Counter to the nutrition narrative of the past half century, cholesterol is not responsible for killing countless people and wreaking havoc on public health. Whether dietary or innate (found in blood), cholesterol has appeared to be deemed as dangerous at all costs. This demonization has led to disapproval of various foods including eggs, butter, and saturated fats, as the current narrative proposed that cholesterol is to blame for all cases of heart disease in the past several decades.
The problem of cholesterol has led to reaction of fear, and thus the "solution" of a multi-billion dollar industry promoting statins and other drugs targeting lower cholesterol. With the administration of statins on the rise, in 2012 nearly one third of adults over the age of 40 were taking cholesterol-lowering drugs, as well as half of adults over the age of 75 years.¹ Today, adults as young as 18 are being targeted to take these devastating compounds.² In fact, Atorvastatin (Lipitor) has been listed as the America's most commonly prescribed drug.³
The war on cholesterol has been the catalyst of a whole new food industry offering low-fat alternatives (which often contain more sugar). This war has been so insidious that has affected the standard American's daily life, from the USDA's food pyramid-plate⁴, school lunches⁵, and medical centers⁶.
Given the wide-spread recommendations, an announcement of the US Dietary Guidelines Advisory Committee appeared to have been over-looked: dietary "cholesterol is not a nutrient of concern for overconsumption", as available evidence shows no appreciable relationship between consumption of dietary cholesterol and serum cholesterol.⁷
Dr. Arthur Labovitz, chairman of the cardiovascular department at the University of South Florida’s Morsani College of Medicine and a board member of the Tampa Bay American Heart Association, was among those supporting the committee’s decision to end the war on cholesterol.
"What we've learned is the amount of cholesterol you eat really does not have a really profound impact on the cholesterol in your blood,” Labovitz told the Tampa Bay Times.⁸ "… We're not telling people to eat five eggs a day. What we're saying is (cholesterol in food) is not poison."
To get to the root of the issue, it's best to examine what cholesterol is, and the history behind how it entered the limelight.
The problem of cholesterol has led to reaction of fear, and thus the "solution" of a multi-billion dollar industry promoting statins and other drugs targeting lower cholesterol. With the administration of statins on the rise, in 2012 nearly one third of adults over the age of 40 were taking cholesterol-lowering drugs, as well as half of adults over the age of 75 years.¹ Today, adults as young as 18 are being targeted to take these devastating compounds.² In fact, Atorvastatin (Lipitor) has been listed as the America's most commonly prescribed drug.³
The war on cholesterol has been the catalyst of a whole new food industry offering low-fat alternatives (which often contain more sugar). This war has been so insidious that has affected the standard American's daily life, from the USDA's food pyramid-plate⁴, school lunches⁵, and medical centers⁶.
Given the wide-spread recommendations, an announcement of the US Dietary Guidelines Advisory Committee appeared to have been over-looked: dietary "cholesterol is not a nutrient of concern for overconsumption", as available evidence shows no appreciable relationship between consumption of dietary cholesterol and serum cholesterol.⁷
Dr. Arthur Labovitz, chairman of the cardiovascular department at the University of South Florida’s Morsani College of Medicine and a board member of the Tampa Bay American Heart Association, was among those supporting the committee’s decision to end the war on cholesterol.
"What we've learned is the amount of cholesterol you eat really does not have a really profound impact on the cholesterol in your blood,” Labovitz told the Tampa Bay Times.⁸ "… We're not telling people to eat five eggs a day. What we're saying is (cholesterol in food) is not poison."
To get to the root of the issue, it's best to examine what cholesterol is, and the history behind how it entered the limelight.
What is Cholesterol, and Why is IT Necessary?
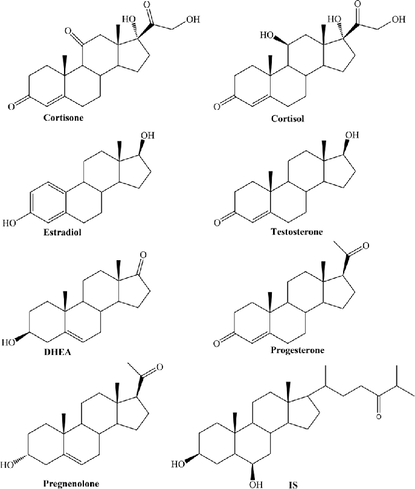
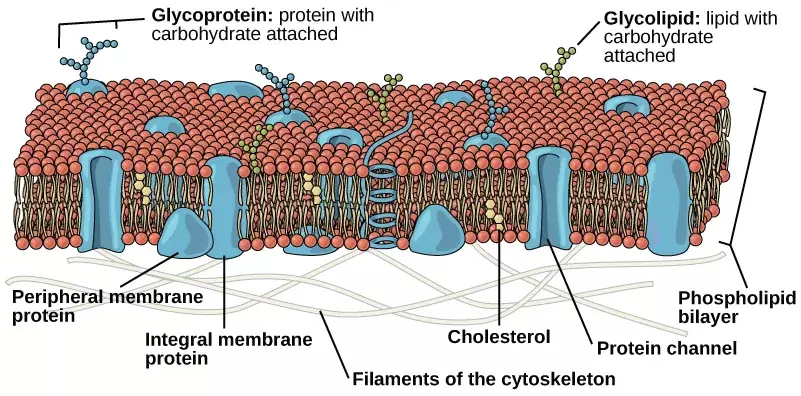
Cholesterol is a soft, waxy substance which exists in every cell, as well as the bloodstream. It is responsible for the structural integrity of cell membranes, hormone precursors (testosterone, estrogen, progesterone, cortisol), vitamin D synthesis, and the development of bile acids to help breakdown fat.
Cholesterol is crucial for optimal health and quality of life. In fact, the brain is the most cholesterol-rich organ in the body, and researchers have observed that cholesterol serves a vital role in normal cognitive function, including learning and memory.⁹
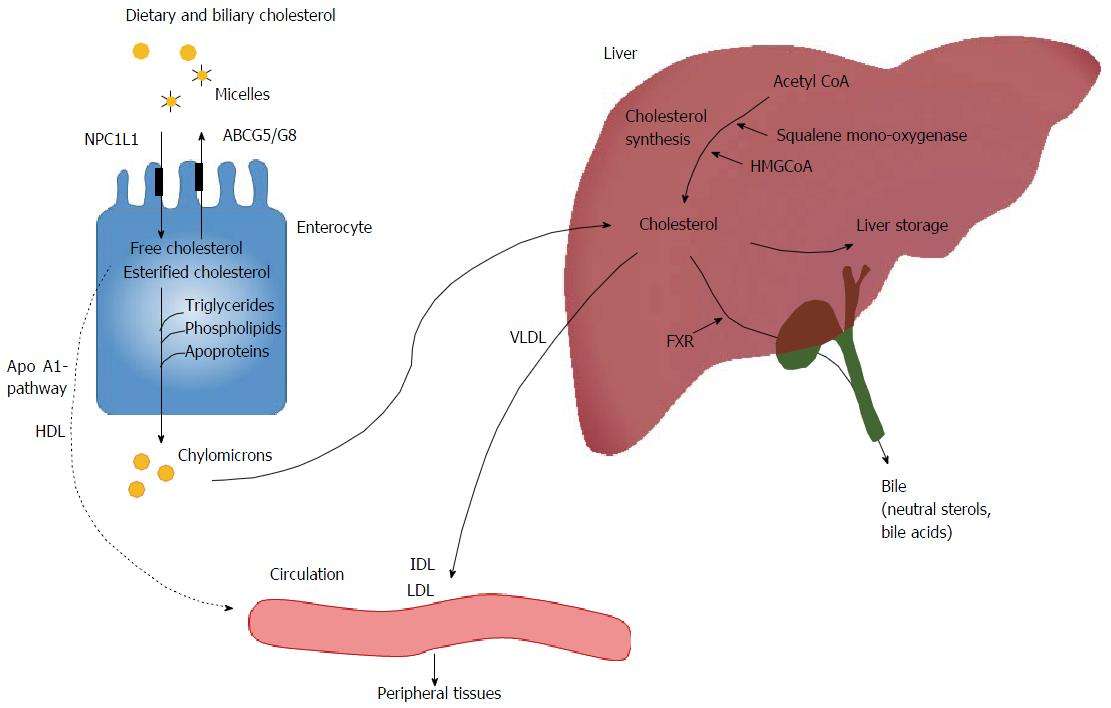
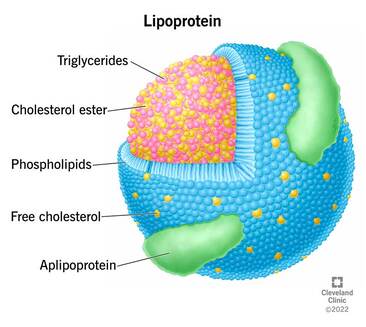
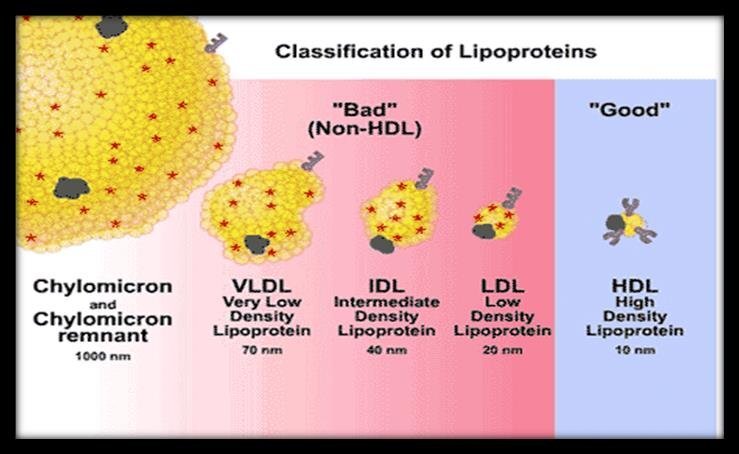
The liver is the source of the majority of cholesterol synthesis. Cholesterol travels through the blood on proteins called “lipoproteins.” Lipoproteins are round particles made of fat (lipids - consisting of cholesterol and triglycerides) and proteins that travel in your bloodstream to cells throughout your body, of which there are two primary types:
Cholesterol is crucial for optimal health and quality of life. In fact, the brain is the most cholesterol-rich organ in the body, and researchers have observed that cholesterol serves a vital role in normal cognitive function, including learning and memory.⁹
The liver is the source of the majority of cholesterol synthesis. Cholesterol travels through the blood on proteins called “lipoproteins.” Lipoproteins are round particles made of fat (lipids - consisting of cholesterol and triglycerides) and proteins that travel in your bloodstream to cells throughout your body, of which there are two primary types:
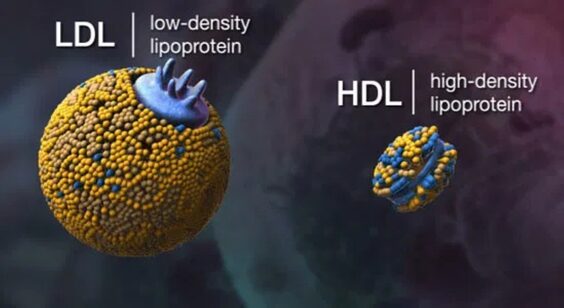
- High-density lipoprotein (HDL): otherwise referred to "good" cholesterol, this compound has been demonstrated to remove LDLs in arteries by transporting them back to the liver for processing. HDLs also aid to help repair the inner walls of blood vessels, thereby preventing heart disease.
