with Life in a Virtual Age. Algonquin Books.
Reported Biological Phenomena (*Effects') and Some Clinical Manifestations Attributed to Microwave and Radio-Frequency Radiation
A. Heating of Organs*
(Applications: Diathermy, Electrosurgery, Electro-coagulation, Electrodesiccation, Electrotomy)
- Whole Body (temperature regulation defects), Hyperpyrexia
- Skin
- Bone and Bone marrow
- (a) Lens of Lye (cataractous lesions - due to the avascular nature of the lens which prevents adequate heat dissipation (b) Corneal damage also possible at extremely high frequencies
- Cenitalia (tubular degeneration of testicles)
- Brain
- Sinuses
- Metal Implants (burns near hip pins, etc.)
B. Changes in physiologic function
- Striated Muscle Contraction
- Alteration of Diameter of Blood Vessels (increased Vascular elasticity, Dilation
- Changes in Oxidative Processes in Tissues and Organs
- Liver Enlargement
- Altered Sensitivity to Drug Stimuli
- Decreased Spermatogenesis (decreased fertility, to sterility)
- Altered Sex Ratio of Births (more girls!)
- Altered Menstrual Activity
- Altered Fetal Development
- Increased Lactation in Nursing Mothers
- Reduction in Piuresis (Na+ excretion, via urine output)
- Altered Renal function (decreased filtration in tubules)
- Changes in Conditioned Reflexes
- Increased Electrical Resistance of Skin
- Changes in the Structure of Skin receptors of the (a) Digestive, and (b) Blood Carrying Systems
- Altered BIood Flow Rate
- Alterations In the Biocurrents (EEG?) of the Cerebral Cortex (in animals)
- Changes In the Rate of Clearance of Tagged Ions from Tissue
- Reversible Structural Changes In the Cerebral Cortex and the Diencephalon
- Electrocardiographic (EKG) Changes
- Alterations In Sensitivity to Light, Sound, and Olfactory Stimuli
- Functional (a) and Pathological (b) Changes in the Eyes: (a) decrease in size of blind spot, altered color recognition, changes in intraocular pressure, lacrimation, trembling of eye-lids; (b) less opacity and coagulation, altered tissue respiration, and altered reduction-oxidation processes
- Myocardial Necrosis
- Hemorrhage in Lungs, Liver, Gut, and Brain (At Fatal Levels of Radiation)
- Generalized Degeneration of all Body Tissue of Radiation (At Fatal Levels of Radiation)
- Loss of Anatomical Parts
- Death
- Dehydration
- Altered Rate of Calcification of Certain Tissue
C. Central Nervous System Effects
- Headaches
- Insomnia
- Restlessness (Awake and During Sleep)
- Electroencephalographic (EEG) Changes
- Cranial Nerve Disorders
- Pyramidal Tract Lesions
- Conditioned Reflex Disorders
- Vagomimetic Action of the Heart; Sympaticomimetic Action
- Seizures, Convulsions
D. Autonomic Nervous System Effects
- Degenerative Disorders (e.g., alteration of heart rhythm)
- Fatigue
- Structural Alterations in the Synapses of the Vagus Nerve
- Stimulation of Parasympathetic Nervous System (Bradycardia), and Inhibition of the Sympathetic Nervous System
E. Peripheral Nervous System Effects
- Effects on Locomotor Nerves
F. Psychological Disorders ("Human Behavioral Studies") - the so-called "Psychophysiologic (and Psychosomatic) Responses"
- Neurasthenia - (general "bad" feeling)
- Depression
- Impotence
- Anxiety
- Lack of Concentration
- Hypochondria
- Dizziness
- Hallucinations
- Sleepiness
- Insomnia
- Increased Irritability
- Decreased Appetite
- Loss of Memory
- Scalp Sensations
- Increased Fatigability
- Chest pain
- Tremor of the hand
G. Behavioral Changes (Animal)
- Reflexive, Operant, Avoidance, and Discrimination Behaviors
H. Blood Disorders
changes in:
- Blood and Bone Marrow
- Phagocytic (polymorphs) and Bactericidal Functions
- Hemolysis Rate (increase), (a shortened lifespan of cells)
- Sedimentation Rate (increase), due to changes in serum concentration levels or amount of fibrinogen. (?))
