|
Olle Johansson, associate professor at the Karolinska Institute (retired Nov 2017, still active), Department of Neuroscience, and head of The Experimental Dermatology Unit, has a long background in the neurosciences and has coauthored – together with his supervisor professor Tomas Hökfelt and many others, including Nobel Laureates – up to the presentation of his doctoral thesis 143 original papers, reviews, book chapters and conference abstracts, a publication record hard to beat! His doctoral thesis at the Karolinska Institute was entitled ”Peptide Neurons in the Central and Peripheral Nervous System. Light and Electron Microscopic Studies”.
Olle Johansson has participated in more than 300 congresses, symposia and meetings as an invited speaker, and with free contributions and as an invited ’observer’ at an additional 200. His studies have been widely recognized in the public media, including newspapers, radio and TV as well as on the Internet, both nationally as well as internationally, and he is a regular interview guest in magazines, journals, tabloids and newspapers, as well as in radio shows, TV programmes and in the Internet-based news blogs and websites. Olle Johansson is a world-leading authority in the field of EMF radiation and health effects. Among many achievements he coined the term ”screen dermatitis” which later on was developed into the functional impairment electrohypersensitivity which recognition mainly is due to his work. He has also been a guest professor as well as adjunct professor in basic and clinical neuroscience at the Royal Institute of Technology, Stockholm. His research group continues to investigate adverse health effects of modern, man-made, artificial electromagnetic fields as well as the functional impairment electrohypersensitivity. The very early introduction of the clinical term “screen dermatitis” was done to explain the cutaneous damages that developed in the late 1970s when office workers, first mostly women, began to be placed in front of computer monitors. Olle Johansson then called for action along lines of occupational medicine, biophysics and biochemistry, as well as neuroscience and experimental dermatology. The working hypothesis early became that persons with the impairment electrohypersensitivity react in a cellularly correct way to the electromagnetic radiation, maybe in concert with chemical emissions such as plastic components, flame retardants, etc., in a highly specific way and with a completely correct avoidance reaction — just as you would do if you had been exposed to e.g. sun rays, X-rays, radioactivity or chemical odors. Nowadays, electrohypersensitivity (EHS) is in Sweden an officially fully recognized functional impairment (i.e., it is not regarded as a disease). Survey studies show that somewhere between 230,000-290,000 Swedish men and women—out of a population of 10,000,000—report a variety of symtoms when being in contact with electromagnetic field sources. To this, one should also add all the current issues regarding the bigger picture: the health effects of electromagnetic fields on the general population, including memory, concentration and learning difficulties, neurological damage and cancer, immune system impairments, fertility issues, as well as impacts on other animals, plants and bacteria. Olle Johansson and his collaborators have, in addition, worked in great depth in areas such as skin diseases, cancer, child delivery, female urine incontinence, oral mucosa diseases, brain and spinal cord morphology, synaptology and chemical transmission, peripheral nervous system-related issues, cardiac function, skeletal muscle function and disease, and connective tissue ripening phenomena. He has published more than 600 original articles, reviews, book chapters and conference reports within the fields of basic and applied neuroscience, dermatoscience, epidemiology, and biophysiology. He has received a number of awards, including the Nokia Consumer Electronics Award, The Grand Environment Award of the Cancer and Allergy Foundation, the SIF Award, Tandvårdsskadeförbundets Pris, and many more. Olle Johansson is – or has been – a member of, i.a., The European Neuroscience Association (ENA), The European Society for Dermatological Research (ESDR), IBAS Users of Scandinavia (IBUS), The International Brain Research Organization (IBRO), The International Society for Stereology (ISS), The New York Academy of Sciences, The Royal Microscopical Society (RMS), Scandinavian Society for Electron Microscopy (SCANDEM), The Skin Pharmacology Society (SPS), Society for Neuroscience, Svenska Fysiologföreningen, Svenska Intressegruppen för Grafisk Databehandling (SIGRAD), Svenska Läkaresällskapet, and the Svenska Sällskapet för Automatiserad Bildanalys (SSAB). Olle Johansson has on-going international scientific collaborations with, i.a., Japan, Belgium, Australia, Brasil, India, Uruguay, Serbia, Germany and USA.
0 Comments
From The Ben Greenfield Podcast:
Jay: "Hello, everybody. It's your beloved sidekick co-host of the Ben Greenfield Fitness Podcast, or at least that's what I like to tell myself at night to help me sleep better. I'm Dr. Jay Wiles. And Ben actually decided to fully turn over the podcast in its entirety to me and rename this podcast to the Dr. Jay Wiles Awesome Extravaganza Podcast. While I am by and large kidding, you are actually stuck with me today as we take a deep dive into all things heart rate variability or HRV. In the health and wellness and longevity sector, HRV has become a metric that has been highly discussed but is still quite misunderstood by many. So, I'm here to clear up the air and give you an in-depth explanation of HRV physiology, the metrics, and practical implications because it seems like every quantifying device nowadays has an HRV measure. And because of this and with my background, I'm constantly inundated with questions about this metric, and what it means, and how we can utilize it, and how we can actually implement it from a practical standpoint. Just so you know, you can find all today's shownotes at BenGreenfieldFitness.com/hrvpodcast. With all that said, let me see if I can set the stage as to why you should even listen to me in regards to the science of HRV and its utilization. Let me give you a little bit of a background on my clinical experience and personal usage of biofeedback. So, when I'm not podcasting, my day job is working as a clinical health psychologist with a specialty in complementary and integrative health, and namely, in psychophysiology or biofeedback. You might already be asking yourself, what is biofeedback? Well, in short, biofeedback is the use of your physiology to enhance self-awareness in order to promote self-regulation. Another way of putting this is that we become more mindfully aware of our physiological response via feedback so that we can inherently change our physiology through numerous techniques. My background is doing this with individuals who are suffering from physiological ailments such as chronic pain, tension-type headaches, migraines, hypertension, or other systemic problems of their physiology. I also see a large array of individuals for more psychological problems such as chronic and systemic stress, anxiety, depression, PTSD, and other symptomology. In the more growing body of research and in my own clinical practice, I'm working with individuals who are looking to enhance peak cognitive and physical performance. I've been working with numerous elite professional athletes and executives that have found HRV training to be the most effective behavioral intervention for enhancing performance. I'm board-certified in biofeedback and heart rate variability biofeedback and I have specialty training in the field of psychophysiology. This means that I've procured a specialized knowledge base alongside practical clinical skills in helping my patients through numerous biofeedback techniques, as well as an in-depth understanding of the bi-directional relationship between our psychological processes and physiological processes. One way or another way to think of biofeedback is to think about it as a learning process, like learning to play a musical instrument, a sport, or even a video game. We perform an action, then we observe the results and then repeat this action throughout the day in an effort to continue to attain the positive result or enhance the result. I've also heard some individuals refer to biofeedback as a psychophysiological mirror that will teach the individual to monitor, understand, and change their physiology. If I had to boil biofeedback down to its most simple terms, we are trying to teach the concept of self-regulation, which would be learning how to control behavior efficiently and immediately without the feedback. I'll get back to this in just a bit, but I wanted to set the stage for the upcoming talk. One of the key features of any biofeedback clinician will be through the teaching of self-regulatory skills and heart rate variability or HRV. Indeed, this is actually the most foundational skill to self-regulation in biofeedback. Within my company, which is called Thrive Wellness and Performance, I work with many different types of individuals ranging from those who are battling with significant stress and fatigue or burnout, or those who are looking to optimize peak performance like many elite athletes and executives. In this role, I provide a comprehensive HRV consultation and individual follow-up HRV coaching sessions to help individuals take back their health and improve overall health outcomes or peak performance. I only have my clients using what I have found to be the top HRV measuring devices and data collection available, which I will talk about later. But after this podcast, you might consider what a biofeedback coach might look like for you on your own personal journey towards health and well-being, longevity, and peak performance. So, today, I want to take a deep dive into the field of psychophysiology, into the field of metrics of heart rate variability, in resonance frequency training, heart rate variability and well-being, performance and recovery, how we interpret data from the wearables that we buy, and some of the pitfalls to devices that provide us maybe with some inaccurate measurement and artefact inclusion. I want this to be a one-stop-shop for all things heart rate variability, a podcast that you come back to when you have a question about heart rate variability. But I must say that there are entire Ph.D. programs in the field of psychophysiology, so we are going to just barely scratch the surface. But for the most part, that will actually look like a deep dive. So, with that said, let's jump on in. I feel like it is necessary to set the stage for why this even matters. In other words, I figured that you would all like some buy-in. From a consumer and a clinician standpoint, I'm normally bought into a topic area when there is vast robust research on that topic area. It's really interesting when you start to peruse the internet and PubMed for HRV studies. As you will see that there were actually minimal studies on this topic about 20 to 30 years ago. But from the '90s until especially the past decade, we have seen exponential advancements in how we practically utilize the important metric of HRV. Indeed, research has demonstrated some significant outcomes as to how we use HRV in predicting cardiac outcomes, especially after a myocardial infarction, which is a heart attack. HRV, over the course of a 24-hour period, is actually the greatest predictor for future heart attacks and is one of the, if not, the most reliable predictors that cardiologists will use. We also see in research how HRV is correlated with increased risk for cerebral vascular accident, which is a stroke, especially after someone has already had a stroke. We can also see a direct link between HRV and sleep, HRV and stress and cortisol production, HRV and depression, HRV and cognitive performance and in sports performance. All of these links and much more have been identified in peer-reviewed journal articles. So, this is just not some unstudied woo-woo metric. We have a lot of confounding data to support our use of this metric for many things. However, I do not want you to think that this is some panacea metric and can be used for any and every outcome. So, what have we found in research in regarding to how we can use HRV as a metric of our physiology? We have found that knowing our HRV and modifying our HRV can lead to improved mental health and well-being. It optimizes our ability to recover and adapt after exercise. It can lead to improved mental and cognitive performance, improved sleep insight into our nervous system and our nervous system-mediated pain, its insight into increased homeostasis of the nervous system that leads to improved stress outcomes, and can be a detection system of dysregulation in the central and peripheral nervous systems. An example of this is that a group of researchers found that individuals with chronic stress-related neck pain had significantly lower HRV scores than the normative population, which was found due to autonomic dysregulation, which I will explain later what that means, after 10 weeks of HRV biofeedback, these individuals were able to significantly increase their HRV which resulted in improved perceived health, increased vitality alongside reduced pain outcomes and improved social functioning. A study performed with physically fit men and women that assessed HRV in the relationship between anxiety and stress and one's engagement in physical exercise found that both men and women that perceive themselves as having higher stress had lower HRV scores regardless of their physical activity. So, while physical activity plays a significant role in HRV modulation, meaning that the more physically fit you are, the higher the HRV unless you are overtraining, emotional or psychological stress likely plays a more significant role in mediating HRV. A meta-analysis was performed in 2014 demonstrated that anxiety disorders are associated with significant reductions in HRV. From a sports performance perspective, an article in the Journal of Sport Science and Medicine in 2014 indicated that we are able to gain accurate insight into recovery via ultra-short-term HRV measurements, anything as low as 60 seconds. HRV has also been found to be associated with aerobic capacity, as researchers have identified, that those with lower aerobic capacity tend to have lower HRV scores. Additionally, those who report as more sedentary have lower HRV when compared to a more active population. And numerous studies have also indicated that a high HRV is associated with better general health due to it allowing the person to better adjust to both internal and external stimuli and that a low HRV is a predictor of cardiovascular disease and