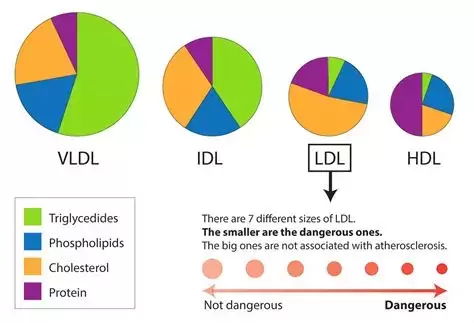
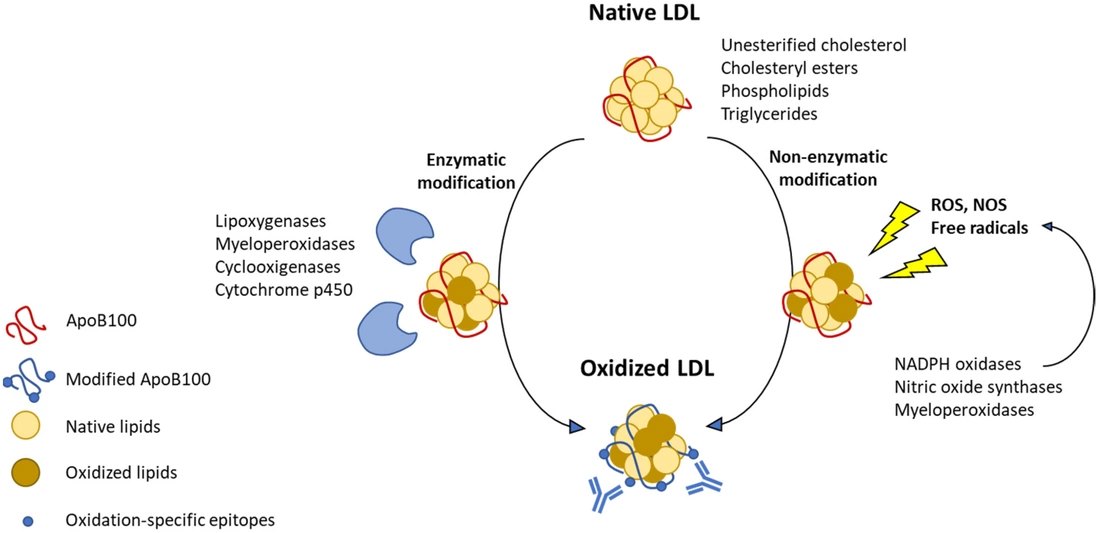
- Low-density lipoprotein (LDL): this is the so-called "bad" cholesterol, which has been reported to build up in arteries, forming plaque, narrowing blood flow, making the vessels stiffer - this is known as atherosclerosis. If a clot forms in these narrow passages, it could prevent the flow of oxygenated blood to the heart cells, leading to a heart attack. It is important to realize that LDL has only been demonstrated to be harmful if it is oxidized (49), which can be modified by antioxidants.50 Additionally, it has been demonstrates that LDL particles rich in polyunsaturated fatty acids (namely foods rich in omega-6 fatty acids, such as industrially processed vegetable oils, including corn, soy, canola, sunflower, safflower, and even olive) are more readily oxidized than LDL particles enriched in saturated fatty acids.50
Other compounds to be aware of when weighing the risk of heart disease include:
Nearly everyone has been warned of the effect that high levels of triglycerides, total cholesterol, and LDL, however not many consider the effect of having too low of levels, which can lead to poor health outcomes.
- Triglycerides: When combining three fatty acids to glycerol, you get a triglyceride. High triglyceride levels have been demonstrated to be caused by consuming excess sugar, sedentary behavior, smoking, excessive alcohol intake, and being overweight or obese.
- Very low-density lipoproteins (VLDL): Unheard of to most, these particles are responsible for dispersing the triglycerides the liver creates. Adding particle size to a cholesterol lab test can determine liver and pancreatic function. Size matters!
- Intermediate-density lipoproteins (IDL): These chylomicrons are formed by the breakdown of VLDL and LDL in the liver. IDLs are reported to be significant risk factors for coronary heart disease and stroke.¹⁰
- Triglyceride-rich-lipoprotein (TRL): Researchers has observed that higher levels of TRL are associated with increased risk for adverse cardiovascular events.¹¹
- Lipoprotein (a), or Lp(a): Lp(a) is made up of LDL plus apo-protein a. High levels of Lp(a) indicate a high risk of heart disease, however Lp(a) levels appear to be hardly examined in common lab tests.
- Apolipoprotein E (Apo-E): This multifunctional protein has central roles in lipid metabolism, neurobiology, and neurodegenerative diseases. It also functions to bind lipoproteins in plasma and the fluid between cells. In other words, it functions to distribute fats among various tissues and cells.¹² Similar to Apo-E exists Apo-B and Apo-A, both of which are better predictors of heart attacks than total cholesterol and LDL.¹³
- Trimethylamine N-oxide (TMAO): If you have a dysregulated gut microbiome you may want to be be concerned with this compound, which, with high levels, has been demonstrated to high risk factor of serious adverse cardiovascular events, as well as all-cause mortality.51 Fortunately, this compound can be offset with modification of nutrition, including modifying gut bacteria and consuming garlic.52
Nearly everyone has been warned of the effect that high levels of triglycerides, total cholesterol, and LDL, however not many consider the effect of having too low of levels, which can lead to poor health outcomes.
Total Cholesterol is not inherently indicative of heart disease risk
In 1985, the National Heart, Lung and Blood Institute initiated the National Cholesterol Education Program (NCEP) which advised adults to monitor cholesterol levels every five years¹⁴, and in turn attempt to bring their levels into the acceptable range.
At this time, only those who had cholesterol levels greater than 260 mg/dL were considered high risk for heart disease.¹⁵ Today, the American Heart Association (AHA) states the optimal total cholesterol is about 150 mg/dL.¹⁶ Thirty years ago, that recommendation was to be under 200 mg/dL.¹⁷ Despite these changes, heart disease remains the leading cause of death¹⁸, as it has for decades.¹⁹
While it is important to realize that cholesterol is one piece of the puzzle, it is not uncommon for individuals with low heart disease risk to have cholesterol levels over 200, due to the levels of HDL. Conversely, individuals with a high risk of heart disease may test with cholesterol levels under 200 mg/dl. It is important to consider the effect of other test levels including HDL when predicting risk of heart disease. Not to mention, these are still guidelines and there is much more that goes into predicting risk of harm.
At this time, only those who had cholesterol levels greater than 260 mg/dL were considered high risk for heart disease.¹⁵ Today, the American Heart Association (AHA) states the optimal total cholesterol is about 150 mg/dL.¹⁶ Thirty years ago, that recommendation was to be under 200 mg/dL.¹⁷ Despite these changes, heart disease remains the leading cause of death¹⁸, as it has for decades.¹⁹
While it is important to realize that cholesterol is one piece of the puzzle, it is not uncommon for individuals with low heart disease risk to have cholesterol levels over 200, due to the levels of HDL. Conversely, individuals with a high risk of heart disease may test with cholesterol levels under 200 mg/dl. It is important to consider the effect of other test levels including HDL when predicting risk of heart disease. Not to mention, these are still guidelines and there is much more that goes into predicting risk of harm.
In fact, it wasn't until the word spread that total cholesterol is a poor predictor of heart disease that HDL and LDL cholesterol were even brought into the picture. And even then, these are just markers which do not reveal the whole picture.
Is heart disease caused by low cholesterol?
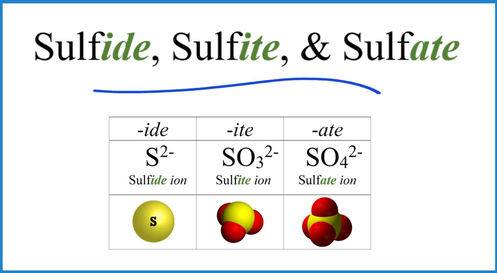
It has been proposed that heart disease is principally a cholesterol sulfate deficiency problem and, more generally, a sulfate deficiency problem.²⁰, 37
For sake of clarity, sulfur is the atom. It's actually the guy in the periodic table, very simple, just 1 sulfur atom - it's like hydrogen or oxygen. Sulfate is a derivative of sulfur, but it includes 4 oxygen atoms, plus a negative two charge.
Yes, sulfur deficiency is a problem in our diet, but, worse than that, we have toxic chemicals that are messing up our body's ability to make the sulfate, to transport the sulfate and it's causing sulfate loss at the kidneys. We're basically running dry on sulfate. This is a contributing factor to the rampant rates of chronic disease in the population.
For sake of clarity, sulfur is the atom. It's actually the guy in the periodic table, very simple, just 1 sulfur atom - it's like hydrogen or oxygen. Sulfate is a derivative of sulfur, but it includes 4 oxygen atoms, plus a negative two charge.
Yes, sulfur deficiency is a problem in our diet, but, worse than that, we have toxic chemicals that are messing up our body's ability to make the sulfate, to transport the sulfate and it's causing sulfate loss at the kidneys. We're basically running dry on sulfate. This is a contributing factor to the rampant rates of chronic disease in the population.
If the supposition is correct, atherosclerosis results from a deficiency in a critical nutrient, cholesterol sulfate, and that the build up of materials that stick to the walls of arteries is a spot where cells of the artery walls, immune cells, and platelets collaborate to produce cholesterol sulfate from homocysteine and oxidized LDL. This underlying deficiency in cholesterol sulfate, due principally to insufficient dietary sulfur and inadequate sun exposure to the skin, leads, over time, to severe depletion of cholesterol and sulfate in the tissues. This deficiency becomes life-threatening with age, and atherosclerotic plaque is a well-choreographed program for renewal of cholesterol sulfate. Unfortunately, there is necessarily collateral damage from superoxide exposure, as superoxide is required to oxidize the LDL and to catalyze the reaction that produces sulfate from homocysteine.37
Worldwide geographical data show an inverse relationship between cardiovascular disease and annual sunlight availability 44. However, placebo-controlled trials failed to show any benefit from vitamin D3 supplementation (45), as opposed to direct sunlight exposure. It is suggested that the cardiovascular benefit comes from cholesterol sulfate synthesis(37), due to direct sunlight exposure.
Worldwide geographical data show an inverse relationship between cardiovascular disease and annual sunlight availability 44. However, placebo-controlled trials failed to show any benefit from vitamin D3 supplementation (45), as opposed to direct sunlight exposure. It is suggested that the cardiovascular benefit comes from cholesterol sulfate synthesis(37), due to direct sunlight exposure.