- Number of Erythrocytes (decrease), also number of lymphocytes
- Blood Glucose Concentration (increase)
- Blood Histamine Content
- Cholesterol and Lipids
- Gamma (also alpha and beta) Globulin, and Total Protein Concetration
- Number of Eosinophils
- Albumin/Globulin Ratio (decrease)
- Hemopoiesis (rate of formation of blood corpuscles)
- Leukopenia (increase in number of white cells), and Leukocytosis
- Reticulocytosis
I. Vascular Disorders
- Thrombosis
- Hypertension
J. Enzyme and Other Biochemical Changes
Changes in activity of:
- Cholinesterase
- Phosphatase
- Transaminase
- Amylase
- Carboxydismutase
- Protein Denaturation
- Toxin, Fungus, and Virus Inactivation (at high radiation dose levels), Bacteriostatic Effect
- Tissue Cultures Killed
- Alteration In Rate of Cell Division
- Increased Concentration of RNA in Lymphocytes, and Decreased Concentration in Brain. Liver, and Spleen
- Changes in Pyruvic Acid, Lactic Acid, and Creatinine Excretions
- Change in Concentration of Glycogen in Liver (Hlyperglycemia)
- Alteration in Concentration of 17- Ketosteroids in Urine
K. Metabolic Disorders
- Glycosuria (sugar in urine; related with blood sugar?)
- Increase in Urinary Phenol (derivatives? DOPA?)
- Alteration of rate of metabolic Enzymatic Processes
- Altered Carbohydrate Metabolism
L. Gastro-Intestinal Disorders
- Anorexia (loss of appetite)
- Epigastric Pain
- Constipation
- Altered Secretion of Stomach "Digestive Juices"
M. Endocrine Gland Changes
- Altered Pituitary Function
- Hyperthyroidism
- Thyroid Enlargement
- Increased Uptake of Radioactive Iodine by Thyroid Gland
- Altered Adrenal Cortex Activity
- Decreased Corticosteroids in Blood
- Decreased Glucocorticoidal Activity
- Hypogonadism (usually decreased testosterone production)
N. Histological Changes
- Changes in Tubular Epithelium of Testicles
- Gross Changes
O. Genetic and Chromosomal Changes
- Chromosome Aberrations (e.g., linear shortening, pseudochiasm, diploid structures, amitotic division, bridging, "sticky" chromosomes, irregularities in chromosomal envelope)
- Mutations
- Mongolism
- Somatic Alterations (changes in cell not involving nucleus or chromosomes, cellular transformation)
- Neoplastic Diseases (e.g*, tumors)
P. Pearl Chain Effect (Intracellular orientation of subcellular particles, and orientation of cellular and other (non-biologic) particles) Also, orientation of animals, birds, and fish in electromagnetic fields
Q. Miscellaneous Effects
- Sparking between dental fillings
- Peculiar metallic taste in mouth
- Changes in Optical Activity of Colloidal Solutions
- Treatment for Syphilis, Poliomyelitis, Skin Diseases
- Loss of Hair
- Brittleness of Hair
- Sensations of Buzzing Vibrations, Pulsations, and Tickling About the Head and Ears
- Copious Perspiration, Salivation, and Protrusion of Tongue
- Changes in the Operation of Implanted Cardiac Pacemakers
- Changes in Circadian Rhythms
References
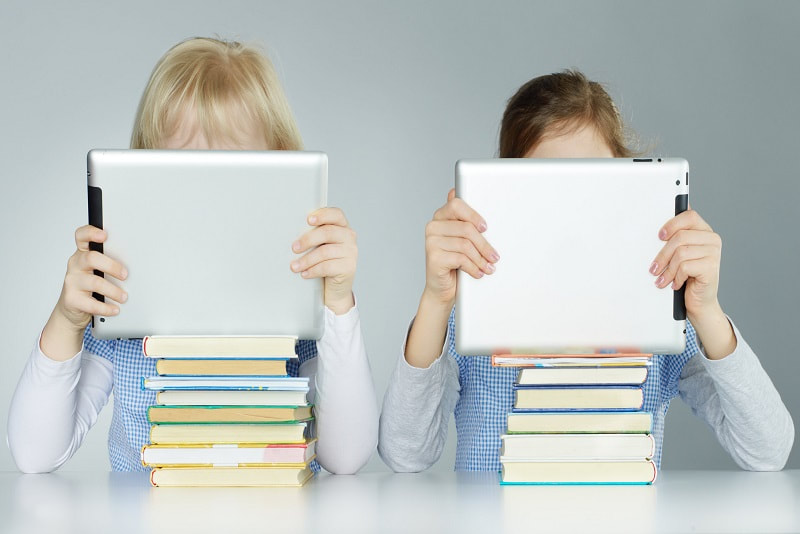
| Undoubtedly, the amount of time that infants and toddlers spend on electronic devices is on the rise. Family ownership of touch screen devices has risen from 7% in 2011 to 71% in 2014 (OfCom, 2014). It is well known that the heavy use of devices, such as tablets, and other electronics, including TV and videogames, contributes to poor sleep. Sleep is the dominant activity of an infant and plays an important role in neurodevelopment and synaptic plasticity. |
For infants and toddlers, touchscreen devices offer an attractive source of stimulation, and their portability allows for a wide range of use across multiple settings. However, the widespread use of devices in this age group has raised serious concerns for parents, educators and policy makers, as the potential impact of touchscreen use on toddler development, such as sleep, remains unknown. In addition, research into the long-term impact of poor sleep during early development remains limited. Yet, findings so far coincide, linking shorter sleep duration to negative developmental outcomes. The majority of studies (~90%) show a consistent pattern linking increased screen time with shorter total sleep time and delayed bedtime. As a result, recent guidelines have recommended screens to be kept out of a child’s bedroom specifically because of the potential impact they may have on sleep (OfCom, 2014).