metabolic diseases and increases the overall risk for mortality. This does not even begin to scratch the surface but should go to show you that this metric is both highly useful. And I would argue, it is imperative for us to know our numbers and make necessary modifications. I also want to quickly highlight a few studies that demonstrate how we can use HRV biofeedback, which would be the use of strategies to enhance self-awareness and self-regulation of HRV. In the study of scientific literature on HRV, and more specifically on HRV biofeedback efficacy, we must turn to the most trusted organization for determining efficacy, which is the Association for Applied Psychophysiology and Biofeedback or AAPB. They provide a ranking system for HRV biofeedback efficacy from an analysis of outcome studies performed on HRV biofeedback for certain symptoms and disorders. The ranking system goes from level 1, which means that it is not empirically supported, all the way to level 5, which means that it is both efficacious and specific and has been statistically shown to be superior to credible sham therapy pill or alternative bona fide treatments in at least two independent study research settings. From a clinical standards perspective, you really want to stay within the level 3 to level 5 range, which level 4 being kind of where most effective treatments lie. Think of level 5 as saying that there is clear evidence that this is the standard modality for that disorder for treatments. That should always be the first line of treatment. Therefore, this is not seen very frequently. An example of this in the biofeedback world is a neurofeedback for those with ADHD. This is considered a level 5 treatment. Now, what does the literature say about HRV biofeedback for certain disorder sets? Well, there is robust research to support HRV biofeedback as a level 4 practice indicating high efficacy outcomes for depression and anxiety, hypertension which is high blood pressure, pre-hypertension, preeclampsia, IBS or irritable bowel syndrome, and chronic muscle pain. In the performance world, we see HRV biofeedback as a level 3 for optimized performance in baseball, basketball, dance, and in golf. And this is not to say that it cannot be utilized for other performance avenues, but this is where we have the most robust research. Another study in the Journal of Applied Psychophysiology and Biofeedback found that HRV biofeedback is an effective, safe, and easy to learn and apply method for both athletes and coaches in order to improve sports performance. In order to have an understanding of how we utilize HRV practically, we must understand the what and the why of our measurement. In order to gain an understanding of why HRV is important, we must take a dive into the field of psychophysiology. Like I alluded to earlier, psychophysiology is studying the interrelationship or the bi-directional relationship between psychological and physiological processes. We have to think of this relationship as both dynamic and bi-directional in nature. This means that it is constantly changing depending on the state of the organism and communicates in both directions. What I mean by this is that what happens within our psychological processes can influence our physiological processes and vice versa. Let me give you an easy-to-understand example. Let's think about hypertension or high blood pressure. It has been long determined that psychological stress can influence hypertension and cardiovascular disease outcomes. This means that somebody's psychological stress experience can inherently increase blood pressure, which is associated with numerous negative health outcomes. The interesting thing about this process though is that it is bi-directional. This means that as someone experiences an increase in blood pressure, which may not be necessarily due to psychological stressors, this physiological change can increase the anxiety or stress response of the individual. Basically, from an ancestral perspective, physiological changes in blood pressure send communication to the brain that there must be a threat. That is resulting in vascular constriction, increased heart rate and increased blood pressure. Therefore, our limbic system, and more specifically, our amygdala in the brain sends our body and our brain into an action-oriented response so that we can either fight or flee from the threat that's in front of us. This is both a conscious and an unconscious response. Another way that we can view this is through the lens of what is called the psychophysiological principle. This principle states that every change in the physiological state is accompanied by an appropriate change in the mental-emotional state, and this is again conscious or unconscious. And then conversely, every change in our emotional or mental state, both conscious or unconscious, is accompanied by an appropriate change in the physiological state. Again, these interconnected and bi-directional relationships. Yet another example of this is when we think about the role that facial muscle contraction can have an influencing emotion and how emotion can influence facial muscle contraction. So, someone that may get a Botox injection, which would actually paralyze facial muscles to treat wrinkles can actually reduce the intensity of a person's emotional experience. Yes, we have a lot of interesting research on this topic. One thing to remember at the foundation of our physiology is that each and every human being is striving for homeostasis, which is the maintenance of the body's internal environment with healthy physiological limits. A state of homeostasis is synonymous with the body striving for a process called allostasis. So, allostasis is a state of maintenance of stability through change and is a process that complements homeostasis. We achieved this state of allostasis through different mechanisms that anticipate challenges and adapt through behavior, a process of learning and then a physiological change. You can think of high HRV as evidence of our ability to adapt to stressors and maintain homeostasis. When we increase our HRV, this provides us with the ability to move in and out of a parasympathetic and sympathetic state as needed and as quickly and as efficiently as possible. I also refer to this as autonomic fortitude. The ability to shift in and out of a sympathetic and parasympathetic state demonstrates high HRV resilience or high heart rate variability resilience and is less likely to lead to things like adrenal fatigue, chronic stress, overtraining, and will yield better recovery. Unfortunately, the state of homeostasis and allostasis is combated with what we call a state of allostatic load. This is when our physiological, psychological, and spiritual adaptations have been significantly taxed, and now we are experiencing the deleterious effects as a result. You can kind of think of this as a balanced scale. In a state of homeostasis, we are adapting to change and challenge effectively. As we experience stressors and challenges that are too taxing on our physiology such as things like chronic pain, stress, depression, overexertion in exercise, toxic relationships, work stress, financial strain, and so forth, the scales become unbalanced and we can have systemic physiological and psychological problems that will arise. Let's think about this from an ancestral perspective. You may have heard of the comparison of how our ancestors may have experienced rapid, acute, and transient states of high stress such as being chased by a mountain lion while hunting and gathering. But when they return to their homelands, their stress response would come back down to baseline. Therefore, there was an activation of the HPA axis or the hypothalamic-pituitary-adrenal axis, and that resulted in an increase–I should say an acute release of adrenaline and cortisol and other glucocorticoids. These levels which can be highly inflammatory would typically come back down after the perceived threat was mitigated and an increased sense of safety was established. However, in our modern society, one that has us entrenched and engulfed in our work and our perceived worth, we have found ourselves in a constant state of physiological arousal and stress, all of which turns on our fight-or-flight response to perceive threat. In a sense, it's almost like perceiving that the mountain lion is continuously chasing us in our modern society. When this occurs day after day, decade after decade, this is going to take a tremendous toll on our psychological, physiological, and spiritual well-being. That is why it is imperative for us to be continuously self-monitoring and mindful of what we have in our lives and how we live our lives and the potential detriment that this may be causing over time. Physiological states of arousal or the state of fight-or-flight is there for our survival and is much needed. However, at some point in time, we begin to experience this imbalance, which tells our brain that a threat is always going to occur, never shutting off or blunting the fight-or-flight response. And this is why we need to take a deep dive into what helps us maintain balance or allostasis and homeostasis. I think the best framework of HRV training is always through the lens of autonomic balance and psychological and physiological resilience. This turns us to the topic of the central nervous system and the peripheral nervous system. We cannot have a conversation on HRV without a conversation on the central nervous system and the peripheral nervous system. The simple way to think about the two is that the central nervous system consists of the brain and the spinal cord, while the peripheral nervous system consists of all the nerves that run out of the central nervous system and innervate every area of our body. You can think of this as all of our organs, all of our limbs, and the skin. Therefore, these two are interconnected and have a bi-directional relationship. The peripheral nervous system has two distinct branches. These are the somatic nervous system and the autonomic nervous system. You can think of the somatic nervous system as being in control of the skeletal muscles and will transmit different somatosensory information back to the central nervous system. Our autonomic nervous system regulates certain aspects of our physiology that occur automatically. These would be things like regulating our cardiac and smooth muscle or heart functioning and respiration. We can then divide the autonomic nervous system into three main systems or three main branches. These are the sympathetic division, the parasympathetic division, and the enteric division. In the study of biofeedback, and specifically heart rate variability, we are focused predominantly on the autonomic nervous system, and more specifically, the parasympathetic and sympathetic branches or divisions. Now, let's break down both of these divisions as there tends to be some confusion in this area. I will start by discussing the sympathetic nervous system. This is the division of our nervous system that readies us for action, challenge, and will regulate the activities that expand or expend energy. The sympathetic nervous system is in direct connection with our endocrine system and regulates certain hormonal responses. This is what helps us to respond to threats to our safety through mobilization, the fight-or-flight response, or a process of active avoidance. In comparison to the parasympathetic response, which I'll speak about later, the sympathetic nervous system responds more slowly and for longer periods of time. For instance, it takes the parasympathetic vagus system less than a second to respond, while the sympathetic nervous system takes about five seconds or greater. From a physiological standpoint, sympathetic nervous system cells are found in the gray matter of the thoracic and lumbar segments of the spinal cord. The sympathetic nervous system also directly innervates our adrenal medulla, which is the central portion of the adrenal gland. The adrenal medulla is actually responsible for the release of the neurotransmitters, epinephrine and norepinephrine when they are stimulated. In response, this reinforces the sympathetic activation of our visceral organs. When we release these neurotransmitters due to a stimulated stress response, this will increase muscular blood flow and will convert stored nutrients into glucose to power skeletal muscle contraction. Basically, this causes the release of neurotransmitters that can put us into action. When the sympathetic nervous system is activated, this can be considered a fight-or-flight response. When this happens on a short-term or acute or transient state, this can be quite effective in increasing performance, helping us to escape a threat, or helping us to fight a threat. There is common misperception and misconception that the sympathetic nervous system is detrimental due to the release of glucocorticoids and stress hormones. We have to keep in mind that while chronic states of glucocorticoid secretion and stress hormone secretion can be a detriment to the body. Transient and acute activation of glucocorticoids and stress hormones can be quite beneficial. If you haven't done so already, I would highly encourage you to check out Dr. Craig Koniver's podcast that he did with Ben on cortisol and read one of the most–and I would also encourage you, I should say, to read one of the most thorough explanations on stress adaptation in a book called “Why Zebras Don't Get Ulcers” by Dr. Robert Sapolsky. From a physiological standpoint, there are many things that occur in our biology when our sympathetic state is kicked into high gear. In this state, we see a dilation of the pupils, an increased heartbeat, relaxed airways, inhibition of activity with the enteric nervous system, which is our gut. Of course, there is the secretion of epinephrine and norepinephrine, and then we also have a relaxed bladder. This is why someone might urinate on themselves if the sympathetic nervous system is activated extremely quickly in a tense situation. Think about it this way. When we perceive a threat in our environment, our body and brain directly communicate with one another and can shut off certain systems depending on what we need to take on the perceived threat. For instance, in a stress response, we have no use for reproduction. So, our reproductive organs are shut down. We do not want to expend blood in the gut to break down food because we do not need it and we need it elsewhere, like in our lungs, in our heart, and in our brain. And therefore, we deactivate our digestive systems. Now that we have a better understanding of the sympathetic nervous system, let's talk about the parasympathetic nervous system, which works in tandem with the sympathetic nervous system. I may need to also clarify that when we talk about the