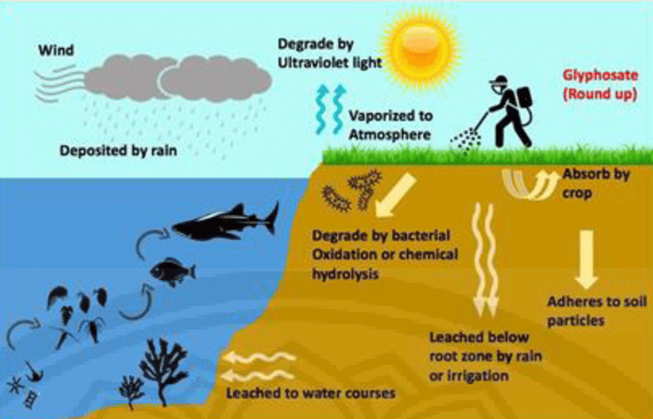
The Connection to Pesticides
Sulfate plays a role in cholesterol regulation and distribution.23 Part of the problem, as elucidated by Stephanie Seneff, is that we're all being chronically poisoned by glyphosate every day. Glyphosate has been demonstrated to disrupt liver function. It's messing up the liver specifically to interfere with its ability to make cholesterol sulfate. That's where the problem starts. The liver is forced to send the cholesterol out as these LDL particles because it cannot distribute the cholesterol as cholesterol sulfate.
Glyphosate is everywhere - it is present in rain water, in soil systems, in organic foods, in rivers and water supplies, the fields of local parks, in the air, and even petroleum car exhaust! Glyphosate, when exposed to fungus, has even been demonstrated to increase the level of mycotoxins, 24 and as it turns out, these mycotoxins have been demonstrated to increase circulating cholesterol levels, among other pathological effects, including neurotoxicity.25
In fact, glyphosate not only disrupts the gut (26), cytochrome P450 enzymes (27), and the skin (28) - a perfect storm to stifle one's natural ability to protect yourself from the sun. And it turns out that cholesterol sulfate is made in huge amounts by the skin (29), which is a large contributing supplying to the body, but that mechanism depends upon the sunlight exposure.
An important factor to consider is glyphosate is a lipophilic neurotoxins.30 These are fat-loving toxins that dissolve like food coloring into water, but these toxins are dissolving into your fat, including the fat in your membranes and into your cholesterol and your bile, and they can recirculate and permeate your system. So essentially, cholesterol levels can be higher due to fat-soluble toxic compounds that blend with cholesterol, including glyphosate residue, but glyphosate is never measured. In fact, there has been a observed relationship between glyphosate and glyphosate.31, 32
Glyphosate is everywhere - it is present in rain water, in soil systems, in organic foods, in rivers and water supplies, the fields of local parks, in the air, and even petroleum car exhaust! Glyphosate, when exposed to fungus, has even been demonstrated to increase the level of mycotoxins, 24 and as it turns out, these mycotoxins have been demonstrated to increase circulating cholesterol levels, among other pathological effects, including neurotoxicity.25
In fact, glyphosate not only disrupts the gut (26), cytochrome P450 enzymes (27), and the skin (28) - a perfect storm to stifle one's natural ability to protect yourself from the sun. And it turns out that cholesterol sulfate is made in huge amounts by the skin (29), which is a large contributing supplying to the body, but that mechanism depends upon the sunlight exposure.
An important factor to consider is glyphosate is a lipophilic neurotoxins.30 These are fat-loving toxins that dissolve like food coloring into water, but these toxins are dissolving into your fat, including the fat in your membranes and into your cholesterol and your bile, and they can recirculate and permeate your system. So essentially, cholesterol levels can be higher due to fat-soluble toxic compounds that blend with cholesterol, including glyphosate residue, but glyphosate is never measured. In fact, there has been a observed relationship between glyphosate and glyphosate.31, 32
It's not only glyphosate that is the problem, it's all toxins. It is well established that our environment is inundated with harmful compounds that disrupt our health, including heart health. 38, 39
Fortunately, there are ways to support the body in detoxifying glyphosate, as well as other toxic compounds, and thereby reducing the overall fat storage, including the value of total cholesterol, thus improving heart disease risk and overall quality of life. The fat is being stored in the fat cells, especially fat stored around organs, often is exacerbated because it's harboring these toxic chemicals.33, 34
The quest is to repair the body, that is the gut, liver, and overall metabolism, by supporting it's innate detoxification capabilities. This occurs by eating your sulfur-containing foods, eating 100% organic, whole foods, thereby making sure you have a high micronutrient content in your food, and getting lots of minerals and vitamins to support detoxification pathways.
Fortunately, there are ways to support the body in detoxifying glyphosate, as well as other toxic compounds, and thereby reducing the overall fat storage, including the value of total cholesterol, thus improving heart disease risk and overall quality of life. The fat is being stored in the fat cells, especially fat stored around organs, often is exacerbated because it's harboring these toxic chemicals.33, 34
The quest is to repair the body, that is the gut, liver, and overall metabolism, by supporting it's innate detoxification capabilities. This occurs by eating your sulfur-containing foods, eating 100% organic, whole foods, thereby making sure you have a high micronutrient content in your food, and getting lots of minerals and vitamins to support detoxification pathways.
New heart Risk 'CAlculator' puts more people than ever on statins
In 2013, the AHA changed the prescribing guidelines for cholesterol treatment.40 Before this change, doctors would rely on levels of total cholesterol and triglycerides to determine whether or not someone was fit for consuming statins.
Today, physicians rely on a "risk calculators" to estimate your overall risk of heart disease, which accounts for various factors including your age, sex, race, cholesterol, blood pressure, metabolic static, pharmacologic drug consumption, and certain habits.41
While this method of determining risk isn't inherently incorrect, the algorithm led to controversy as statins were then prescribed to a whole new group of people who never had symptoms of cardiovascular disease. If healthcare providers follow these new guidelines, as many as 59 percent more women and 47 percent more men will be taking statins than if they had been diagnosed under the old guidelines - it has been estimated that the number of people eligible for statins under these new guidelines increased by 56 million in the United States.42
Today, physicians rely on a "risk calculators" to estimate your overall risk of heart disease, which accounts for various factors including your age, sex, race, cholesterol, blood pressure, metabolic static, pharmacologic drug consumption, and certain habits.41
While this method of determining risk isn't inherently incorrect, the algorithm led to controversy as statins were then prescribed to a whole new group of people who never had symptoms of cardiovascular disease. If healthcare providers follow these new guidelines, as many as 59 percent more women and 47 percent more men will be taking statins than if they had been diagnosed under the old guidelines - it has been estimated that the number of people eligible for statins under these new guidelines increased by 56 million in the United States.42
New Guidelines - Thousands of children on statins
In 2012, the National Heart, Lung, and Blood Institute (NHLBI), teamed with the National Institutes of Health and the US Department of Health and Human Services, to create new guidelines for heart health and risk with respect to children.43
Under these guidelines, it is admitted that children will require pharmacologic therapy. While this is not that surprising if one looks at the quality of the standard American diet and lifestyle, especially of children, adhering to these pediatric guidelines means that an additional 483,500 young people, as early as 8 years old, with elevated LDL levels would qualify for taking statins, compared to the 78,200 that was determined based on the previous guidelines.46
These numbers are so appalling that cardiologists at Boston Children's hospital decided it was necessary to publicly reaffirm that it is in the best interest of individuals to "clearly address other modifiable risk factors", such as diet and exercise, before actually consuming statins or other pharmacologic drugs. Dr. Suzanne Steinbaum, a cardiologist at Lenox Hill Hospital in New York City stated, "Medication should be the last resort and a true behavioral and healthy lifestyle program should be implemented... Regardless of the guidelines, we need to not have this younger generation rely on medication, but instill in them what healthy food choices, exercise and smoking cessation means before simply giving them a pill."47
You might be asking yourself, "well, what's so wrong about statins?" Simply considering the serious and direct side effects of statins (including cardiomyopathy, diabetes, and many other conditions), not to mentioned the use and side effects of drugs to counteract those side effects, it is difficulty to imagine how statins could be justified at all in children, especially considering that elevated cholesterol is modifiable with basic lifestyle, nutrition, and movement practices.
Under these guidelines, it is admitted that children will require pharmacologic therapy. While this is not that surprising if one looks at the quality of the standard American diet and lifestyle, especially of children, adhering to these pediatric guidelines means that an additional 483,500 young people, as early as 8 years old, with elevated LDL levels would qualify for taking statins, compared to the 78,200 that was determined based on the previous guidelines.46
These numbers are so appalling that cardiologists at Boston Children's hospital decided it was necessary to publicly reaffirm that it is in the best interest of individuals to "clearly address other modifiable risk factors", such as diet and exercise, before actually consuming statins or other pharmacologic drugs. Dr. Suzanne Steinbaum, a cardiologist at Lenox Hill Hospital in New York City stated, "Medication should be the last resort and a true behavioral and healthy lifestyle program should be implemented... Regardless of the guidelines, we need to not have this younger generation rely on medication, but instill in them what healthy food choices, exercise and smoking cessation means before simply giving them a pill."47
You might be asking yourself, "well, what's so wrong about statins?" Simply considering the serious and direct side effects of statins (including cardiomyopathy, diabetes, and many other conditions), not to mentioned the use and side effects of drugs to counteract those side effects, it is difficulty to imagine how statins could be justified at all in children, especially considering that elevated cholesterol is modifiable with basic lifestyle, nutrition, and movement practices.
The neutrality of Cholesterol
It was more than 50 years ago when the Framingham study set the stage for demonized high cholesterol as the source of heart disease, and that consuming cholesterol and saturated fat was to blame.48
However, it is argued by Dr. Fred Kummerow - a biochemist and food scientist who pioneered the interaction of lipids, cholesterol, heart disease and nutrition for over seven decades - that it is not cholesterol that causes heart disease. His fight to ban trans fats is a testimony to the fact that trans fat are the blame for increased rates of heart disease. Indeed, trans fats can cause blood clots in the arteries, leading to sudden cardiac death. 53 Cholesterol in food is not the same as cholesterol in the blood. Cholesterol in the blood is a sign, a marker, a messenger, but it's not the source of harm.
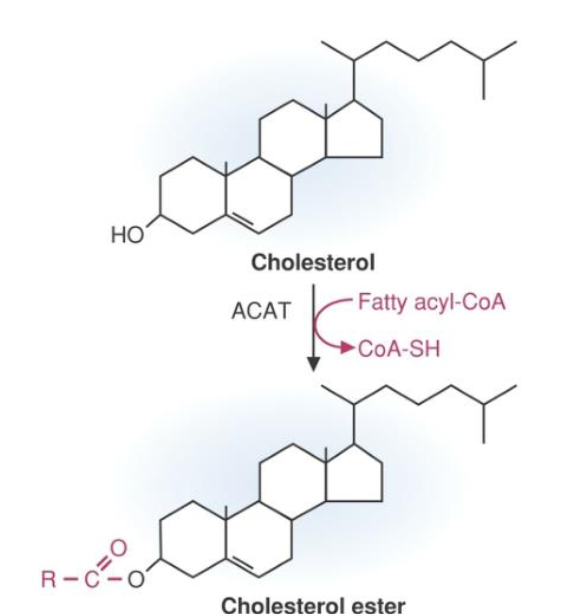
In fact, the food you eat which may be high in cholesterol does not increase blood cholesterol levels due to a process known as esterification. The cholesterol-rich foods you eat have an attached ester group, which prevent a large majority of cholesterol from integrated in the blood, via the Niemann-Pick C1-Like 1 (NPC1L1) transporter found on the gastrointestinal tract, which serves as a checkpoint to regulate cholesterol. Some (10-15%) of the dietary cholesterol is de-esterified and integrated into the body, but it represents a small fraction of the entire pool of the body's cholesterol.56
During his years of work, Dr. Kummerow had made it abundantly clear that cholesterol isn't good or bad and, in fact, should be respected as a vital aspect of overall health and vitality.