Given the evidence that:
- media use is linked to poor sleep in older children and adults,
- touchscreen use in infants/toddlers is highly prevalent, and
- sleep plays a prominent role in early cognitive and brain development,
A recent meta-analytic review identified 20 studies in children and adolescents aged between 6 and 19, and found strong and consistent evidence for detrimental effects of portable touchscreen devices on sleep quality and quantity (Carter, Rees, Hale, Bhattacharjee, & Paradkar, 2016). All studies used parent questionnaires, and have reported a significant effect of screen time on sleep: increased amount of TV viewing was associated with parent-reported sleep problems, shorter night-time sleep duration, reduced quality of sleep, and irregular naptime and bedtime schedules, adjusting for known confounds including socioeconomic status (SES).
Using a large scale survey, researchers have started to investigate the relationship between touchscreen use and sleep in infants and toddlers between 6 and 36 months of age. Parents were asked to report on the average duration of their child’s daytime and night-time sleep, the time taken for their child to fall asleep, as well as the frequency of night awakenings, to obtain a comprehensive account of infant/toddler sleep patterns.
The UK-based survey on 715 families, reported that 75% of toddlers between 6 months and 3 years of age use a touchscreen on a daily basis. The researchers found that the prevalence of daily use increases substantially with age, from 51% in 6- to 11-month-old infants to 92.05% by 25–36 months. Among users, daily usage increased with age from 8.53 minutes a day (6–11 months) to 45 minutes a day (26–36 months). The average touchscreen usage in this sample is 24.44 minutes.
There was a significant association between touchscreen use and duration of sleep at night, and sleep onset (the type it takes to falls asleep), with increased touchscreen use associated with decreased night-time sleep, increased daytime sleep and a longer sleep onset. There was no significant association between touchscreen usage and frequency of night awakenings. Results also showed that increased touchscreen use was associated with decreased overall amount of sleep. The researchers concluded that every additional hour of touchscreen use is associated with an overall reduction in sleep of 15.6 minutes.
The blue wavelengths emitted by electronic devices—which are beneficial during daylight hours because they boost attention, reaction times, and mood—seem to be the most disruptive at night. While light of any kind can suppress the secretion of melatonin, blue light at night does so more powerfully. Researchers conducted an experiment comparing the effects of 6.5 hours of exposure to blue light to exposure to green light of comparable brightness. The blue light suppressed melatonin for about twice as long as the green light and shifted circadian rhythms by twice as much (3 hours vs. 1.5 hours). (Harvard, 2015).
It is worth noting that touchscreen use may also have positive effect on some aspects of development. In a recent study of the same sample of infants and toddlers, increased active touchscreen use was associated with earlier achievement in fine motor milestones (Bedford, Saez de Urabain, Cheung, Karmiloff-Smith & Smith, 2016).
Together, these findings emphasize the need for a more in-depth understanding of how to maximize benefits and minimize negative consequences of this modern technology.