concept of autonomic balance, we are talking about a balancing of the two nervous systems. There's this notion that the sympathetic nervous system is the villain and the parasympathetic nervous system is the hero. This indeed is a fallacy and is a misunderstanding of the complex interrelationship between both divisions of our autonomic nervous system when in fact, it is a balance of these two divisions that is going to increase heart rate variability and demonstrate better overall health outcomes. You wouldn't want have an overly active parasympathetic nervous system just like you would not want to have a chronically activated sympathetic nervous system. I will get back to more on this later, but for now, let's discuss the parasympathetic nervous system and division of the autonomic nervous system. The parasympathetic division helps to regulate activities that will naturally increase the body's energy reserves. When you think about this branch of the nervous system, we might consider it like the inhibitory reactor, whose attendance is to pull us towards homeostasis. That's when we experience that state of allostatic load that I was talking about earlier. The other thing that you might already be aware of that you will want to pair with the parasympathetic nervous system is with our tenth cranial nerve, which is referred to as the vagus nerve. The parasympathetic nervous system cell bodies are found in the nuclei of four of the cranial nerves, but also in the sacral region of the spinal cord. We see this in the vagus nerve, which innervates many of our primary organs such as our heart, our lungs, our esophagus, the stomach, pancreas, liver, and the intestines. This means that it has direct communication to affect change in these organ systems. Its main chemical messenger is a neurotransmitter called acetylcholine. While acetylcholine can act as an excitatory neurotransmitter in certain parts of the brain such as exciting the basal ganglia for movement, acetylcholine actually acts predominantly as an inhibitory neurotransmitter within the parasympathetic division. When I say that it acts as an inhibitory neurotransmitter, this means that it results in reduced firing of nerve cells, which is going to be in direct opposition to the sympathetic activation that may be occurring. The parasympathetic nervous system is primarily mediated by the vagus nerve and has been referred to as the rest and digest branch of the autonomic nervous system. Some predominant researchers, particularly Dr. Stephen Porges, has found that the vagus nerve is mediated by a sense of safety and security. And I'll talk a lot more about this later. One way I like to think of this is that when we can intentionally create a safe space physically and psychologically, we are going to exhibit action in the vagus nerve. Another example of this would be how breathwork can modulate the parasympathetic nervous system and increase HRV on an acute level. If we take the time and we are able to take an intentional slow diaphragmatic breath, this is communicating to both our mind and body that we are in a safe place and we are able to engage in this behavior. This may not occur, let's say, if we are being chased by a mountain lion. For our survival, we do not want to pump the brakes and give our mind and body the message to relax in that case. It is a time where we need all of our resources and faculties to get out of the situation. One more thing that I will say about the parasympathetic nervous system is that it indeed works as a brake to the sympathetic nervous system. You can think of it as working similarly to a car. When the car is put in park, it will–or I should say when the car is put into drive, it will automatically accelerate without you having to press the gas pedal. This natural acceleration is like your sympathetic nervous system. It's always on. You're never going to be able to turn it off completely, but that's a good thing. It is scanning the environment for threats, which keeps us vigilant and keeps us safe. Now, you can floor the gas pedal and that would be like activating the sympathetic nervous system, and this is helpful in the immediate situations, but would be detrimental and result in a loss of fuel in a very long-term period. Whereas the parasympathetic nervous system works as that brake. It slows us down. The brake is leveraging the vagus nerve as the primary mediator. So, stimulating activation of the vagus nerve results in a cascade of beneficial psychophysiological outcomes when it's done at the right time. The last aspect of psychophysiology that is immensely important in the relationship between HRV is the process that we refer to as the baroreflex mechanism. One of the ways we maintain homeostasis is through a fully functional baroreflex response or baroreflex mechanism. This is actually a negative feedback loop that helps us to maintain homeostatic or stable blood pressure. Not only is this paramount to our survival as a species, but is also one of the primary areas of focus for heart rate variability biofeedback. This is because the aim of HRV biofeedback, which again is self-regulation of HRV, is to exercise the baroreceptor reflex to enhance homeostatic regulation and executive functions. The pathway is to modify our physiology by exercising the baroreflex in order to restore the dynamic autonomic balance of our nervous system. So, let me break it down in its most simplistic forms. Baroreflex or baroreceptors are these blood pressure receptors that are located in the aortic arch and the internal carotid arteries, which contribute to overall HRV. These receptors are referred to as stretch receptors or detection receptors. When you inhale, your heart rate is going to naturally increase. This will result in a rise in blood pressure about five seconds after this heart rate is increased. This increase in blood pressure will cause a stretch in the carotid arteries alongside the aortic arch causing the baroreceptors to fire action potentials at a very rapid rate. This rapid firing is sent through your tenth cranial nerve which is the vagus nerve, and the ninth cranial nerve which is the glossopharyngeal nerve to a part of our hindbrain referred to as the medulla, and more specifically, the nucleus of the solitary tract. This area of our brain will receive the signaling from the baroreceptors and will then subsequently activate the parasympathetic nervous system, which is, of course, our rest and digest branch of the nervous system. This process will also inhibit the sympathetic nervous system from signaling. The signaling of the parasympathetic nervous system will then result in a release of the neurotransmitter acetylcholine, which I said is again an inhibitory neurotransmitter, which inhibits and works on our pacemaker cells found in the sinoatrial node or the SA node of the heart. This will result in vasodilation, which is the opening of blood vessels to allow the increase of blood flow and will result in subsequent decreased blood pressure. Because of this mechanism, the heart rate will be brought back down to stable functioning. So, conversely, when someone has a sudden drop in blood pressure, the decreased blood pressure will then signal the medulla to inhibit the parasympathetic nervous system and will initiate action in the sympathetic nervous system. The sympathetic nervous system will begin to release norepinephrine and epinephrine, which will act again on that same area, the SA node of the heart to increase heart rate and will result in vasoconstriction, which will increase blood pressure. So, all in all, the baroreflex response is a sudden response and is a response to sudden changes in blood pressure that helps our bodies to regulate the impact of everyday activities and changes in emotional states. If, for instance, these things are not well-managed and result in hypertension, what the body will do is it will actually adjust and begin to see these elevations as the new normal levels because the body is always looking to adapt and create a new set point and the thermostat that we call homeostasis. The end result is that yes, you have high blood pressure, but you also have lower HRV. This is why modulating HRV by exercising our baroreflex and signaling the parasympathetic nervous system has a vast importance. Alright. So, now, it's time to link everything that we've discussed thus far into the topic of heart rate variability or HRV. In its most simplistic form, HRV or heart rate variability refers to the beat to beat variation in the time intervals between heart contractions. When we think about the oscillations of a healthy heart, they are actually quite complex. The healthy heart is typically seen as one that can rapidly adjust to sudden physical and psychological challenges. HRV is absolutely crucial to our overall health, resilience, and may be increased through different behavioral activations and practices like effortless breathing, exercise, compassion practices, and mindfulness practices. Within the research field of HRV, we define HRV as the fluctuation in time intervals between each adjacent heartbeat. Like I mentioned earlier, this is referred to as an interbeat interval and is typically measured in milliseconds. If you have any device that measures heart rate variability, it is probably utilizing a software algorithm that is probably calculating the interbeat interval between successive R spikes or the peaks of blood volume pulse. An R wave or an R spike would be read via an ECG or an electrocardiogram output, and this is the spike in electrical activity due to the depolarization of the ventricles of the heart. From an electrical standpoint, every heartbeat starts at what's called the SA node that I mentioned earlier, the sinoatrial node, which is also considered the heart's pacemaker. Interestingly enough, the natural pace of the heart without a fully functioning SA node is around 100 beats per minute, which by most standards, clinically, would be a form of tachycardia or a fast heartbeat. It is the SA node that helps to keep the heart on pace. The electrical signaling is what results in a cascade of complex events, which we call heartbeat. When we are measuring HRV on a majority of wearable devices, the algorithm is looking at peaks and blood volume through a device called photoplethysmography or PPG. These typically utilize infrared light sensors that shine through the skin and detect fluctuations in blood volume via the heart changes and pulse. Either measure that you're examining, one of the things that we know about the heart is that it is not a metronome. Indeed, if we see a heart that has consistent times in the interbeat intervals, we know that something is incredibly wrong with this individual's cardiovascular or nervous system. This is because at the heart of HRV is resilience. What I mean by this is that HRV's highest representation as a metric is on how resilient your physiology is to change. We have to keep in mind that we have trillions, yes, trillions among trillions of physiological processes occurring every moment within our biology. This means that the heart has a lot to keep up with. If the heart starts to regulate itself, kind of like a metronome, it is essentially the heart crying out for help, and sang aloud, I have no other choice but to regulate something amidst chaos. This sounds a little bit counterintuitive as it would seem like homeostasis would mean that the heart rate or heart rate variability would be consistent, but this is in fact very far from the truth. What we know from research is that heart rate variability is one of the most studied and highly accurate measurements and metrics for assessing the stress response, cardiovascular-related mortality and mobility and performance recovery. So, what are the sources of HRV? So, HRV is produced by two distinct overlapping processes. First is the concept of autonomic balance, which we talked about earlier. But to remind you, that is the complex relationship between both the parasympathetic and sympathetic divisions of the autonomic nervous system. The other are the regulatory mechanisms that control heart rate via a few processes. These include a process called respiratory sinus arrhythmia, the baroreflex, and rhythmic changes in vascular tone. I've already discussed the baroreflex. So, now let's talk about respiratory sinus arrhythmia or RSA. So, RSA is an extremely important concept in HRV regulation and optimization. We can actually use this process to manipulate our overall heart rate variability. You can do this. Anyone can do this. Respiratory sinus arrhythmia is the speeding and slowing of the heart across the breathing cycle. When we slow our breathing pattern down, we see a couple of things occurring physiologically. First, as we inhale, our heart rate will naturally incline to its peak. And when we exhale, and as we exhale, the heart will lower to its trough point. This makes sense if we think about it. As we are inhaling, the body is receiving usable oxygen to be delivered throughout the body into the brain. Therefore, the heart needs to utilize this immediately and will increase its cardiac output for the delivery of oxygen and gas exchange throughout the body. As we increase RSA, this rhythm, through low and slow breathing, we can actually stimulate vagal tone and, which again that's the vagus nerve, and we can lower blood pressure through the baroreflex mechanism. So, now let's shift to the metrics of HRV. It's likely if you have any HRV measuring devices that you have seen that this device calculates HRV through a means of SDNN or RMSSD, or it may measure low-frequency or high-frequency, and it's likely that you have no idea what this means or have had to look it up and still do not understand what it means. I want to clarify these measurements and give you my opinion on what you should be looking for and how to base your numbers on the norms and your own baselines. First of all, we need to differentiate between the types of HRV measurement. There are two predominant types of measurements that I'm going to talk about today. One is the time domain measurement, and the other is a frequency band or frequency domain measurement. Both of these are looking at different metrics. So, now, let's start with the time-domain measurement. When I speak about time-domain HRV measurements, I'm talking about a measurement that is calculated based on time intervals between each adjacent heartbeat. A little while ago, I mentioned how the heart does not function like a metronome. There are different time intervals in between each adjacent heartbeat where one heartbeat to another may be 800 milliseconds and the next adjacent heartbeat may only be 750 milliseconds. This shows variability in the time intervals. The difference between those two that I just mentioned is 50 milliseconds. And so therefore, we