However, it is argued by Dr. Fred Kummerow - a biochemist and food scientist who pioneered the interaction of lipids, cholesterol, heart disease and nutrition for over seven decades - that it is not cholesterol that causes heart disease. His fight to ban trans fats is a testimony to the fact that trans fat are the blame for increased rates of heart disease. Indeed, trans fats can cause blood clots in the arteries, leading to sudden cardiac death. 53 Cholesterol in food is not the same as cholesterol in the blood. Cholesterol in the blood is a sign, a marker, a messenger, but it's not the source of harm.
In fact, the food you eat which may be high in cholesterol does not increase blood cholesterol levels due to a process known as esterification. The cholesterol-rich foods you eat have an attached ester group, which prevent a large majority of cholesterol from integrated in the blood, via the Niemann-Pick C1-Like 1 (NPC1L1) transporter found on the gastrointestinal tract, which serves as a checkpoint to regulate cholesterol. Some (10-15%) of the dietary cholesterol is de-esterified and integrated into the body, but it represents a small fraction of the entire pool of the body's cholesterol.56
During his years of work, Dr. Kummerow had made it abundantly clear that cholesterol isn't good or bad and, in fact, should be respected as a vital aspect of overall health and vitality.
Evolution of Cholesterol as a measure of heart health
It was in his book published in 2014 where Dr. Kummerow explains how cholesterol became the enemy. He highlights that the hypothesis of high cholesterol as a major risk factor in heart disease originated in 1906, as well as the flaw in this hypothesis being noted in the Framingham study forty years later.
But the flaws were ignored, and the anti-cholesterol campaigns continued to grow, thereby obstructing progress in determining the source of heart disease.
Treating cholesterol numbers became the focus of managing heart disease, and after the advent of statins, they became to go-to tool for modifying symptoms of high cholesterol. In this time, partially hydrogenated vegetable oils - introduced in 1911 in the form of shortening - became widely available, thereby increasing the rates of trans fats of consumers.
To make matter worse, cookbooks were rewritten to replace butter and lard with shortening. Processed foods were made with this "revolutionary" ingredient. It was selected as a preferred oil in the process of deep-fried foods due to its high smoke point and cost-effective price.
Today, thanks for Dr. Kummerow, we are well aware of the dangers of trans fats, and in turn their consumption is limited. But it took nearly a century for the FDA to finally recognize the harms of these ingredients.
But the flaws were ignored, and the anti-cholesterol campaigns continued to grow, thereby obstructing progress in determining the source of heart disease.
Treating cholesterol numbers became the focus of managing heart disease, and after the advent of statins, they became to go-to tool for modifying symptoms of high cholesterol. In this time, partially hydrogenated vegetable oils - introduced in 1911 in the form of shortening - became widely available, thereby increasing the rates of trans fats of consumers.
To make matter worse, cookbooks were rewritten to replace butter and lard with shortening. Processed foods were made with this "revolutionary" ingredient. It was selected as a preferred oil in the process of deep-fried foods due to its high smoke point and cost-effective price.
Today, thanks for Dr. Kummerow, we are well aware of the dangers of trans fats, and in turn their consumption is limited. But it took nearly a century for the FDA to finally recognize the harms of these ingredients.
Lowering Cholesterol does not inherently improve heart disease risk
Simply put, the right amount of cholesterol will vary based on the individual. It is clear that the medical establishment and public laymen have an overly simplistic view of cholesterol that leads to the believe that lowering cholesterol will lower heart disease risk. The types of cholesterol are important variables to consider, as well as type of fat consumption.
Even the idea that LDL is "bad" is incorrect. What matters most is if the LDL particles have been oxidized. Cholesterol has no impact of heart disease, unless it is has been oxidized, at which point it becomes an oxysterol. Oxidation can be caused by excess exposure to light and heat, as well as other physiologic processes, causing those LDL particles to become destructive.
Even the idea that LDL is "bad" is incorrect. What matters most is if the LDL particles have been oxidized. Cholesterol has no impact of heart disease, unless it is has been oxidized, at which point it becomes an oxysterol. Oxidation can be caused by excess exposure to light and heat, as well as other physiologic processes, causing those LDL particles to become destructive.
So if cholesterol isn't the culprit causing heart disease, what is? As mentioned it's cholesterol that has been oxidized that causes harm. More specifically, oxidized cholesterol can increase thromboxane formation, a compound that can result in blood clots. Thromboxane (facilitates blood clotting) works antagonistically to prostacyclin (facilitates blood flow). It is ideal to monitor the ratio of these compounds, because small changes can result in big effects.
A big component to eliminate from the diet that is responsible for heart disease is trans fat found in partially hydrogenated oils. Hydrogenated oils are created to increase the shelf life of processed food-like products.
A big component to eliminate from the diet that is responsible for heart disease is trans fat found in partially hydrogenated oils. Hydrogenated oils are created to increase the shelf life of processed food-like products.
Cholesterol is your friend
As mentioned, regular consumption of foods that are rich in cholesterol (organic, pasture-raised butter, beef, eggs) does not inherently increase your risk of heart disease. That is why cholesterol and saturated fat-rich animal foods are featured in my Integral Nutrition Program. Many of the healthiest foods also happen to be rich in cholesterol and saturated fats. Like cholesterol, saturated fat has also been wrongly vilified. In fact, several independent meta-analyses performed concluded that there is no significant evidence that the consumption of saturated fat is associated with an increased risk for cardiovascular disease.57, 58, 59
Furthermore, researchers have observed that ramping up the consumption of saturated fat by double or triple the recommended daily allowance does not translate to increased blood levels of saturated fat. However, increased consumption of carbohydrates reliably increases blood levels. 60
There is no way to determine how many people have been negatively affected by the decades of dogmatic propaganda regarding the thought that saturated fat is harmful to your heart, especially when there are data suggesting that a lack of healthy fat actually increases your risk of cardiovascular disease. 61
Furthermore, researchers have observed that ramping up the consumption of saturated fat by double or triple the recommended daily allowance does not translate to increased blood levels of saturated fat. However, increased consumption of carbohydrates reliably increases blood levels. 60
There is no way to determine how many people have been negatively affected by the decades of dogmatic propaganda regarding the thought that saturated fat is harmful to your heart, especially when there are data suggesting that a lack of healthy fat actually increases your risk of cardiovascular disease. 61
Relationship to Inflammation
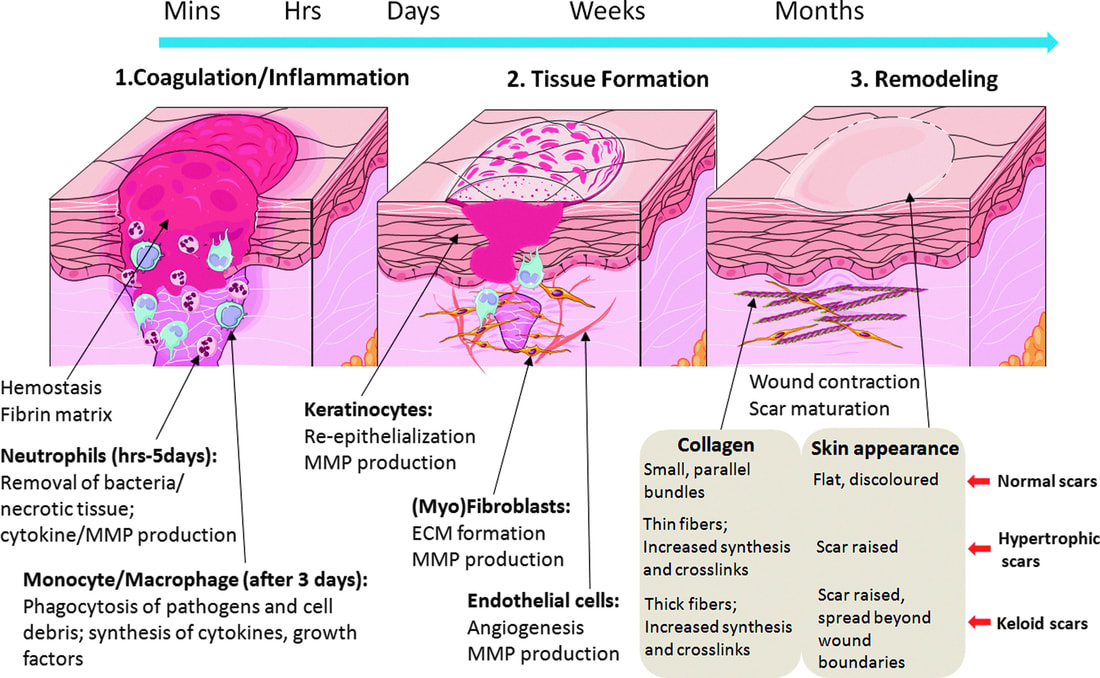
Inflammation is a double-edged sword. It isn't inherently bad, as it serves a role. The positive function of inflammation is to serve as a signal to trigger healing.
Consider the following example: You go to the gym for leg day. After your warmup, you get your squats in and work up to hit your personal best record. You move to some other exercises and finish up with some balance. On the way out, it's dark and you're fatigued, not seeing the step on the way out, you trip and scrape your knee resulting in a small open wound.
Now, that there are two bouts of inflammation in the aforementioned example. The first is that open wound knee, which is going to trigger an immediate immune response as your body's natural way of dealing with threats to your health, such as antigens from bacteria, fungi, chemicals, toxins, or foreign substances. The second is the workout you just performed - the muscle fibers from the squats literally have microtears, like the skin from the open wound. In both scenarios you will use inflammation to trigger healing. One is a "positive" form of stress, exercise, and the other is a "negative" form of stress, the open wound.
Consider the following example: You go to the gym for leg day. After your warmup, you get your squats in and work up to hit your personal best record. You move to some other exercises and finish up with some balance. On the way out, it's dark and you're fatigued, not seeing the step on the way out, you trip and scrape your knee resulting in a small open wound.
Now, that there are two bouts of inflammation in the aforementioned example. The first is that open wound knee, which is going to trigger an immediate immune response as your body's natural way of dealing with threats to your health, such as antigens from bacteria, fungi, chemicals, toxins, or foreign substances. The second is the workout you just performed - the muscle fibers from the squats literally have microtears, like the skin from the open wound. In both scenarios you will use inflammation to trigger healing. One is a "positive" form of stress, exercise, and the other is a "negative" form of stress, the open wound.
Without the inflammation, the cascade of physiologic events would not occur to result in healing. The five characteristics of inflammation include discomfort, redness, swelling, heat and impaired function. But these characteristics exist for a reason, as blood rushing toward these areas are providing nutrients and cofactors for clotting, and improved immune function. The impaired function serves as a form of immobilization to protect the region to facilitate healing. Eventually each of these processes leads to an end-stage. In the case of the wound, a scar, and in the case of the squats, increased strength. Our body's are designed to handle brief bouts of inflammation and stress as it makes us stronger. However, it is when this stress become chronic and unchecked when problems begin to set in.