References
Toddlers’ Fine Motor Milestone Achievement Is Associated with Early Touchscreen Scrolling. Front Psychol 7, 1108, https://doi.org/10.3389/fpsyg.2016.01108
Carter, B., Rees, P., Hale, L., Bhattacharjee, D. & Paradkar, M. S. (2016). Association Between Portable Screen-Based Media Device Access or Use and Sleep Outcomes: A Systematic Review and Meta-analysis. JAMA Pediatr, https://doi.org/10.1001/jamapediatrics.2016.2341
Cheung, C., Bedford, R., Saez De Urabain, I., Karmiloff-Smith, A. and Smith, T. (2017). Daily touchscreen use in infants and toddlers is associated with reduced sleep and delayed sleep onset. Scientific Reports, 7, p.46104. https://doi.org/10.1038/srep46104
Harvard (2015). Blue light has a dark side - Harvard Health. [online] Harvard Health. Available at: https://www.health.harvard.edu/staying-healthy/blue-light-has-a-dark-side [Accessed 3 Oct. 2017].
Hill, C. M., Hogan, A. M. & Karmiloff-Smith, A. (2007). To sleep, perchance to enrich learning? Arch Dis Child 92, 637–643, https://doi.org/10.1136/adc.2006.096156
Kelly, Y., Kelly, J. & Sacker, A. (2013). Time for bed: associations with cognitive performance in 7-year-old children: a longitudinal population-based study. J Epidemiol Community Health 67, 926–931, https://doi.org/10.1136/jech-2012-202024
Magee, C. A., Gordon, R. & Caputi, P. (2014). Distinct developmental trends in sleep duration during early childhood. Pediatrics 133, e1561–1567, https://doi.org/10.1542/peds.2013-3806
Lam, P., Hiscock, H. & Wake, M. (2003). Outcomes of infant sleep problems: a longitudinal study of sleep, behavior, and maternal well-being. Pediatrics 111, e203–207
OfCom. Children and Parents: Media Use and Attitudes Report. (2014). Available at https://www.ofcom.org.uk/__data/assets/pdf_file/0027/76266/childrens_2014_report.pdf
Wake, M. et al. (2006). Prevalence, stability, and outcomes of cry-fuss and sleep problems in the first 2 years of life: prospective community-based study. Pediatrics 117, 836–842, https://doi.org/10.1542/peds.2005-0775
Archives
May 2024
April 2024
March 2024
February 2024
January 2024
December 2023
September 2023
August 2023
June 2023
October 2022
July 2022
February 2022
January 2022
December 2021
November 2021
October 2021
August 2021
July 2021
June 2021
March 2021
February 2021
January 2021
December 2020
November 2020
September 2020
August 2020
March 2020
December 2019
November 2019
October 2019
September 2019
August 2019
July 2019
May 2019
April 2019
March 2019
February 2019
January 2019
December 2018
November 2018
October 2018
September 2018
August 2018
July 2018
June 2018
April 2018
March 2018
February 2018
January 2018
December 2017
November 2017
October 2017
September 2017
August 2017
July 2017
June 2017
May 2017
April 2017
March 2017
February 2017
January 2017
Categories
All
5G
Adductors
Anxiety
Autism
Ayurveda
Big Pharma
Body
Breathing
Cancer
Cannabis
Carbohydrates
Cardiovascular Disease
Children
Chronic Disease
Cognition
Consciousness
Coronavirus
Covid
Cryotherapy
Depression
Deuterium
Diet
Dietary Guidelines
EMFs
Emotions
Endocrine Disruptors
Environment
Exercise
Farming
Fasting
Fats
Fluoride
Food
Food Like Product
Food-like Product
Forest
Gardening
Genetics
Glyphosate
GMOs
Hamstrings
Healing
Health
Herbalism
Hormones
HRV
Immunity
Infertility
Laughter
Lockdowns
Loneliness
Longevity
Masks
Meditation
Metabolism
Microbiome
Microwave Radiation
Mind
Mortality
Musculoskeletal System
Nature
Neuroplasticity
Nutrition
Omega 3
Omega-3
Organic
Pelvis/Thigh
Pesticides
Physical Therapy
Placebo
Pollution
Positive
Pregnancy
Prevention
Processed Foods
Psi
Quadriceps
Research
Retirement
Salt
Sleep
Spine/Thorax
Spirit
Stress
Sugar
Technology
Touch Screens
Toxicity
Vaccines
Well Being
Well-Being




 RSS Feed
RSS Feed