can say that there was 50 milliseconds of variability between the two sets of heartbeats. Now, as with anything in science, we're not going to base our HRV score on two sets of interbeat intervals as this is much too small of a sample size to give us any relevant or usable data. You would never base it on that. This is why we have to assess HRV over a period of time intervals. The amount of time needed for different calculations is going to vary depending on the type of time domain index you are interested in examining. For instance, the two primary usable time domain indices that we see most commonly are SDNN and RMSSD, and I'm going to explain the difference in just a minute. These both require different time domains to get accurate measurement or usable data. So, SDNN, for example, requires a minimum of five minutes, but in reality, it's really only clinically relevant if we assess over 24-hour period, and I'll explain more about what I mean about that in a second. While the RMSSD metric has actually been shown to provide valuable interpretations at as low as 10 seconds, 30 seconds, and 180 seconds. However, like SDNN, RMSSD is most accurate over a five-minute period. So, it will be important for you to know what you are calculating and what timeframe you need to measure or to provide or ensure accurate measurement. So, let's dive into the primary time domains. We will start with what is considered the gold standard of HRV measurement, which is SDNN. So, SDNN stands for the standard deviation of the interbeat intervals of normal sinus beats, which is measured again in milliseconds. Remember that this is measuring normal sinus beats and not artifact. This is one of the things that really irks me more than others is that we have a lot of devices that use the SDNN algorithm but do not remove artifact beats, which are essentially like ectopic beats or false or error beats due to things like movement, electrical interference, or changes in lining. And when that happens, you have data that's fairly void and unusable. And actually, technically, you cannot say that you are calculating SDNN if you do not remove artifact. That would actually be another metric called SDRR. So, unfortunately, many devices that calculate SDNN either do not have this artifacting built-in or it is based on very poor removal resulting in fairly inaccurate HRV data. I'd say that I'm quite the HRV snob, so it's something that I always look into. A similar measurement, which I just mentioned earlier, is SDRR, and that calculates all the sinus beats, even abnormal or false beats. The problem with this measurement though, which in a lot of our wearables, is that you can have abnormal beats that reflect cardiac dysfunction or even noise, but it will masquerade as HRV. So, I never use the SDRR data. But back to SDNN, when we talk about the standard deviation of interbeat intervals, what we are talking about is how much on average does each beat differ from the next. The reason this is considered the gold standard of HRV measurement is because it has been found to have contributions from both the sympathetic nervous system and parasympathetic nervous system. So, we can get full insight into our autonomic response with this measurement. Like I mentioned before, SDNN is most accurate when it is assessed over 24 hours than during short periods because the longer periods can provide data about cardiac reactions to a great range of environmental stimulation, or lack thereof in the case of sleep. It is also the 24-hour recordings that allow us to assess the sympathetic nervous system contribution to SDNN. For assessing cardiac risk, SDNN is almost always used and can be a valuable predictor of both morbidity and mortality. And looking at 24-hour recordings, an SDNN less than 50 milliseconds has been demonstrated in those classified as unhealthy. Those with 50 milliseconds to 100 milliseconds is a classification for compromised health, and 100 milliseconds and above is considered a healthy individual from a cardiac standpoint. When we look at heart attack survivors, those who have had a higher classification had a greater risk of living–or sorry, I should say a greater probability of living during a 31-month follow-up period. One study demonstrated that individuals with an SDNN greater than 100 milliseconds had a 5.3 times lower risk of mortality at follow-up than those with values less than 50 milliseconds. We can actually correlate the SDNN metric with other frequency domains that I will discuss later. SDNN is correlated with the ultra-low-frequency band, the very low-frequency band, and the low-frequency band. Now, let's turn to another time-domain index for HRV. And for short-term time-domain evaluation, it's probably my most preferred measure, which is the RMSSD metric. So, RMSSD is the root mean square of successive differences between normal heartbeats. And now that I have sufficed in spinning your heads, let me explain it. In order to calculate this value, we must calculate each successive time difference between adjacent interbeat intervals in terms of milliseconds. Then each of these values is squared and the result is then averaged before the square root of the total is obtained. Now, that is a lot of what we do in research. So, I wanted to give you that equation, but for the sake of practicality, it may not be necessarily that important. The measurement is mediated or provides us insight into the workings of our parasympathetic nervous system and is highly correlated with the high-frequency band. We actually know that RMSSD is more influenced by the parasympathetic branch than SDNN. While a five-minute measurement is the gold standard for RMSSD, you can get usable data in ultra-short-term domains that I mentioned at the beginning of this podcast. This makes it really good as an on-the-go measurement. One thing that I like about RMSSD is that it is not mediated by respiratory sinus arrhythmia like SDNN is. What I mean by this is that with SDNN, you can affect change in this number by taking those low and slow diaphragmatic breaths. Whereas RMSSD does not appear to be mediated by respiration or slow breathing and may provide more insight into recovery as it is primarily assessing tonic or relaxed or static HRV. So, if you want to gain insight into your recovery and remove the effects of respiration to assess non-manipulated HRV, RMSSD is the way to go. So, that's the one I use for recovery. This is one of the best measures of vagal tone due to the lack of manipulation of respiration. This is why I actually like the use of the Oura ring to assess HRV at night while I sleep, but more about that later. Another one that is used quite frequently and is very easy to assess in the HRV time domains is something called HRV amplitude. This is a very simple measurement that is an average of the difference between the highest and lowest heart rate during each respiratory cycle. So, remember, RSA or respiratory sinus arrhythmia is the fluctuation of heart rate from the start to the finish of a breath cycle. Normal RSA occurs when you inhale and your heart rate increases, and when you exhale, your heart rate decreases. If you subtract the peak heart rate in the cycle and the lowest heart rate at the end of the cycle, this will provide HRV amplitude. So, this is not a great index of vagal tone as it can be mediated by respiration. This measure normally depends on both age and fitness level. As we age, HRV, and especially amplitude, tends to go down. The more sedentary we are, the lower the amplitude we are likely to have. In elite athletes, I have seen amplitude as high as 50 to 60 beats per minute. This means that at the start of their exhale, their heart rate is at 50 beats per minute, and at the peak of their respiratory cycle, the heart rate gets up to about 100 beats per minute, and then comes back down to 50 beats per minute on the exhale. Whereas I've seen some patients with cardiovascular disease or chronic pain go from 70 beats per minute to 73 beats per minute, which would only be an amplitude or heart rate variability of 3 beats per minute, which is extremely low. This is where we might warrant some HRV biofeedback. Now that we've talked about some of the predominant time-domain indices, let's move towards frequency domains as these have become quite popular in recent years. Let's first differentiate between time domain and frequency domain measurements of HRV. As a recap, when we think about time-domain indices, this quantifies the total amount of heart rate variability. Whereas frequency domain measurements will quantify the distribution of absolute or relative power into different frequency bands. Absolute power can be expressed in terms of millisecond square divided by cycles per second, and relative power is expressed as the percentage of total HRV, or we refer to this as normal units. In frequency domain HRV measurement, power is expressed in normal units by dividing the absolute power for specific frequency band by the sum absolute power of the low-frequency and high-frequency bands. When we calculate power in normal units, this will also allow us to directly compare the spectral distribution of HRV bands for two different people. Now, all of this is referring to the algorithms that constitute frequency domains or power. But for the sake of our discussion, I want to see if I can now simplify all of this crazy complex information. Let's think about an EEG. So, this actually measures individual brainwave domains. For instance, when we have the slowest brainwave, which is associated with sleep, this is called delta waves. The next band or wave band would be theta, then alpha, and then beta. This is an example of how the process of something called a power spectral analysis can separate brainwaves into their own component rhythms that operate within different frequency ranges. We can do the same actual thing–we can do the same thing, I should say, with HRV. A great way to think about this is to think about shining a light through a prism. The prism will reflect white light into its component wavelengths. So, through a mathematical process called the fast fourier power spectral analysis, we can break HRV when at time domain into its component wavelengths. And into each of these wavelengths, we can give a little bit more insight into our autonomic functioning. Before I begin talking about each of these wavelengths or frequency domains, I want to know that there is still some controversy regarding the autonomic contributions to some of these domains since these measurements will kind of profoundly vary with testing conditions. One thing to note about HRV frequency bands similar to that of EEG bands is that we are predominantly concerned with the dominant band at the time of assessment. This is because we have activations of all bands at any given time, but we are concerned with what is mostly activated or is considered the dominant domain. Think about EEG again. If you are to hook yourself up to an EEG, you might have one band that is more dominant than the others. So, say, for instance, theta, but this does not mean that you are producing zero delta, zero alpha, or zero beta. Indeed, you are making all of them at once, but one may be more predominant as a wavelength at that time. It's a common mistake for many individuals to believe that we are only making one set of brainwave frequencies within the area of the brain that we are studying. So, I hope that this helps to clarify that just because–like the brain, the heart is not simply making one frequency to the void of others. Yes, it may be presenting with one dominant frequency, but we are still able to measure all of the others as activated during this period. With all that said, there's still a lot of great data that we have gotten from studying frequency domains that I believe are very important for us to cover. We'll start off with the ultra-low-frequency band, which are oscillations less than 0.003 Hertz. This is a frequency band that can be only measured within a 24-hour period. For this band, there is no consensus regarding the mechanisms that generate its power, but we do know that it is indicative of very slow-acting biological processes. Some researchers believe that circadian rhythms may be the primary driver of the ultra-low-frequency band. There's also belief that core body temperature, metabolism, and other bodily systems over a long period of time may contribute to this frequency. There is also disagreement about what branch of the nervous system contributes to the ultra-low-frequency band. So, for the sake of our discussion, until we learn more about this unique frequency band, there's not much more that I want to say about its utilization. So, now, we move to the very low-frequency band, which is the frequency band that ranges from 0.003 Hertz to 0.04 Hertz. In order to record the very low-frequency band, we must record at least five minutes' worth of data. But 24 hours is actually considered the gold standard. Through research, we know that any low values on a 24 clinical HRV recording can predict greater risk or adverse outcomes. However, what we have found that is the very low power frequency is more strongly associated with all-cause mortality than the low-frequency or high-frequency domains. Therefore, as we gain more research on this band, we are finding that the very low-frequency bands may be quite fundamental to health. When researchers have studied very low-frequency bands, band power, they have found that low power in this domain has been associated with rhythmic death, high levels of inflammation, and lower levels of testosterone. They've also found that parasympathetic nervous system activity may contribute to very low-frequency band power since parasympathetic blockade almost completely abolishes it. When researchers have blockaded the sympathetic nervous system, this does not appear to affect the very low-frequency power. So, from a practical standpoint, especially when measuring over 24 hours, this is not a band of the frequency domains that we want to have low. This brings us to some of the more well-known frequency bands. And the first one I want to discuss is the low-frequency band, which ranges from 0.04 Hertz all the way up to 0.15 Hertz. This band requires a minimum recording of two minutes, while this is one of the more commonly used in many phone-based applications and biohacking wearables. Interestingly enough, there is actually disagreement regarding the sources of activity within this band. Formally, this region or frequency band was called the baroreceptor range because it does mainly reflect baroreceptor activity under resting conditions. It appears that low-frequency band power may be produced from both the parasympathetic and sympathetic nervous system and is regulated via the baroreceptors that regulate blood