Cholesterol comes into the picture in an effort to replace the damaged cells. If you recall, one of cholesterols main function is to support the structural integrity of cell membranes. No cell can form without cholesterol. The damaged cells desired to be replaced by the body results in a trigger to the liver to create more cholesterol and release it into the bloodstream. This is a very intentional process for the body to produce new, healthy cells. Additionally, it's not only possible, but very common for internal damage to occur in the body on a regular basis. This damage results in a state of chronic, low grade inflammation.80
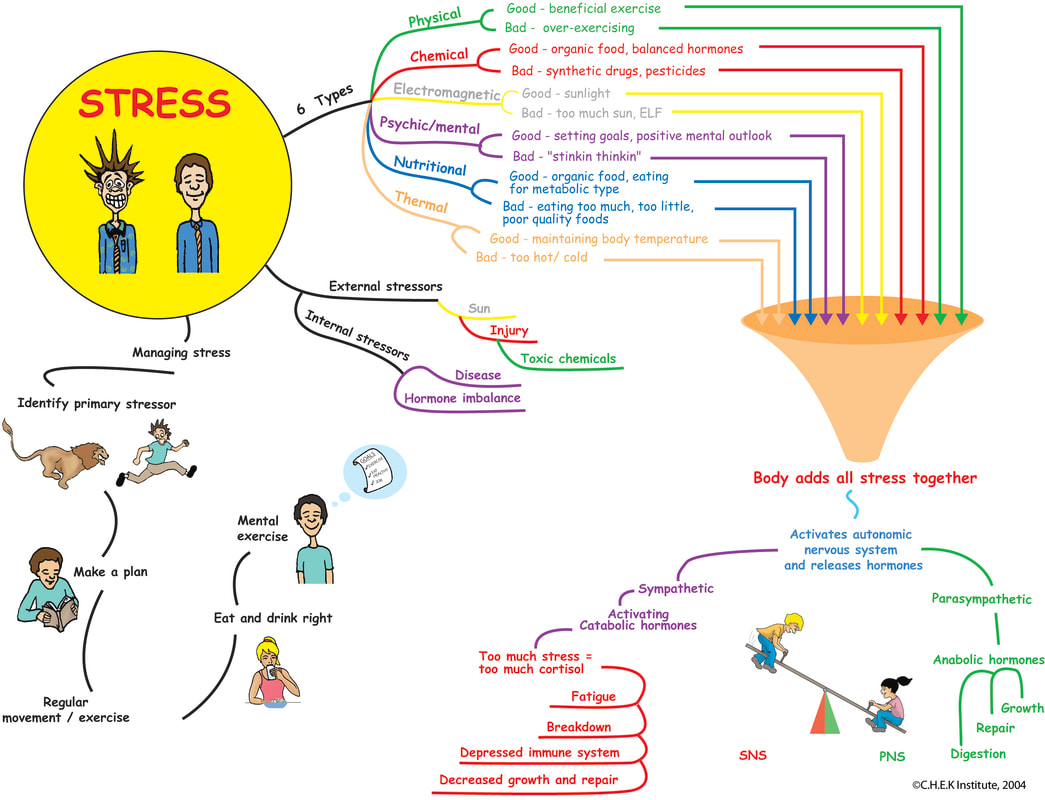
This chronic low-grade inflammation has been observed to be caused by various factors, including but not limited to:
It is in your best interest to address these factors (and many others) if you are interested in lowering your risk of heart disease by way of balancing cholesterol and inflammation. However, before treating this inflammation, it would be ideal to identify how much inflammation is present. This can be achieved with a lab test to detect the amount of high-sensitivity C-reactive protein (hsCRP), which measures the amount of inflammation in arteries.
The following table displays hsCRP levels with the corresponding risk of cardiovascular disease (82):
- Oxidized cholesterol (such as foods high in cholesterol that are cooked in high temperatures, or prolonged exposure to light)
- Excessive consumption of sugars and grains
- Consumption of processed foods, many of which contains trans fats
- Exposure to pesticides via the consumption of convention crops or administration of pesticides, such as glyphosate81
- Lack of sleep or low quality sleep
- Sedentary lifestyle
- Smoking
- High levels of stress (physical, mental, emotional, chemical, thermal, electromagnetic)
- Chronic infections
- Obesity
It is in your best interest to address these factors (and many others) if you are interested in lowering your risk of heart disease by way of balancing cholesterol and inflammation. However, before treating this inflammation, it would be ideal to identify how much inflammation is present. This can be achieved with a lab test to detect the amount of high-sensitivity C-reactive protein (hsCRP), which measures the amount of inflammation in arteries.
The following table displays hsCRP levels with the corresponding risk of cardiovascular disease (82):
Low Risk |
Intermediate Risk |
High Risk |
< 1 mg/L |
1 - 3 mg/L |
> 3 mg/L |
It is no secret that chronic inflammation can increase the risk of heart disease and result in heart attacks.83 But conventional medicine stops short of seeing the big picture. In the eyes of conventional medicine, it’s only when increased cholesterol circulating in your bloodstream is observed that they conclude that cholesterol—not the underlying damage to your arteries—is the cause of heart attacks.
High cholesterol: An Invented disease
Sally Fallon Morell, president of the Weston A. Price Foundation, and Mary Enig, Ph.D, an expert in lipid biochemistry, were among the first beyond Dr. Kummerow to call high cholesterol “an invented disease, a ‘problem’ that emerged when health professionals learned how to measure cholesterol levels in the blood.”84
Since then, this explanation still holds true. As mentioned, increased levels of cholesterol reveal increased systemic inflammation. Cholesterol serves a role, and it is elevated for a reason: to help the body heal and recover.
Since the onset of the cholesterol myth, the pharmaceutical industrial complex has missed the boat as they continue to dangerously
recommended lowering cholesterol in an effort to reduce the risk of heart attacks, when what was actually needed was to address the underlying root cause of the inflammation.
Since then, this explanation still holds true. As mentioned, increased levels of cholesterol reveal increased systemic inflammation. Cholesterol serves a role, and it is elevated for a reason: to help the body heal and recover.
Since the onset of the cholesterol myth, the pharmaceutical industrial complex has missed the boat as they continue to dangerously
recommended lowering cholesterol in an effort to reduce the risk of heart attacks, when what was actually needed was to address the underlying root cause of the inflammation.
Dangers of Cholesterol deficiency
Indeed, low cholesterol can harm your health and quality of life. Various scientific inquires have led to the discovery of the following findings:
- Cholesterol is needed to prevent hemorrhagic stroke: There are two types of stroke: 1) Ischemic, associated with lack of oxygenated blood flow to the brain; 2) Hemorrhagic, associated with the rupture of a blood vessel in the brain resulting in bleeding. The risk for ischemic strokes could be raised in the presence of excessive oxidized cholesterol. However, it is the risk for the second, hemorrhagic stroke, which is increased when cholesterol levels are low. Researchers have observed "The only cause of death attributable to low serum cholesterol concentration was hemorrhagic stroke." 64
- Cholesterol is needed to prevent aggression: Cholesterol is a precursor of serotonin. Serotonin has a function in the central nervous system to suppress harmful behavior impulses. Low membrane cholesterol decreases the number of serotonin receptors. Since membrane cholesterol exchanges freely with cholesterol, a lowered serum cholesterol concentration may contribute to a decrease in brain serotonin, with poorer suppression of aggressive behavior (especially under the influence of alcohol).62, 63
- Cholesterol helps us fight infection: Researchers have observed low levels of cholesterol result in insufficient immune function.67 In fact, cholesterol serves a crucial role for lytic mechanism (breakdown of cells via immune surveillance).68 Additionally, cholesterol-rich diets have been observed to improve the outcomes of patients with tuberculosis, leading researchers to suggest "cholesterol should be used as a complementary measure in antitubercular treatment."70 Cholesterol-lowering drugs, incidentally, exhibit immunosuppressive (67) and potent immunotoxic properties (71,72,73), likely in part due to their cholesterol depleting effects.
- Cholesterol is needed to fight cancer: There is a clear inverse relationship between cholesterol levels and the risk for a variety of cancers, and mortality associated with cancer.65 Whether temporal or causal, this relationship continues to be observed.66 A likely mechanism underlying the potential causal relationship is due to the aforementioned insufficient immune function.67 Researchers have even taken the so-called "bad" LDL-cholesterol and administered it to a culture of highly malignant, multi-drug resistant leukemia cells, and observe the cells lose their resistance to chemotherapy.69
- Cholesterol is needed for memory: Low HDL cholesterol has been identified as a risk factor for deficit and decline in memory in middle aged adults.74 Even in Parkinson's disease, higher total serum cholesterol concentrations are associated with slower clinical progression of the disease, as cholesterol is involved in a plethora of critical biological functions ranging from cellular repair or degeneration to being a neurosteroid precursor.75 Statin drugs, which inhibit the production of cholesterol, hence severely affecting the brain, are now required by the FDA to display the black box warning that they may adversely affect the memory.76 Over 50 studies from the National Library of Medicine's bibliographic database, Medline, have been indexed on the neurotoxicity of statin drugs77, with six of these specifically addressing statin-induced memory impairment.78
- Cholesterol is needed for longevity: Researchers have observed a fascinating relationship between telomere length - the shoestring cap-like ends of the chromosomes which prevent DNA damage associated with cellular aging - with higher LDL and total cholesterol levels. The longer the length of these protective caps, the higher the cholesterol.79 This study among others indicate that lower cholesterol is associated with increased mortality.
Dangers of Statins
The data compiled on the dangers of statin administration is overwhelming and compelling. Statins have been demonstrated to result in various degrees of toxicity affecting multiple organ systems and cell types. To date there have been 30 adverse pharmacological actions researched for statin drugs (HMG-CoA reductase inhibitors), in order of highest available evidence²¹, including:
A huge concern with the consumption of statins is the disrupted effect on coenzyme Q10 (CoQ10).35 CoQ10 is essential for mitochondrial function (there is an enormous concentration of mitochondria in heart cells), and deficiencies of this important compound has been linked to neurologic and muscle impairments, including the heart muscle. CoQ10 protects the heart from failure. In fact, low concentrations of CoQ10 is independently linked to adverse heart health outcomes, and it turns out that there is a inverse relationship between CoQ10 and LDL.36
Due to the affected mechanisms listed above, over 300 abnormal side effects, health outcomes, disorders and diseases have been connected to the consumption of statins²², including but not limited to:
- Myotoxic (muscle, including cardiac muscle)
- Neurotoxic (nerve)
- Hepatotoxic (liver)
- Carcinogenic (cancer)
- Endocrine disruptor: (hormone) insulin resistance, testes, thyroid, ovary, pancreas
- Diabetogenic
- Cardiotoxic
- Nephrotoxic (kidney)
- Immunotoxic
- Cytotoxic (cell)
- Teratotoxic (birth defects)
- Cataractogenic
- Inflammatory
- Hemorrhagic
- Immunosuppressive
- Arthritic
- Anxiogenic (anxiety)
- Apoptotic (cell death)
- Immunoreactive
- IL-6 up-regulation (inflammation)
- TNFa up-regulation (inflammation)
- Ulcerogenic
- Embryotoxic
A huge concern with the consumption of statins is the disrupted effect on coenzyme Q10 (CoQ10).35 CoQ10 is essential for mitochondrial function (there is an enormous concentration of mitochondria in heart cells), and deficiencies of this important compound has been linked to neurologic and muscle impairments, including the heart muscle. CoQ10 protects the heart from failure. In fact, low concentrations of CoQ10 is independently linked to adverse heart health outcomes, and it turns out that there is a inverse relationship between CoQ10 and LDL.36
Due to the affected mechanisms listed above, over 300 abnormal side effects, health outcomes, disorders and diseases have been connected to the consumption of statins²², including but not limited to:
Statin-Induced Pathologies |
Myopathies |
Chemically-Induced Liver Damage |
High Cholesterol |
Drug-Induced Nutrient Depletion |
Diabetes Mellitus: Type 1 and 2 |
Rhabdomyolysis |
Coenzyme Q10 Deficiency |
Cancers: All |
Coronary Artery Disease |
Cataracts |
Drug-Induced Toxicity |
Oxidative Stress |
Pancreatitis |
Insulin Resistance |
Cardiovascular Diseases |
Hyperlipidemia |
Myalgias |
Peripheral Neuropathies |
|
Cognitive Decline/Dysfunction |
Dyslipidemias |
Creatine Phosphokinase (CK): Elevated |
Testosterone: Too Low |
Vitamin D Deficiency |
Erectile Dysfunction |
Kidney Failure |
Hyperglycemia |
Hypertension |
Aggression |
Autoimmune Diseases |
Low Immune Function |
Depression |
Dietary Fatty Acid Imbalance: Omega 3/6 |
Muscle Soreness |
Eczema |
Insomnia |
Sperm Quality: Low |
Triglycerides: Elevated |
Psychiatric Disorders |
Hypothyroidism |
DNA Damage |
Bone Fractures |
Fatigue |
Infertility: Male |
Inflammation |
Tendon Rupture |
Balance Disorders |
Better Predictors of Heart disease: RHR and HRV
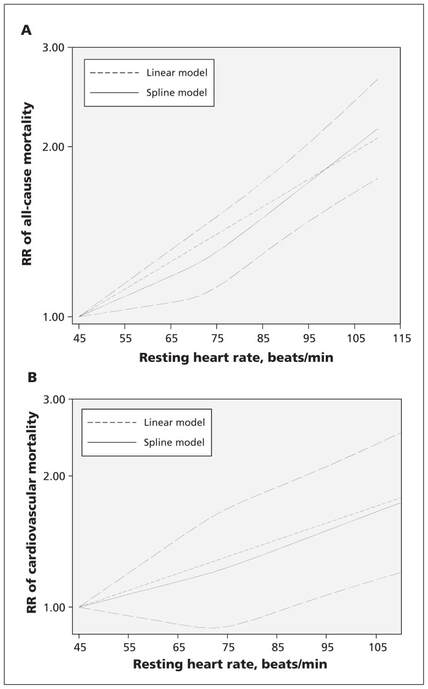
Researchers have concluded there are various factors that can predict heart disease risk fairly accurately, and this includes resting heart rate (RHR) and heart rate variability (HRV).
RHR is a familiar, straightforward and inexpensive-to-measure clinical variable, and it can be modified by a number of factors, such as physical activity, psychologic stress, smoking, intake of omega-3 fatty acids and medications. Higher heart rate has been linked to increased risks of cardiovascular disease and premature mortality through a multitude of actions, including its detrimental effects on progression of coronary atherosclerosis, on occurrence of heart attacks and abnormal arrhythmias, on heart function and on circulating levels of inflammatory markers. The data compiled on RHR suggests that for every increment of 10 beats/minute there is an increase in heart disease mortality by 8%, and an increase in all-cause mortality by 9%. 54
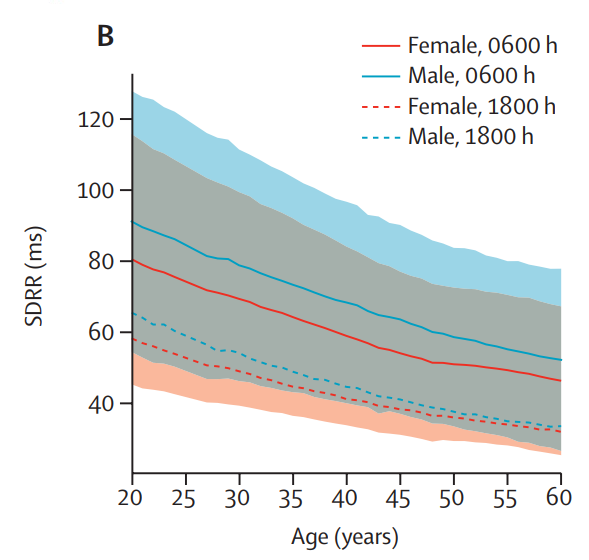
HRV refers to the variation in time between successive heart beats and represents a noninvasive measure of the autonomic nervous system. Because the autonomic nervous system regulates heart rate during normal cardiac rhythm, HRV reveals complex cardiovascular responses, which are dictated by the parasympathetic (rest and relax) and sympathetic (fight or flight) nervous systems, to constantly changing physiological variations. Although HRV is significantly affected by sex and aging, low HRV is independently predictive of cardiovascular disease events in the general population. HRV declines from the ages of 20 years to 60 years, with a decrease in all HRV measures. Robust data also link low HRV with adverse outcomes and mortality after sustaining a cardiovascular event, such as a heart attack. Additionally, diurnal variation of HRV metrics over a 24 h period reveal that HRV metrics vary throughout the day, reaching peak values in the early morning hours.55
RHR is a familiar, straightforward and inexpensive-to-measure clinical variable, and it can be modified by a number of factors, such as physical activity, psychologic stress, smoking, intake of omega-3 fatty acids and medications. Higher heart rate has been linked to increased risks of cardiovascular disease and premature mortality through a multitude of actions, including its detrimental effects on progression of coronary atherosclerosis, on occurrence of heart attacks and abnormal arrhythmias, on heart function and on circulating levels of inflammatory markers. The data compiled on RHR suggests that for every increment of 10 beats/minute there is an increase in heart disease mortality by 8%, and an increase in all-cause mortality by 9%. 54
HRV refers to the variation in time between successive heart beats and represents a noninvasive measure of the autonomic nervous system. Because the autonomic nervous system regulates heart rate during normal cardiac rhythm, HRV reveals complex cardiovascular responses, which are dictated by the parasympathetic (rest and relax) and sympathetic (fight or flight) nervous systems, to constantly changing physiological variations. Although HRV is significantly affected by sex and aging, low HRV is independently predictive of cardiovascular disease events in the general population. HRV declines from the ages of 20 years to 60 years, with a decrease in all HRV measures. Robust data also link low HRV with adverse outcomes and mortality after sustaining a cardiovascular event, such as a heart attack. Additionally, diurnal variation of HRV metrics over a 24 h period reveal that HRV metrics vary throughout the day, reaching peak values in the early morning hours.55
Solutions
Movement: regular exercise (strength training, Zone-2 Cardio) 4x/week, proper breathing mechanics
Nutrition: organic whole foods, appropriate micronutrients (vitamins and minerals), pasture-raised (grass-fed/finished) animal products, RO filtered water
Nutrition: organic whole foods, appropriate micronutrients (vitamins and minerals), pasture-raised (grass-fed/finished) animal products, RO filtered water
- Avoid: processed and conventional foods, vegetable/seed oils, alcohol, gluten, pasteurized dairy, any potential foods contaminated by mycotoxins (raw nuts, grains - sprouted is ideal), fried foods, standard American diet (SAD diet), refined sugar such as high fructose corn syrup, canned foods, food additives such as carrageenan
- Implement: mushrooms, fiber (psyllium, flaxseed, oats), red yeast rice, probiotics, fermented foods, polyphenols (green tea), CoQ10, Cod liver oil, Magnesium, various herbs (garlic, curcumin, ginseng, dill, cardamom, bergamot, amla berry, saffron, thyme, sea buckthorn, turmeric, goldenseal, ashwagandha, bacopa, basil, etc.)
Lifestyle
- Detox (Quarterly 7-day, Daily intermittent)
- Mitigate stress (Mental, physical, chemical, electromagnetic, etc.)