pressure. One of the things that we know about the low-frequency band is that the sympathetic nervous system does not appear to produce rhythms much above 0.1 Hertz, while the parasympathetic nervous system can be observed to affect heart rhythms down to 0.05 Hertz. When we engage in slow respiration rates and slow breathing, vagal activity can easily generate oscillations within the low-frequency band. This is why you hear a lot of individuals say, “To train within the low-frequency band.” Indeed, this can actually be quite simple for most individuals. Breathing at a rate of six breaths per minute has been found to put most people within this low-frequency domain. We might even say that this domain can be representative of autonomic balance. There's a process of breathing, which we call resonance frequency, which is a common biofeedback tool that places the individual within this range. This is something that I'm going to talk about in a little bit when I get into common modalities for enhancing HRV. But for now, know that this is a common range to train autonomic balance in vagal tone. Within the Institute of HeartMath, they actually have identified the single high amplitude peak within this low-frequency domain, and more specifically, at the 0.1 Hertz mark to indicate what they call a state of high coherence. From this model standpoint, coherence is when the heart, mind, and emotions are energetically in alignment and in cooperation. They've identified coherence as when we increase synchronization and harmony between the cognitive emotional and physiological symptoms, which results in efficacious or efficient and harmonious functioning. The idea of the HeartMath Institute and their wearable technology such as their emWave2 and the Inner Balance is to increase heart rate variability and coherence through paced breathing and visualization. The last frequency band and domain that I want to discuss today is the high-frequency band. This is found between the 0.15 to 0.40 Hertz and requires a recording of at least one minute. The high-frequency band can reflect parasympathetic activity, and we also refer to this as the respiratory band because it corresponds to the heart rate variations related to the respiratory cycle. As you may recall, these phasic heart rate changes are known as RSA and may be a pure index of cardiac vagal control. What I should say too, when you inhale, the heart rate is going to accelerate, when you exhale, the heart rate is going to slow. So, when we inhale, our cardiovascular centers will inhibit vagal outflow resulting in the speeding of the heart. And when we exhale, this will restore the vagal outflow and slow the heart due to the release of acetylcholine. When there is total vagal blockage, this will virtually eliminate all of the oscillations found in the high-frequency band and will reduce the power range and the low-frequency band. We see a high correlation between the high-frequency band and the RMSSD time-domain band. When individuals have high-frequency band power, it's correlated with an increase in stress, in panic, in anxiety, and in worry. And it's still important for us to remember that high-frequency power and RSA does not represent vagal tone. Keep in mind that high-frequency power and RSA is very easy for us to manipulate by slowing our respiration rates. A study done in 2017 demonstrated that if you slow your breathing to six breaths per minute, you should observe increased heart rate fluctuations compared with 15 breaths per minute, which is the average human breath rate. It is during this time that the mean heart rate should not appreciably change because vagal tone did not decrease. This is an example of how high-frequency power can index vagal modulation of our heart rate, but it does not represent vagal tone. Another common index for frequency-domain measurement and power is something called the low-frequency to high-frequency ratio. The intent here is to estimate the ratio between sympathetic nervous system and parasympathetic nervous system activity. This measurement is seen typically in wearables like the Polar chest strap and the Elite HRV app. The assumption here for the low-frequency to high-frequency ratio is that low-frequency power may be generated by the parasympathetic nervous system, sympathetic nervous system, and baroreflex mechanisms while the high-power band is produced by the parasympathetic nervous system. So, in this model, a low, low-frequency to high-frequency ratio will reflect parasympathetic dominance. This might be seen when we conserve energy and engage in the tend-and-befriend behaviors. You might consider yourself to have low autonomic arousal and be quite relaxed when this ratio is low. So, to contrast this, when we have a low-frequency to high-frequency ratio, this may indicate sympathetic dominance, which occurs when we engage in the fight-or-flight behaviors or form of parasympathetic withdrawal. One thing to keep in mind about this from a research perspective is that brief recordings of the low-frequency to high-frequency ratio are a little controversial as short-term measurements tend to be poorly correlated with 24-hour values. So, it's in my opinion that examining the research that a five-minute resting baseline of the low-frequency to high-frequency ratio may not be our best estimate of autonomic balance. So, with all of this information on the different frequency bands, how might I use them both personally and clinically? Well, first, you must assess your intent on measuring the frequency domains. So, for instance, am I doing more meditative or resonance frequency training to, in a sense, manipulate HRV so that I can experience an increase in vagal tone or relaxation response? Or am I using it for examining recovery? Depending on my needs for the assessment, I may be examining these numbers from different lenses. Let's take the first example and break it down. Again, I'm going to talk about the concept of resonance frequency training in a few minutes, but if I were utilizing heart rate variability for relaxation, reducing distress, or a way to enhance meditative practices, I would be looking to increase the low-frequency band and integrate what we refer to as coherence. Increased low-frequency band will indicate enhanced vagal activity and activation of the parasympathetic nervous system and autonomic balance. Whereas I would not want to manipulate breathing and respiration such as breathing at my resonance frequency rate if I were assessing overall recovery. This is because manipulating breath rate will almost certainly change your HRV scores. One of the things that I'm most consistently asked about are norms. So, it makes sense to ask this question as we want to be able to provide a basis for comparison for HRV numbers. If you look at any website where there is HRV discussion, there are always individuals posting their HRV data and asking, is this low? Is this normal? and so forth. I want to be able to answer some of these questions here, but please know that we never utilize HRV scores as a means to diagnose. Also, as you have also inferred, HRV changes quite frequently and should not be a metric that you take once and then try to make any type of conclusion. Also, like many other biometrics that we quantify, HRV is one that it's great to have a consistent baseline and then work on training that number in an upward direction. Well, many questions come my way regarding low HRV. I'm also asked questions about high HRV and whether or not this can be problematic, and I'm going to speak about this as well. But let's turn to HRV norms to see if I can dispel some myths and highlight some potential goals. I've already mentioned before that when looking at the marker that is considered the gold standard, which is SDNN, from a cardiac functioning standpoint, we see that happening with a 24-hour recording. Those with less than 50 milliseconds of HRV are considered unhealthy, and those with an HRV from 50 to 100 milliseconds are considered to have compromised health, while those with HRV over 100 milliseconds are considered healthy from a cardiac standpoint. A couple of things on this. First, please remember that these are just standards for cardiac outcomes and are not made to be used from a diagnostic standpoint. There are plenty of other pieces of information that we need in order to notate whether someone has a healthy cardiovascular system or an unhealthy one, not just HRV alone. While this is the gold standard metric, we are all about integrating data. So, second, if you already heard me mention these numbers and you're freaking out because your Oura ring is telling you that you're in the 30s or 20s, you're actually freaking out for no reason. The Oura ring uses the RMSSD data and not SDNN. Lastly, I don't know many individuals who are recording 24 hours with the SDNN marker other than those who are wearing like Holter monitors for a long period of time. So, from a quantification standpoint such as the utilization of wearables, many of us are just really not collecting this data. And this is predominantly clinical. So, I just wanted to provide these numbers initially, as again these numbers are the gold standard for cardiovascular outcomes. Well, there are many different types of time-domain measurements that we mentioned before like the SDNN and SDRR and RMSSD. There are also other ones like the SDANN index. There's the NN50, the PNN50 and so on. But these are not typically ones that you're going to cross paths with unless you're doing clinical biofeedback with a specialist like myself. A majority of these wearables or technology that you would utilize from a consumer standpoint are either going to be via SDNN or RMSSD. That is why I'm going to devote much more time to these. There have been numerous studies looking at identifying norms, but the largest study ever done on normalizing data was done compiling 44 selected studies, which examined over 21,000 adult participants. Some things to keep in mind. First, this analysis included three large populations with a minimum age of 40, which may actually end up explaining their comparatively low HRV scores and can't be generalized to yourself if you're under 40. Well, yeah, because that's the minimum age. And they also didn't factor in other types of variables, things like age, gender, socioeconomic status, and so forth. But here is what they found. The researchers of this large comparative study found the average mean SDNN score in milliseconds to be 50 milliseconds with a standard deviation of 16. They found the average RMSSD to be 42 milliseconds with an average standard deviation of 15. They found the low-frequency to high-frequency ratio in terms of millisecond squared to be 2.8 with a standard deviation of 2.6. Another interesting study that was done in 2015 looked at 2,000 subjects between the ages of 25 to 74. Now, these were noted as healthy adults as they included anyone with cardiac arrhythmia, diseases, those who were on significant medications or pregnant. However, I tend to utilize this information as a basis for my own norm charting. I want to break it down in terms of age and gender and look at two distinctive time domains, both SDNN and RMSSD. I'm about to spit out a lot of data, so just bear with me and make sure that you listen for your own age norms. So, let's start with ages 25 to 34. The study found that males in this age range had an average RMSSD of 39.7 milliseconds with a standard deviation of 19.9 milliseconds, and in SDNN of 50 milliseconds with a standard deviation of 20.9 milliseconds, they found that women had an average RMSSD of 42.9 milliseconds with a standard deviation of 22.8 milliseconds, and a standard deviation, or I should say SDNN, of 48.7 milliseconds with a standard deviation of 19.0 milliseconds. In examining men and women in the age category of 35 to 44, they found that men had an average RMSSD of 32.0 milliseconds with a standard deviation of 16.5 milliseconds, and an SDNN of 14–sorry, 44.6 milliseconds with a standard deviation of 16.8 milliseconds. They found that women in this age category had a standard deviation–sorry, an RMSSD of 35.4 milliseconds with a standard deviation of 18.5 milliseconds and an SDNN of 44.5 milliseconds with a standard deviation of 20.5 milliseconds. In examining the age category of those 45 to 54, they found that men in this age category had an average RMSSD of 23.0 milliseconds with a standard deviation of 10.9 milliseconds and an SDNN of 36.8 milliseconds with a standard deviation of 14.6 milliseconds. They found women in this category to have an average RMSSD of 26.3 milliseconds with a standard deviation of 13.6 milliseconds and an SDNN of 36.9 milliseconds with a standard deviation of 13.8 milliseconds. The next category were males and females ranging from 55 to 64 years of age. For males in this category, they found an average RMSSD of 19.9 milliseconds with the standard deviation of 11.1 milliseconds and an SDNN of 32.8 milliseconds with a standard deviation of 14.7 milliseconds. For women in this category, they found an average RMSSD of 21.4 milliseconds with an average standard deviation of 11.9 milliseconds and an SDNN of 30.6 milliseconds with a standard deviation of 12.4 milliseconds. Lastly, in the oldest category that they studied, which were those aged 65 to 74, they found that males in this age category had an RMSSD of 19.1 milliseconds with a standard deviation of 10.7 seconds and a standard deviation or SDNN of 29.6 milliseconds with a standard deviation of 13.2 milliseconds. Lastly, they found that women in this age category had an RMSSD of 19.1 milliseconds and a standard deviation of 11.8 milliseconds and an SDNN of 27.8 milliseconds with a standard deviation of 11.8 milliseconds. So, wow, there is a lot of information. I hope that this puts some people at ease as I get questions all the time about Oura ring measurements and whether they are too high or too low. And now, I highly encourage you to check out these numbers again if you have questions about how you compare with those within your age category and for your gender as well. What is great about the studies is that they do also show comparisons in the low-frequency and high-frequency bands, and then the low-frequency and the high-frequency ratio. This was a study performed by Voss and their colleagues in 2015. The last thing that I want to say about HRV norms, something that I get quite a lot of questions about is in regards to high HRV scores. As I noted before, while it is important to modern HRV from a norm standpoint, it is equally if not more important to self-quantify in an effort to compare HRV scores to yourself. This means establishing a baseline and then making comparisons not just to norms, but making comparisons to your own baseline. Now, the research is not clear on whether or not there's