- Get adequate sunshine
- Nature therapy
- Avoid: plastic, statins, insulin, heavy metals, smoking, vaping of glycerin-containing nicotine products
Resources
References
- Prescription cholesterol-lowering medication use in adults aged 40 and Over: United States, 2003–2012. (2014). https://www.cdc.gov/nchs/data/databriefs/db177.pdf
- Wooller, S. (2023, January 12). Now anyone over 18 can get statins! huge shake-up of NHS Drug Guidelines could see doctors give millions more brits the cheap cholesterol-busting pills. Daily Mail Online. https://www.dailymail.co.uk/health/article-11627331/Millions-Brits-statins-health-chiefs-recommendations.html
- Top 10 prescription medications: Most commonly prescribed drugs in the U.S. GoodRx. (2021). https://www.goodrx.com/drug-guide
- USDA, USDHHS. (2010). Dietary guidelines for Americans - health.gov. https://health.gov/sites/default/files/2020-01/DietaryGuidelines2010.pdf
- Healthy School Food. Physicians Committee for Responsible Medicine. (2018). https://www.pcrm.org/good-nutrition/healthy-communities/healthy-school-food
- UCSF Health. (2022, June 24). Guidelines for a low cholesterol, low saturated fat diet. ucsfhealth.org. https://www.ucsfhealth.org/education/guidelines-for-a-low-cholesterol-low-saturated-fat-diet
- USDA. (2015). Scientific Report of the 2015 Dietary Guidelines Advisory Committee. Health.gov. https://health.gov/sites/default/files/2019-09/Scientific-Report-of-the-2015-Dietary-Guidelines-Advisory-Committee.pdf
- Back to eggs and bacon? what new cholesterol guidelines mean to you. Tampa Bay Times. (2015). https://www.tampabay.com/news/health/medicine/back-to-eggs-and-bacon-what-new-cholesterol-guidelines-mean-to-you/2218505/
- Orth, M., & Bellosta, S. (2012). Cholesterol: Its regulation and role in Central Nervous System Disorders. Cholesterol, 2012, 1–19. https://doi.org/10.1155/2012/292598
- Yoshida, H., Ito, K., Manita, D., Sato, R., Hiraishi, C., Matsui, S., & Hirowatari, Y. (2021). Clinical significance of intermediate-density lipoprotein cholesterol determination as a predictor for coronary heart disease risk in middle-aged men. Frontiers in Cardiovascular Medicine, 8. https://doi.org/10.3389/fcvm.2021.756057
- Busko, M. (2015, June 1). Triglyceride-rich-lipoprotein cholesterol predicts CV events. Medscape. https://www.medscape.com/viewarticle/845693?form=fpf
- Huang, Y., & Mahley, R. W. (2014). Apolipoprotein E: Structure and function in lipid metabolism, neurobiology, and alzheimer’s diseases. Neurobiology of Disease, 72, 3–12. https://doi.org/10.1016/j.nbd.2014.08.025
- Walldius, G., Jungner, I., Holme, I., Aastveit, A. H., Kolar, W., & Steiner, E. (2001). High apolipoprotein B, low apolipoprotein A-I, and improvement in the prediction of fatal myocardial infarction (Amoris study): A prospective study. The Lancet, 358(9298), 2026–2033. https://doi.org/10.1016/s0140-6736(01)07098-2
- Centers for Disease Control and Prevention. (2001, May 2). Cholesterol screening and awareness -- behavioral risk factor surveillance system, 1990. https://www.cdc.gov/mmwr/preview/mmwrhtml/00017607.htm
- NIH. (1984). Lowering Blood Cholesterol to Prevent Heart Disease. U.S. Department of Health and Human Services. https://web.archive.org/web/20090604072656/http://consensus.nih.gov/1984/1984Cholesterol047html.htm
- American Heart Association. (2018). Cholesterol Management Guide for Health Care Practitioners. AMGEN. https://www.heart.org/-/media/files/health-topics/cholesterol/cholesterol-guide-for-hc-practitioners-english.pdf
- Johnson, C. L. (1993). Declining serum total cholesterol levels among us adults. JAMA, 269(23), 3002. https://doi.org/10.1001/jama.1993.03500230084034
- Centers for Disease Control and Prevention. (2021). Leading causes of death. https://www.cdc.gov/nchs/fastats/leading-causes-of-death.htm
- Centers for Disease Control and Prevention. (2017). Leading causes of death and numbers of death. https://www.cdc.gov/nchs/data/hus/2017/020.pdf
- Asprey, D. (2013). Dr. Stephanie Seneff: Glyphosate Toxicity, Lower Cholesterol Naturally & Get Off Statins. Bulletproof. https://daveasprey.com/dr-stephanie-seneff-glyphosate-toxicity-lower-cholesterol-naturally-get-off-statins-238/
- Statin drugs. GreenMedInfo. (2017). https://greenmedinfo.com/toxic-ingredient/statin-drugs
- Golomb, B. A., & Evans, M. A. (2008). Statin adverse effects. American Journal of Cardiovascular Drugs, 8(6), 373–418. https://doi.org/10.2165/0129784-200808060-00004
- Strott, C. A., & Higashi, Y. (2003). Cholesterol sulfate in human physiology: What’s it all about? Journal of Lipid Research, 44(7), 1268–1278. https://doi.org/10.1194/jlr.r300005-jlr200
- Reddy, K. N., Abbas, H. K., Zablotowicz, R. M., Abel, C. A., & Koger, C. H. (2007). Mycotoxin occurrence and Aspergillus flavus soil propagules in a corn and cotton glyphosate-resistant cropping systems. Food Additives and Contaminants, 24(12), 1367–1373. https://doi.org/10.1080/02652030701509964
- Martins, I. J. (2015). Overnutrition Determines LPS Regulation of Mycotoxin Induced Neurotoxicity in Neurodegenerative Diseases. International Journal of Molecular Sciences, 16(12), 29554–29573. https://doi.org/10.3390/ijms161226190
- Chang, C., Peng, Y., Hung, D.-Z., Hu, W., Yang, D.-Y., & Lin, T. (1999). Clinical impact of upper gastrointestinal tract injuries in glyphosate-surfactant oral intoxication. Human & Experimental Toxicology, 18(8), 475–478. https://doi.org/10.1191/096032799678847078
- Fathi, M., Han, G., Kang, R., Shen, D., Shen, J., & Li, C. (2020). Disruption of cytochrome P450 enzymes in the liver and small intestine in chicken embryos in ovo exposed to glyphosate. Environmental Science and Pollution Research, 27(14), 16865–16875. https://doi.org/10.1007/s11356-020-08269-3
- Amerio, P., Motta, A., Toto, P., Pour, S. M., Pajand, R., Feliciani, C., & Tulli, A. (2004). Skin Toxicity from Glyphosate‐Surfactant Formulation. Journal of Toxicology: Clinical Toxicology, 42(3), 317–319. https://doi.org/10.1081/clt-120038769
- Elias, P. M., Williams, M. L., Choi, E.-H., & Feingold, K. R. (2014). Role of cholesterol sulfate in epidermal structure and function: Lessons from X-linked ichthyosis. Biochimica et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids, 1841(3), 353–361. https://doi.org/10.1016/j.bbalip.2013.11.009
- Seneff, S., & Samsel, A. (2015). Glyphosate, pathways to modern diseases III: Manganese, neurological diseases, and associated pathologies. Surgical Neurology International, 6(1), 45. https://doi.org/10.4103/2152-7806.153876
- Elliott, Z. (2019). Do Pesticides cause Obesity and Diabetes? Thescholarship.ecu.edu. https://thescholarship.ecu.edu/handle/10342/8553
- Ren, X.-M., Kuo, Y., & Blumberg, B. (2020). Agrochemicals and obesity. Molecular and Cellular Endocrinology, 515, 110926. https://doi.org/10.1016/j.mce.2020.110926
- Grün, F., & Blumberg, B. (2007). Perturbed nuclear receptor signaling by environmental obesogens as emerging factors in the obesity crisis. Reviews in Endocrine and Metabolic Disorders, 8(2), 161–171. https://doi.org/10.1007/s11154-007-9049-x
- Zhang, W., Gao, Y., Chen, C., Li, A., Ma, X., Liang, Y., Yao, X., Song, M., & Jiang, G. (2021). Bisphenol S Promotes the Formation of Visceral Fat in Mice. Environmental Science and Technology Letters, 8(8), 699–704. https://doi.org/10.1021/acs.estlett.1c00419
- Deichmann, R., Lavie, C., & Andrews, S. (2010). Coenzyme q10 and statin-induced mitochondrial dysfunction. The Ochsner Journal, 10(1), 16–21. https://pubmed.ncbi.nlm.nih.gov/21603349/
- Molyneux, S. L., Florkowski, C. M., George, P. M., Pilbrow, A. P., Frampton, C. M., Lever, M., & Richards, A. M. (2008). Coenzyme Q10: An Independent Predictor of Mortality in Chronic Heart Failure. Journal of the American College of Cardiology, 52(18), 1435–1441. https://doi.org/10.1016/j.jacc.2008.07.044
- Seneff, S., Davidson, R. M., Lauritzen, A., Samsel, A., & Wainwright, G. (2015). A novel hypothesis for atherosclerosis as a cholesterol sulfate deficiency syndrome. Theoretical Biology and Medical Modelling, 12(1). https://doi.org/10.1186/s12976-015-0006-1
- Grigg, J. (2004). Environmental toxins; their impact on children’s health. Archives of Disease in Childhood, 89(3), 244–250. https://doi.org/10.1136/adc.2002.022202
- Li, H., Kilgallen, A. B., Münzel, T., Wolf, E., Lecour, S., Schulz, R., Daiber, A., & Van Laake, L. W. (2020). Influence of mental stress and environmental toxins on circadian clocks: Implications for redox regulation of the heart and cardioprotection. British Journal of Pharmacology, 177(23). https://doi.org/10.1111/bph.14949
- Stone, N. J., Robinson, J. G., Lichtenstein, A. H., Bairey Merz, C. N., Blum, C. B., Eckel, R. H., Goldberg, A. C., Gordon, D., Levy, D., Lloyd-Jones, D. M., McBride, P., Schwartz, J. S., Shero, S. T., Smith, S. C., Watson, K., & Wilson, P. W. F. (2013). 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. Circulation, 129(25 suppl 2), S1–S45. https://doi.org/10.1161/01.cir.0000437738.63853.7a
- 2018 Prevention Guidelines Tool CV Risk Calculator. (2018). Static.heart.org; American Heart Association. https://static.heart.org/riskcalc/app/index.html#
- Andersson, C., Enserro, D., Larson, M. G., Xanthakis, V., & Vasan, R. S. (2015). Implications of the US Cholesterol Guidelines on Eligibility for Statin Therapy in the Community: Comparison of Observed and Predicted Risks in the Framingham Heart Study Offspring Cohort. Journal of the American Heart Association, 4(4). https://doi.org/10.1161/jaha.115.001888
- Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents FULL REPORT. (2012). National Institutes of Health. U.S. Department of Health and Human Services. https://www.nhlbi.nih.gov/files/docs/guidelines/peds_guidelines_full.pdf
- Grimes, D. S., Hindle, E., & Dyer, T. (1996). Sunlight, cholesterol and coronary heart disease. QJM, 89(8), 579–590. https://doi.org/10.1093/qjmed/89.8.579
- Wood, A. P., Secombes, K. R., Thies, F., Aucott, L., Black, A. L., Mavroeidi, A., Simpson, W. R., Fraser, W. D., Reid, D. M., & Macdonald, H. M. (2012). Vitamin D3Supplementation Has No Effect on Conventional Cardiovascular Risk Factors: A Parallel-Group, Double-Blind, Placebo-Controlled RCT. QJM: An International Journal of Medicine, 97(10), 3557–3568. https://doi.org/10.1210/jc.2012-2126