a ceiling to HRV scores. In other words, there's no definitive research to demonstrate that having a high HRV score compared to a low HRV score or compared to the norm has negative effects. However, it has been proposed that individuals with significantly high HIV scores may not be pushing themselves as hard as they could. Again, this is quite a subjective statement, but it is something to note. Some theorize that high HRV scores may be an indication that you could push yourself a little bit harder on your workouts, and I'm not sure I quite buy into this, but it's worth further exploring. My opinion in conclusion though is I would still, even from a personal standpoint and clinical standpoint, would like to see higher HRVs when compared to lower HRV scores. The only time that a high HRV score can be extremely problematic is if we find there is arrhythmia or some other cardiovascular problem that is contributing to long durations of time between the heartbeats. So, for example, if someone is having some arrhythmic heartbeats, they may end up skipping beats, which will result in what looks like an elevated HRV when in fact, this is more representative of dysfunction and a disorder. So, in instances like this, a high HRV can be problematic. Normally, with arrhythmias, there are going to be additional symptoms that the individual is experiencing that would warrant a stress test or an echocardiogram to determine dysfunction. So, now that we've taken a deep dive into the HRV metrics and norms, I think that it's time for us to discuss specific techniques and tactics for HRV training. I like to split this into two sections. First would be specific HRV biofeedback techniques, and the second would be HRV hacks. Some people believe that the most important metric to change is their resting HRV score, which what I would argue is highly important. But something that I would argue that is much more important than your resting HRV would be your ability to quickly and efficiently tap into your parasympathetic response. The ability to modulate HRV quickly holds substantial benefits for the individual, especially when compared to resting HRV. Well, resting HRV can be a great representation of overall health, recovery, and well-being. I'm not nearly as concerned with making substantial changes in that area as I am with parasympathetic efficiency. One thing I must say, and honestly, there is no easy way around this, in order to truly know what changes are taking place from an HRV perspective, you need to be quantifying it with some form of wearable or device. However, all the techniques that I'm going to share with you do not require HRV measuring devices in order for them to be effective. The greatest thing about biofeedback is that it's not a piece of equipment that is the change agent. Indeed, the change agent is inherently in the ways that we change our physiology. I think that it's important for us to remember this because we get so caught up in all these really cool and expensive biohacking wearables, but in the end, this is just information and not the mediator of change itself. So, if you have some expendable income, I'm going to talk about a few devices that I really like and how I utilize them practically. Many of these are fairly reasonable in price. I don't expect you to go out and buy a $15,000 piece of biofeedback equipment as this is something I would use like clinically. So, you wouldn't want to go out and do that for yourself necessarily. You would have no clue what you're doing unless you had that training. What I use on a day-to-day basis for my own personal HRV training are much less expensive devices, though I must say it is really nice to have the ability to practice on clinical biofeedback whenever I want. But trying to carry around all that equipment is a bit of a hassle when I can just throw on my Oura ring. So, the first tactic to HRV training and HRV biofeedback that I want to discuss is what I considered the most important or something that I believe each and every person who is doing HRV training should learn. And this is something called resonance frequency training, which is an assessment tool and technique created by Paul Lehrer. This entails you determining the exact resonance frequency of your cardiovascular system. This frequency is a manipulation of your respiration rate, which has a significant impact like we talked earlier on your heart rate due to the stimulation of the baroreflex. At this respiration rate, there is significant effects due to maximized respiratory sinus arrhythmia and baroreflex gain. The idea behind resonance frequency training is to breathe at a rate that causes the heart rate to go up and down in phase with your own respiration rate. At this rate, respiratory gas exchange is efficiently maximized. And what researchers have determined is that when you engage in regular practice of resonance frequency techniques, it has been shown to provide clinically significant improvements in a variety of symptoms and disorders such as chronic pain, asthma, depression, COPD, food cravings, and hypertension, just to name a few. What Dr. Paul Lehrer and his colleagues found is that when a person breathes at their resonance frequency rate, which is typically between four and a half and six and a half breaths per minute, the cardiovascular system will resonate, much like the sound of a vibrating string in a box above the violin, creating this big reverberating sound. Again, when breathing at this resonance frequency rate, the baroreflex system is stimulated and strengthened. Again, this is that blood control and emotional regulation control mechanism. And we find this to be at its most efficient rate when we're breathing at the resonance frequency rate. Remember too, when our blood pressure goes up, the baroreflex causes the heart rate to go down. And this is what causes that rhythm and that heart rate fluctuation. From a clinical standpoint, there are a couple of things that we are looking at in assessing resonance frequency. First, we are looking at something called phase convergence with breathing. And what this means is that we want to see that the heart rate and respiration rate are in phase or in agreement with one another. Basically, do the lines trace the same pattern? Where you start breathing, the heart rate follows the breath all the way to the peak, and as you exhale, the heart rate should decline with this line pattern. The next thing is looking at heart rate amplitude. We're going to choose the resonance frequency rate that has the highest amplitude to remind you is the highest heart rate minus the lowest heart rate within a respiratory cycle. Then we want to see which breath rate maximizes the low-frequency amplitude peak. Basically, which breath rate has the most power in the low-frequency domain? Given all these factors, we then calculate our own resonance frequency. Now, you are only going to really be able to do this if you have a more advanced HRV measuring device, such as a Polar chest strap with the Elite HRV or clinical biofeedback. The most accurate results are going to be by going to see a biofeedback practitioner. The good thing though is that we know through research that we all have, probably all have a resonance frequency in between four and a half to six and a half breaths per minute. As a safe bet, I will typically tell people to breathe at around six breaths per minute if they do not have access to this testing metric. Research has indicated that this is the strongest way to coach and train vagal tone and increase HRV. The idea behind this is that the more frequently we train using our resonance frequency training, the more easily we can tap into the low-frequency band. Something interesting about this type of training is that elite athletes have utilized this in order to get into the zone before a serve, like in tennis, or before a golf swing, or before a pitch is thrown in Major League Baseball. If we train the style of breathing and pace of our breathing on a daily basis, our body is going to most easily adapt and we are going to be able to tap into the state and maximize HRV within two to three breaths. Again like anything, this is going to take consistent practice. I might also mention that there are a few ways to practice this style of breathing. Of course we need to be able to pace our breathing, but also there are some suggestions on how we breathe mechanically. First is for us to exercise a diaphragmatic breath. This is where we inhale through our nose and allow our lungs and stomach to expand so that it can push the diaphragm towards the pelvic floor. I like to use some visual imagery to demonstrate this. When we inhale, I want you to think of your lungs and stomach like operating like a balloon would. As you bring air in through your inhalation, you will imagine that you are filling the balloon with air, allowing it to expand to about 80%. Don't overinflate the balloon. Once you're at this point, you will then exhale slowly and quietly and deflate the balloon. Sometimes I like to think about myself gently pulling my belly button towards my spine. I'm not tugging or trying to allow the air to be pushed out, I want to allow this to feel as effortlessly as possible. When this occurs, we are able to stimulate the vagus nerve that innervates the posterior section of your lungs. This will also help to maximize respiratory gas exchange for an increased oxygen and nutrient delivery. Then depending on who you ask, you can either exhale through pursed lips like you're blowing through a straw, or you can simply just breathe back through your nose. That's typically my suggestion. It's imperative to breathe or inhale through your nose as this will actually maximize nitric oxide delivery and vasodilation, which are very important in increasing HRV. One of the biggest training tools that I will use and that I find to be best is to breathe as quietly and as gently as you can. I do not want to try to see, or I should say–yeah, I do not want to try to see if I can inhale as much air as I can as possible. I will actually want to just focus more on the slow quiet diaphragmatic breaths. And sometimes I'll even create what feels more like a hypoxic environment in my body. And this is similar to the work of Patrick McKeown, who wrote “The Oxygen Advantage.” If you're breathing this way and training this way, the research suggests that you need to perform this for about 20 minutes two times a day. And I like to utilize this strategy when I'm engaging in meditation or just as a separate health strategy. So, that's resonant frequency training. Now, of course, there are many other breathwork techniques that you can utilize, but I found this one to be quite effective both personally and clinically. The key features to this style of breathing is to remember to breathe low, to breathe slow, and to breathe quietly. Again Patrick McKeown, who, like I mentioned earlier, the author of “The Oxygen Advantage,” recommends to breathe so quietly as if you are not trying to move any hairs within your nostrils. So, have that visualization as you take a breath in. Another way to maximize HRV is through the process of meditation. Indeed, numerous research studies have indicated that engaging in different meditative techniques such as visualization or guided imagery meditation and mindfulness meditation can significantly improve overall HRV. This is likely due to the fact in correlation of slow respiratory patterns when engaging in these exercises. But also that mediation, or meditation I should say, brings about a sense of calm and safety, which is likely due to vagal tone or vagal nerve stimulation. I tend to like to pair breathwork in meditation as I'm always looking to maximize efficiency and time in my day. These techniques, when I combine them with my utilization of biofeedback wearables, has been found to be the most effective way for me to enhance HRV. If you're looking in the wearables and self-quantification scene, you likely already know of many wearables for determining HRV. I have found some to be really good and I have found some that have left me quite disappointed. I like checking HRV in different ways. So, first, I like checking the resting or that static HRV state. This is going to give me an HRV that is not manipulated by respiration and is a better representation of my overall nervous system recovery. Remember, it's actually quite easily–or I should say it's actually quite easy to manipulate HRV via breathing slowly and diaphragmatically. As such, I do like to measure HRV when I don't have the opportunity to manipulate the results, and the perfect place and time for that is sleep. Now, I know that I've already mentioned the use of my Oura ring, which I found to be one of the most accurate ways to measure HRV non-invasively. There are also other devices such as the WHOOP band and the Biostrap that can provide accurate results. I tend to like something that's a little less invasive physically such as a ring over a wrist strap. However, you need to go with your own preference. Also, whatever device that you end up getting, you need to make sure that you're basing your norms on the metrics of the device that you're using. For instance, if you use your Apple watch, which Apple watch does calculate HRV, their measurement is SDNN, while the Oura ring uses the RMSSD metric. So, each morning, I take off my ring and then put it on the charger to get it off airplane mode, and I'll check a few metrics in regard to sleep. I'll look at body temperature and then I'll look at heart rate variability. I'll always look at my HRV numbers in comparison to both my own, as well as the normative population. The great thing about self-quantification is that we can establish a baseline for ourselves and then make general comparisons to that baseline. While it's important for you to compare yourself to norms, it is equally, or maybe more important for you to have a baseline comparison for yourself. I utilize this number for my ring to give me a good representation as to my overall level of recovery. Your nervous system is not going to lie. If your HRV is significant low, say one to two standard deviations below your average, then that may give you the information about whether or not you should train that day or how hard you should train. Let me give you a personal example of how I've utilized this. I typically play tennis two to three days a week. My average ring score is about 110 to 115 milliseconds. If my HRV score the following morning is 80 or below, I will typically take it a little bit easier on physical exertion that day. Interestingly enough, our autonomic nervous system recovers fairly quickly, but research has also indicated that HRV can be a great measurement of recovery in order to prevent injury or re-injury. I have used this as a reliable means to avoid injury. And I've also found that when I have overreached or overtrained and my HRV measurements told me I was already doing that, then this has resulted in me engaging in more injury or being more prone to injury. One thing to also keep in mind is that decreased HRV is highly associated and correlated with increased heart rate. For instance, we know that a heavy night of drinking alcohol can cause the heart rate to go up. And in turn, this will end up resulting in a decreased HRV. So, if you notice that your HRV is significantly lower on nights that you consumed alcohol, that is why. Now, if I'm doing more HIV biofeedback training and to increase my HRV from an emotional or psychological or stress-based standpoint, then there are numerous devices that you can use for feedback for, in the moment, HRV scores. Some popular ones include the emWave2 and Inner Balance by the HeartMath Institute. And as I indicated earlier, the intent behind these devices from HeartMath is increased coherence, which is very similarly associated to resonance frequency. Both of these devices utilize PPG or photoplethysmography, which I mentioned earlier, and our devices that typically go on the ear lobe or on the finger and look at overall blood volume fluctuations through infrared lights that shine through the muscular tissue. This is a great and accurate means of measurement, as well as easy and efficient to determine HRV. The only way, or I should say the other way is through ECG or electrocardiogram, which is a little more complicated, but in my opinion, is the most reliable due to the minimization of artifact. You can use these devices to help coach you in different breathing techniques and meditative techniques to increase HRV. You can see HRV waveforms begin to establish after just a few minutes of breathing in a coached pattern. And what's going on here is a strengthening of your overall autonomic nervous system, an enhancement in autonomic balance and vagal stimulation that is increasing acetylcholine production that helps to regulate the speed of your heart. Most people will say that they feel the effects of this HRV training within a matter of minutes. And because I've trained on these types of devices for so long, I can enhance my own HRV within a matter of about two or three breaths, and this demonstrates strong and specific and efficient control of my autonomic nervous system, something that you can do as well with training. And I like these devices because they are very accurate and user-friendly. There are other training devices such as the Biostrap and WHOOP that can be paired with their own app. But there are also devices that I found to be the most accurate and effective devices for HRV biofeedback. One of them is the highly popular and well-known Elite HRV app and the Polar chest strap. This isn't actually an ECG device that instead of measuring the blood flow and the blood volume pulse, such as the devices I mentioned earlier, this will actually measure the electrical output of the heart. Now, these are a little bit more invasive, something that you can clip on your finger or your ear, but I like them because their accuracy and ability to reduce artifacts, and as you remember, artifacts are like those false beats. Many of the wearables do not remove false beats, which can lead to very inaccurate data. The Polar H7 chest strap with either the NatureBeat or the Elite HRV app is a great way to go, but I actually have one app or one device that is not as well-known, but I've found it to be without a doubt my favorite device that I've ever worn for heart rate variability training. The device that I'm talking about is by a company called Lief Therapeutics, L-I-E-F Therapeutics. This is a wearable ECG device that attaches to two separate electrodes and is placed right below the left chest, similar to the position where you would place a full ECG. This device is very lightweight and will track HRV throughout the day. The great thing about this device is that it will help you to establish your own baseline, and then throughout the day, it will detect when your HRV has fallen significantly below your baseline. You will then receive haptic vibrating feedback in a vibrating pattern to let you know that your HRV is low. And once you fill this haptic feedback, it will then provide you with different vibrating patterns consistent with whatever breathing pattern you have indicated to the app that is your preferred respiratory rate. So, for instance, in my resonant frequency, it's five breaths per minute, which might actually is. On the phone application, I can tell it that when my HRV has fallen significantly lower than my baseline, to start a breathing pattern at that rate. There will then be two distinct feedbacks from the haptic engine that I will experience at this time. When there is no vibration on the device, this is telling me to start my inhalation. When the device begins to vibrate, I will exhale until the vibration is complete. I will do this until I've gotten my HRV back up to baseline. After a period of time wearing the Lief device, I have found that I am able to increase my level of self-awareness and also my ability to more quickly regulate myself HRV that I have seen kind of multiple benefits with this thing. This is so much so that I'm able to pinpoint now when my advice will begin to vibrate even before it begins vibrating. My level of self-awareness regarding my stress response in HRV has become so heightened due to this device that I don't even need it anymore, but I still use it because–well, I've found that it's just the best HRV biofeedback device I've ever used. The application also has multiple guided meditations, abilities to track HRV on a daily and weekly basis, the ability to train with paced breathing, the ability to feel your own heartbeat from the haptic feedback engine and much more. You can find more about this company if you go to getlief.com, L-I-E-F. But I cannot stress how much I've used this device and found benefit, as well as how many of my patients have utilized this device and found significant benefit as well. This is the device that I have all of my personal clients buy for coaching and the one that I personally use. My last comment on HRV wearables is to gain–or I should say to again remind you to be aware of the potential inclusion of artifact data. This is something that can significantly skew your results and should be assessed and taken into consideration before assessing HRV. One way to help mitigate the effects of artifact collection is to make sure that you are sitting at a table or sitting in a stable position and that you are just completely still during readings, especially during short-term readings. I generally also check my HRV at the same time each day, and even in the same place each day to get readings that are as reliable and as consistent as possible. There are plenty of other ways to increase your overall HRV. One of the ways that I have found to be the most effective increasing the resting HRV is through the use of cold exposure. So, cold exposure, as many of you know, is a hormetic stressor that results in acute sympathetic state arousal. As such, this is the perfect time for us to induce a parasympathetic state during the cold exposure and during cold recovery. What you may notice initially is a significant decrease in HRV immediately following the cold exposure, and this of course is common. However, because our body wants to reenter a state of homeostasis, the reparative process will result in higher HRV. I have found that through the use of either cold plunges or hot to cold contrast showers, I've been able to modulate my HRV pretty significantly with these techniques. I also like the idea of cold exposure at night. So, quality sleep is also a way to increase HRV. And tracking HRV alongside sleep is a valuable system of this quantification. What you will find is that the lower your heart rate goes due to more deep and restorative sleep, the higher your HRV will be. And as I mentioned before, one of the things that helps me sleep immensely from a recovery standpoint and overall quality of sleep standpoint is by using a mechanism to cool my bed, such as the Ooler system or the chiliPAD. I've noticed significant enhancements in overall HRV when cooling my core temperature down with a cold shower as well before bed, and then I use the chiliPAD system at night when I sleep. Hands-down, the most robust research for increasing overall HRV aside from HRV biofeedback for stress reduction is physical exercise. Now, given this audience, I know I do not need to go into the benefits of exercise, but many research studies have looked at how exercise can enhance each HRV both from a cardiac standpoint and from an autonomic balance standpoint. If you haven't already gathered, we have to remember that there is a dose-response curve with exercise. As Ben always says, we're looking for the minimal effective dose of exercise, and this is true for exercise effects on HRV. We indeed know that if we continually and consistently overtrain, this is going to lead to increased chance for injury and has a highly predictable correlation with low HRV. We can use both a low HRV to demonstrate overall recovery or lack thereof, but we also know that continued overtraining will result in the continued lowering of HRV. For instance, in one study looking at the effects of moderate exercise versus heavy endurance exercise on nocturnal HRV, that's the resting HRV, researchers found that heavy endurance athletes such as marathon runners had significant low-frequency power during heavy training and after a marathon. In this study, we actually see decreased HRV during the nocturnal hours after both moderate exercise and marathon completion. But we see statistically significant reductions in HRV for those who are engaging in heavy endurance exercise when compared to those engaging in moderate exercise. This isn't surprising that we would see a reduction in HRV for those engaging in moderate exercise, but it does go to show that there is significant HRV reduction after heavy or intense exercising. One strategy that I utilize personally is the uses of HIIT training or high-intensity interval training and Tabata sets. Because these are types of workouts that are more effective in stimulating our body's need to adapt, they can also increase HRV in the long run. Now, as a general rule of thumb, if my HRV is significantly lower on the day, I will never utilize this type of training. I will almost always avoid doing so in an effort to avoid overtaxing my nervous system. When they examined the usage of high-intensity interval training, this is researchers, versus moderate intensity continuous training on HRV, the individuals–I should say individuals who are considered physically inactive, they found that HIIT training was significantly superior to moderate intensity continuous training and improving HRV. One study that really stood out to me was examining the effects of physical exercise on HRV in patients with cancer diagnosis. They found that these individuals with cancer diagnosis that engaged in exercise actually enhance their overall HRV and cardiac autonomic regulation. And it was concluded that because of the association of higher HRV parameters and prolonged survival in cancer patients, exercise to increase HRV in these individuals can be a highly effective treatment strategy. So, it's my guess that we're going to see more studies on the efficacy of exercise on HRV as time goes by. Another tactic that I utilize on a daily basis for increasing HRV is compassion and meditative practices. So, numerous studies have indicated that engaging in a meditation practice can increase HRV by reducing the fight-or-flight response and increasing our safety response. I found this as a highly useful strategy for myself and for my patients and have seen demonstrable effects for increasing HRV with this type of practice. One study examined the use of gratitude journaling on HRV and other inflammatory biomarkers and individuals with heart failure. They found that these individuals that participated in gratitude interventions had reduced inflammatory biomarkers and increased parasympathetic HRV responses when they were engaging in the gratitude task. While the results did not indicate a significant difference in HRV after journaling, there were notable benefits during the time of journaling. And inflammation biomarkers were significantly changed and maintained after intervention, which is really cool. This is why I believe that it's important for us to engage in mindfulness-based exercises and gratitude exercises each and every day as this can have valuable benefits to our sense of safety and well-being. The last thing that I will say that this could be a podcast in and of itself is that there are plenty of dietary considerations. Now, I could get into one diet over the other, whether it's carnivore versus omnivorous diet on HRV. And there's really not a lot of great data to support one or the other specifically for HRV. However, we do know that a whole foods anti-inflammatory dietary pattern is going to be significant benefit on HRV when compared to the standard American diet. As we know, there is a significant reduction in inflammatory markers and stress that can significantly enhance HRV. So, the takeaway from this, which you may already know, is to find what dietary patterns work best for you and watch HRV scores as you manipulate what you're eating. One thing to note about fasting, as many individuals ask about what fasting does to HRV, interestingly enough, we have data to demonstrate that short-term fast or time-restricted eating can significantly enhance HRV in the long run. However, do not be surprised if you see significant reductions in HRV when you are engaging in an extended fast. You have to remember, a fast is a form of hormetic stress, and therefore, in the temporary, can reduce HRV scores. However, as the body repairs and returns to homeostasis, we tend to see HRV increase. In the end, if we break HRV optimization down in its most simplistic form, we are truly looking to tell our brain in our body that we are safe. One of the most famous researchers on HRV modulation is Dr. Stephen Porges that I mentioned earlier, who created “The Polyvagal Theory.” In this theory, Dr. Porges proposes competing roles for the unmyelinated fibers in the vagus nerve and the newly more evolved myelinated nerves. Now, he theorized that the evolution of the autonomic nervous system was central to the development of emotional experience and effective processes involved in our social behavior. As human beings, we are not limited to fight, flight, or freezing behavioral responses. We can self-regulate and initiate pro-social behaviors, which may be referred to as those tend-to-befriend behaviors when we do encounter stressors. This is what Dr. Porges calls the social engagement system. And the theory suggests that the system depends on the healthy functioning of the myelinated vagus nerve, which works like that vagal break. From this perspective, we can only activate the myelinated vagus when our nervous system perceives that we are safe. When we engage in social safety, we perceive this as a mutual process, one that involves eye contact, close proximity, and trust. This myelinated vagus enables us to self-regulate, calm ourselves, and inhibits the sympathetic outflow of the heart. The myelinated vagus also allows us to engage the prefrontal cortex and executive functions where we can be attentive and mindful when we encounter daily stressors. This will inhibit the myelinated vagus and produce what is called vagal withdrawal. This will then interfere with our attentiveness and our level of social engagement. According to this theory, quality communication and pro-social behaviors can only be effectively engaged when our defense circuits are inhibited. So, how do we increase HRV in the most consistent and effective manner? We must have a perceived sense of psychological and physiological safety. We are constantly evaluating our environment for threats as a way to maintain our safety both physically and psychologically. When this occurs for days, weeks, years, or decades, this can result in an overarching schema of continued concerns of our lack of safety or lack of trust and others, and ultimately, social disengagement or withdrawal. These isolated behaviors and distortions in our cognition have significant impact on our stress physiology, heart rate variability, and can directly play a role in our perceived sense of meaning and purpose in life. This brings it all together. When our nervous system perceives safety, we activate the myelinated vagus nerve system, and this is a way to conserve and rebuild energy stores to socially bond with others and engage in executive functioning like self-regulation and planning. When our nervous system perceives danger, we activate the sympathetic nervous system and inhibit the unmyelinated vagus resulting in the fight, flight response or active avoidance. If we perceive that our life is at threat and that the fight, flight, or active avoidance response system will not succeed, then we'll actually activate our unmyelinated vagus, which will result in passive avoidance through behaviors like immobilization, feigning death, fainting or shutting down completely. This threat to our survival is what Dr. Stephen Porges believes activates the unmyelinated vagus and results and subsequent disorders like PTSD. This again is why safety security and trust is needed to maximize health outcomes from a mind, body, and spiritual perspective. So, there you go. Man, we have taken a deep dive into all things HRV, but we've only scratched the surface. My hope is that this information was useful and resulted in you learning the ins and outs of why HRV and the self-regulation of HRV is of vast importance for physical and mental health. If this metric of quantification has not been of importance to you in the past, I sure hope that you now see why it should be. In my guess, like anything in the field of science, we're going to learn more and more about this metric and the usefulness of it as we expand the field of research. I hope this podcast has highlighted how important this metric of HRV is and why it should be important for us to consider finding a coach that can help you increase your parasympathetic efficiency quickly, as this is one of the strongest ways to mitigate stress, to improve recovery and enhance performance and longevity. Thank you, Ben, for providing me with your platform to share my passion on heart rate variability and self-regulation. Like I mentioned earlier, you can also find all the shownotes at BenGreenfieldFitness.com/hrvpodcast. And you can check me out at drjaywiles.com, or at my practice which is thrive-wellness.com. Take care, everybody, and have an awesome day." References
Greenfield, B. (2020). [Transcript] - A Deep Dive Into HRV: How To Use Heart Rate Variability To Optimize Your Sleep, Stress, Recovery, Performance, Nervous System Balance & Much More! - Ben Greenfield Fitness - Diet, Fat Loss and Performance Advice. Retrieved 13 March 2020, from https://bengreenfieldfitness.com/transcripts/transcript-what-is-heart-rate-variability/
It is widely recognized that radiation exposures such as X-rays and gamma radiation can increase the risk of cancer in humans and animals. These types of radiation are referred to as ionizing radiation (Ionization energy is defined as the minimum amount of energy required to remove an electron from an atom or molecule in the gaseous state). This is different from nonionizing radiation, which includes ultraviolet (UV), visible light, extremely low frequency radiation (ELF), and radiofrequency or microwave (RF) radiation. Conventionally, researchers believed that nonionizing radiation is not harmful or carcinogenic, despite evidence surfacing regarding the relationship between UV radiation and skin cancer. Research evaluating the exposure to RF radiation was conducted primarily by military agencies. Due to the advent and use of cellular telephone systems, which involve widespread public exposures, reevaluation of exposure risk has become urgent. Four types of physiological effects has been observed by researched in multiple studies:
These findings suggest that exposure to RF radiation, including from devices such as microwave ovens, are potentially carcinogenic and have other health effects. An important point to consider is that low dose radiation exposure over time has damaging effects, rather than one large exposure to radiation. Alternatives to Microwaves Rather than using a microwave, consider using a stove or convection oven. These methods take a bit more time, but it is well worth it! Consider using headphones to talk on cell phones rather than placing the device directly to your head. If possible, request to avoid airport scanners by opting for a pat-down. Lastly, try to reduce overall radiation exposure over time. References Goldsmith, J. (1997). Epidemiologic Evidence Relevant to Radar (Microwave) Effects. Environmental Health Perspectives, 105, 1579. https://doi.org/10.2307/3433674
Over the course of the past century, the Western culture has faced numerous health epidemics, from obesity to opioids. Today we are facing an epidemic of a different nature. The epidemic of loneliness. We're more connected than ever, but are we feeling more alone? In the last 50 years, rates of loneliness have doubled in the United States. In a survey of over 20,000 American adults, it was found that almost half of respondents reported feeling alone, left out, and isolated. Further, one in four Americans shared that they rarely feel understood, and one in five people believe they rarely or never feel not close to people. Loneliness is on the rise for Americans regardless of geographic location, gender, race, or ethnicity. Human beings did not evolve to be alone. Sociality plays a fundamental part in the wellbeing of Homo sapiens. Conversely, social isolation and loneliness are known risk factors for premature death, more so than being obese (Holt-Lunstad et al., 2015). Individuals who feel socially isolated and alone also have higher rates of cardiovascular disease, alcoholism and suicidality, physical diseases related to stress and compromised immune function, and in later life, greater risk of degenerative dementia. Even worse, researchers have observed that geriatric individuals who are considered lonely have a 45% increased risk of mortality (Leland, 2012; Perissinotto, Stijacic Cenzer and Covinsky, 2012). Moreover, lonely individuals experience reductions in reasoning and creativity. In addition to these reduced abilities, loneliness affects workplace productivity, as lonely individuals report less job satisfaction and are more likely to face unemployment. Not surprisingly, loneliness is commonly correlated with mental health concerns such as anxiety and depression. Similarly, loneliness is often associated with poor coping mechanisms, such as compulsive technology use, smoking, and self-harm. In other words, loneliness has both physical and psychological implications, many of which could be long term. Alone versus Lonely Before determining yourself as lonely, there is a difference between being alone and feeling lonely. Being alone and feeling lonely are not mutually dependent. Loneliness is a subjective experience, a feeling of sadness stemming from isolation or abandonment. But, a person can be alone without feeling lonely, since alone describes a state of being and lonely describes an emotional response to one's circumstance. For example, most people don't feel sad when they go to the restroom by themselves. A person can be alone in the sense that no other people are present, or alone in the sense that they are unaccompanied, even in a crowd. When assessing loneliness, introverted and extroverted personalities should be taken into account, because some people enjoy the presence of being alone with themselves, whereas others are dependent on others to cope with not being by themselves. Being at either end of the spectrum, whether it is total isolation or complete dependence, is not considered a healthy behavioral pattern. Factors Influencing LonelinessThe predictors of loneliness is the basis for the identification of factors that cause and contribute to loneliness. The are three broad categories that influence the feeling of loneliness:
These categories may be subdivided into multiple factors that increase loneliness:
While it is impossible to avoid loneliness completely, it may be alleviated. It is recommended to investigate the contributory factors towards loneliness because knowledge of these may substantially lessen the impact of loneliness on people's mental health status. Such knowledge will contribute to an improved quality of life, productivity and health. Sleep Deprivation-Induced Loneliness The "loneliness phenotype" can be triggered by sleep deprivation. Researchers have observed that a lack of sleep induces critical changes within the brain, altering behavior and emotions, while also disturbing essential metabolic processes and influencing the expression of immune-related genes. The end result is that people who are sleep-deprived avoid social interaction. This asocial profile is recognizable by other people, who, in turn, shun the sleep-deprived people in a psychosocial loop that perpetuates in a vicious cycle of loneliness and other mental health disorders. Some Solutions to Loneliness REferences Ali, S. (2018). What You Need to Know About the Loneliness Epidemic. [online] Psychology Today. Available at: https://www.psychologytoday.com/us/blog/modern-mentality/201807/what-you-need-know-about-the-loneliness-epidemic [Accessed 1 Sep. 2019].
Harris, R. (2015). Are we lonelier than ever?. [online] The Independent. Available at: https://www.independent.co.uk/life-style/health-and-families/features/the-loneliness-epidemic-more-connected-than-ever-but-feeling-more-alone-10143206.html [Accessed 1 Sep. 2019]. Holt-Lunstad, J., Smith, T., Baker, M., Harris, T. and Stephenson, D. (2015). Loneliness and Social Isolation as Risk Factors for Mortality. Perspectives on Psychological Science, 10(2), pp.227-237. https://doi.org/10.1177/1745691614568352 Leland, K. (2012). Loneliness Linked to Serious Health Problems and Death Among Elderly. [online] UC San Francisco. Available at: https://www.ucsf.edu/news/2012/06/98644/loneliness-linked-serious-health-problems-and-death-among-elderly [Accessed 1 Sep. 2019]. Perissinotto, C., Stijacic Cenzer, I. and Covinsky, K. (2012). Loneliness in Older Persons. Archives of Internal Medicine, 172(14). https://doi.org/10.1001/archinternmed.2012.1993 Ben Simon, E. and Walker, M. (2018). Sleep loss causes social withdrawal and loneliness. Nature Communications, 9(1). https://doi.org/10.1038/s41467-018-05377-0
Skyscrapers, prison cell-like living quarters, stressful mediocre jobs and impersonal city life do not encourage friendliness, let alone a sense of community. A city is simply a place where large groups of lonely people live together. The ostensible connectedness that cellphones and devices alike offer is attenuated by the unexpected consequence of decreasing the desire to connect with others, contributing to loneliness and isolation overtime. Researchers have observed subjects using cellphones for a short period of time were less likely to volunteer for a community service activity when asked compared to a control group. In addition, the cellphone users were less determined in solving word problems, even when the amount of correct answers would be matched by a monetary donation to charity. This deflated focus on others persisted even when the cellphone users were requested to draw an image of a cellphone and think about using it. The researchers posit, “The cellphone directly evokes feelings of connectivity to others, thereby fulfilling the basic human need to belong.” The researchers suggest that this feeling results in a reduced desire to actually connect with others or to engage in empathetic and prosocial behavior (Abraham, Pocheptsova & Ferraro, 2019). Loneliness also correlates with Internet use (Hu, 2009). Researchers observed that online chatting resulted in increased loneliness (Hu, 2007). Jacob Needleman, professor of philosophy at San Francisco State University, suggests that the loneliness that we as a society are experiencing cuts people off, not just from each other, but also from some harmonizing force in themselves. Our society is lacking an essential harmonious relationship with some universal force (Needleman, 2014). The absence of this essential harmonious relationship will not be filled by Facebook, Instagram, or any other social networking website. References Abraham, Ajay & Pocheptsova, Anastasiya & Ferraro, Rosellina. (2019). The Effect of Mobile Phone Use on Prosocial Behavior.
Dossey, L. (2013). One Mind. Carlsbad: Hay House. Hu, M (2007). Social Use of the Internet and Loneliness. Hu, M. (2009). Will Online Chat Help Alleviate Mood Loneliness?. Cyberpsychology & Behavior, 12(2), 219-223. doi: 10.1089/cpb.2008.0134 Needleman, J. (2014). The heart of philosophy. New York: Jeremy P. Tarcher. |
The Awareness domain contains research, news, information, observations, and ideas at the level of self in an effort to intellectualize health concepts.
The Lifestyle domain builds off intellectual concepts and offers practical applications.
Taking care of yourself is at the core of the other domains because the others depend on your health and wellness.
Archives
May 2024
Categories
All
|

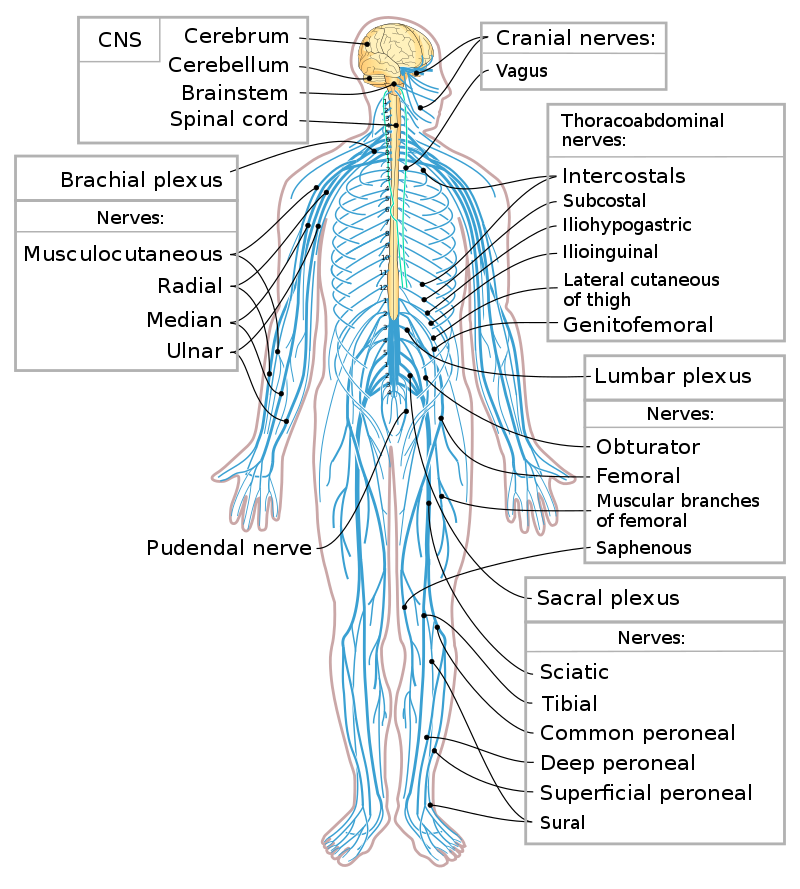


 RSS Feed
RSS Feed