- Gooding, H. C., Rodday, A. M., Wong, J. B., Gillman, M. W., Lloyd-Jones, D. M., Leslie, L. K., & de Ferranti, S. D. (2015). Application of Pediatric and Adult Guidelines for Treatment of Lipid Levels Among US Adolescents Transitioning to Young Adulthood. JAMA Pediatrics, 169(6), 569. https://doi.org/10.1001/jamapediatrics.2015.0168
- Preidt, R. (2015, April 6). New Guidelines Would Greatly Boost Number of Young People on Statins - Consumer Health News | HealthDay. Consumer.healthday.com. https://consumer.healthday.com/cardiovascular-health-information-20/heart-stroke-related-stroke-353/new-guidelines-would-greatly-boost-number-of-young-people-on-statins-698074.html?lexp=true&utm_expid=38353063-4.pIV1hUrQR8K_MJ1_OqjLag.1
- Kannel, W. B. (1961). Factors of Risk in the Development of Coronary Heart Disease—Six-Year Follow-up Experience. Annals of Internal Medicine, 55(1), 33. https://doi.org/10.7326/0003-4819-55-1-33
- Seppo Ylä-Herttuala. (1999). Oxidized LDL and Atherogenesisa. Annals of the New York Academy of Sciences, 874, 134–137. https://doi.org/10.1111/j.1749-6632.1999.tb09231.x
- Steinberg, D. (1997). Low Density Lipoprotein Oxidation and Its Pathobiological Significance. Journal of Biological Chemistry, 272(34), 20963–20966. https://doi.org/10.1074/jbc.272.34.20963
- Guasti, L., Galliazzo, S., Molaro, M., Visconti, E., Pennella, B., Gaudio, G. V., Lupi, A., Grandi, A. M., & Squizzato, A. (2020). TMAO as a biomarker of cardiovascular events: a systematic review and meta-analysis. Internal and Emergency Medicine, 16(1), 201–207. https://doi.org/10.1007/s11739-020-02470-5
- Panyod, S., Wu, W.-K., Chen, P.-C., Chong, K.-V., Yang, Y.-T., Chuang, H.-L., Chen, C.-C., Chen, R.-A., Liu, P.-Y., Chung, C.-H., Huang, H.-S., Lin, A. Y.-C., Shen, T.-C. D., Yang, K.-C., Huang, T.-F., Hsu, C.-C., Ho, C.-T., Kao, H.-L., Orekhov, A. N., & Wu, M.-S. (2022). Atherosclerosis amelioration by allicin in raw garlic through gut microbiota and trimethylamine-N-oxide modulation. Npj Biofilms and Microbiomes, 8(1). https://doi.org/10.1038/s41522-022-00266-3
- Lemaitre, R. N., King, I. B., Mozaffarian, D., Sotoodehnia, N., Rea, T. D., Kuller, L. H., Tracy, R. P., & Siscovick, D. S. (2006). Plasma Phospholipid Trans Fatty Acids, Fatal Ischemic Heart Disease, and Sudden Cardiac Death in Older Adults. Circulation, 114(3), 209–215. https://doi.org/10.1161/circulationaha.106.620336
- Zhang, D., Shen, X., & Qi, X. (2015). Resting heart rate and all-cause and cardiovascular mortality in the general population: a meta-analysis. Canadian Medical Association Journal, 188(3), E53–E63. https://doi.org/10.1503/cmaj.150535
- Natarajan, A., Pantelopoulos, A., Emir-Farinas, H., & Natarajan, P. (2020). Heart rate variability with photoplethysmography in 8 million individuals: a cross-sectional study. The Lancet Digital Health, 2(12). https://doi.org/10.1016/s2589-7500(20)30246-6
- Lecerf, J.-M., & de Lorgeril, M. (2011). Dietary cholesterol: from physiology to cardiovascular risk. The British Journal of Nutrition, 106(1), 6–14. https://doi.org/10.1017/S0007114511000237
- Chowdhury, R., Warnakula, S., Kunutsor, S., Crowe, F., Ward, H. A., Johnson, L., Franco, O. H., Butterworth, A. S., Forouhi, N. G., Thompson, S. G., Khaw, K.-T., Mozaffarian, D., Danesh, J., & Di Angelantonio, E. (2014). Association of dietary, circulating, and supplement fatty acids with coronary risk: a systematic review and meta-analysis. Annals of Internal Medicine, 160(6), 398–406. https://doi.org/10.7326/M13-1788
- Siri-Tarino, P. W., Sun, Q., Hu, F. B., & Krauss, R. M. (2010). Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease. The American Journal of Clinical Nutrition, 91(3), 535–546. https://doi.org/10.3945/ajcn.2009.27725
- Kang, Z.-Q., Yang, Y., & Xiao, B. (2019). Dietary saturated fat intake and risk of stroke: systematic review and dose-response meta-analysis of prospective cohort studies. Nutrition, Metabolism and Cardiovascular Diseases, 30(2). https://doi.org/10.1016/j.numecd.2019.09.028
- Doubling Saturated Fat in the Diet Does Not Increase Saturated Fat in Blood. (2014, November 18). Www.newswise.com; Ohio State University. https://www.newswise.com/articles/study-doubling-saturated-fat-in-the-diet-does-not-increase-saturated-fat-in-blood2?sc=dwhn
- DiNicolantonio, J. J. (2014). The cardiometabolic consequences of replacing saturated fats with carbohydrates or Ω-6 polyunsaturated fats: Do the dietary guidelines have it wrong? Open Heart, 1(1), e000032. https://doi.org/10.1136/openhrt-2013-000032
- Virkkunen, M. (1983). Serum Cholesterol Levels in Homicidal Offenders. Neuropsychobiology, 10(2-3), 65–69. https://doi.org/10.1159/000117987
- Hawton, K., Cowen, P., Owens, D., Bond, A., & Elliott, M. (1993). Low Serum Cholesterol and Suicide. British Journal of Psychiatry, 162(6), 818–825. https://doi.org/10.1192/bjp.162.6.818
- Law, M. R., Thompson, S. G., & Wald, N. J. (1994). Assessing possible hazards of reducing serum cholesterol. BMJ, 308(6925), 373–379. https://doi.org/10.1136/bmj.308.6925.373
- Knekt, P., Reunanen, A., Aromaa, A., Heliövaara, M., Hakulinen, T., & Hakama, M. (1988). Serum cholesterol and risk of cancer in a cohort of 39,000 men and women. Journal of Clinical Epidemiology, 41(6), 519–530. https://doi.org/10.1016/0895-4356(88)90056-x
- Strasak, A., Pfeiffer, R. M., Brant, L. J., Rapp, K., Wolfgang Hilbe, Willi Oberaigner, Lang, S., Wegene Borena, Concin, H., Diem, G., Ruttmann, E., Bernhard Glodny, Pfeiffer, K. P., & Ulmer, H. (2009). Time-dependent association of total serum cholesterol and cancer incidence in a cohort of 172 210 men and women: a prospective 19-year follow-up study. Annals of Oncology, 20(6), 1113–1120. https://doi.org/10.1093/annonc/mdn736
- Trieu, V. N., & Uckun, F. M. (1999). Low Density Lipoprotein (LDL)-Mediated Suppression of Lewis Lung Carcinoma in Hypercholesterolemic LDL Receptor-Deficient Mice. Biochemical and Biophysical Research Communications, 255(2), 377–381. https://doi.org/10.1006/bbrc.1999.0184
- Heiniger, H. J., Brunner, K. T., & Jean‐Charles Cerottini. (1978). Cholesterol is a critical cellular component for T-lymphocyte cytotoxicity. Proceedings of the National Academy of Sciences of the United States of America, 75(11), 5683–5687. https://doi.org/10.1073/pnas.75.11.5683
- Shu, Y., & Liu, H. (2007). Reversal of P-glycoprotein-mediated multidrug resistance by cholesterol derived from low density lipoprotein in a vinblastine-resistant human lymphoblastic leukemia cell line. Biochemistry and Cell Biology, 85(5), 638–646. https://doi.org/10.1139/o07-065
- Pérez-Guzmán, C., Vargas, M. H., Quiñonez, F., Bazavilvazo, N., & Aguilar, A. (2005). A Cholesterol-Rich Diet Accelerates Bacteriologic Sterilization in Pulmonary Tuberculosis. Chest, 127(2), 643–651. https://doi.org/10.1378/chest.127.2.643
- Noël, B. (2007). Lupus erythematosus and other autoimmune diseases related to statin therapy: a systematic review. Journal of the European Academy of Dermatology and Venereology, 21(1), 17–24. https://doi.org/10.1111/j.1468-3083.2006.01838.x
- Mammen, A. L. (2011). Autoimmune myopathies: autoantibodies, phenotypes and pathogenesis. Nature Reviews Neurology, 7(6), 343–354. https://doi.org/10.1038/nrneurol.2011.63
- Gajski, G., Garaj-Vrhovac, V., & Oreščanin, V. (2008). Cytogenetic status and oxidative DNA-damage induced by atorvastatin in human peripheral blood lymphocytes: Standard and Fpg-modified comet assay. Toxicology and Applied Pharmacology, 231(1), 85–93. https://doi.org/10.1016/j.taap.2008.03.013
- Singh-Manoux, Archana, et al. “Low HDL Cholesterol Is a Risk Factor for Deficit and Decline in Memory in Midlife.” Arteriosclerosis, Thrombosis, and Vascular Biology, vol. 28, no. 8, Aug. 2008, pp. 1556–1562, https://doi.org/10.1161/atvbaha.108.163998.
- Huang, Xuemei, et al. “Serum Cholesterol and the Progression of Parkinson’s Disease: Results from DATATOP.” PLoS ONE, vol. 6, no. 8, 11 Aug. 2011, p. e22854, https://doi.org/10.1371/journal.pone.0022854.
- “FDA Drug Safety Communication: Important Safety Label Changes to Cholesterol-Lowering Statin Drugs.” FDA, 19 Jan. 2016, www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-important-safety-label-changes-cholesterol-lowering-statin-drugs.
- “Statin Drugs & Neurotoxic Focused Research | GreenMedInfo.com.” GreenMedInfo, 2016, greenmedinfo.com/greenmed/topic/52438/focus/35335/page. Accessed 24 Oct. 2023.
- “Statin Drugs & Memory Disorders Focused Research | GreenMedInfo.com.” GreenMedInfo, 2016, greenmedinfo.com/greenmed/topic/52438/focus/3223/page. Accessed 24 Oct. 2023.
- Shiels, Paul G., et al. “Accelerated Telomere Attrition Is Associated with Relative Household Income, Diet and Inflammation in the PSoBid Cohort.” PLoS ONE, vol. 6, no. 7, 27 July 2011, p. e22521, https://doi.org/10.1371/journal.pone.0022521.
- Felman, Adam. “Inflammation: Causes, Symptoms, and Treatment.” Www.medicalnewstoday.com, 13 Apr. 2020, www.medicalnewstoday.com/articles/248423.
- Ishaka, Aminu, et al. “Glyphosate Suppresses the Ability of PON1 to Hydrolyse Oxidized-LDL in the Exposed Farm Workers in Pahang, Malaysia.” IIUM Medical Journal Malaysia, vol. 22, no. 3, 1 July 2023, https://doi.org/10.31436/imjm.v22i3.2303.
- Pfützner, Andreas, and Thomas Forst. “High-Sensitivity C-Reactive Protein as Cardiovascular Risk Marker in Patients with Diabetes Mellitus.” Diabetes Technology & Therapeutics, vol. 8, no. 1, Feb. 2006, pp. 28–36, https://doi.org/10.1089/dia.2006.8.28.
- Dunkin, Mary Anne. “What You Should Know: Myocarditis.” WebMD, WebMD, 20 Oct. 2009, www.webmd.com/heart-disease/myocarditis.
- Fallon, Sally, and Enig, Mary G. “Dangers of Statin Drugs: What You Haven’t Been Told about Popular Cholesterol-Lowering Medicines.” The Weston A. Price Foundation, 14 June 2004, www.westonaprice.org/health-topics/modern-diseases/dangers-of-statin-drugs-what-you-havent-been-told-about-popular-cholesterol-lowering-medicines.
²⁴ ²⁵ ²⁶ ²⁷ ²⁸ ²⁹ ³⁰
³¹ ³² ³³ ³⁴ ³⁵ ³⁶ ³⁷ ³⁸ ³⁹ ⁴⁰
⁴¹ ⁴² ⁴³ ⁴⁴ ⁴⁵ ⁴⁶ ⁴⁷ ⁴⁸ ⁴⁹ ⁵⁰
⁵¹ ⁵² ⁵³ ⁵⁴ ⁵⁵ ⁵⁶ ⁵⁷ ⁵⁸ ⁵⁹ ⁶⁰
⁶¹ ⁶² ⁶³ ⁶⁴ ⁶⁵ ⁶⁶ ⁶⁷ ⁶⁸ ⁶⁹ ⁷⁰
⁷¹ ⁷² ⁷³ ⁷⁴ ⁷⁵ ⁷⁶ ⁷⁷ ⁷⁸ ⁷⁹ ⁸⁰
⁸¹ ⁸² ⁸³ ⁸⁴ ⁸⁵ ⁸⁶ ⁸⁷ ⁸⁸ ⁸⁹ ⁹⁰
⁹¹ ⁹² ⁹³ ⁹⁴ ⁹⁵ ⁹⁶ ⁹⁷ ⁹⁸ ⁹⁹ ¹⁰⁰
³¹ ³² ³³ ³⁴ ³⁵ ³⁶ ³⁷ ³⁸ ³⁹ ⁴⁰
⁴¹ ⁴² ⁴³ ⁴⁴ ⁴⁵ ⁴⁶ ⁴⁷ ⁴⁸ ⁴⁹ ⁵⁰
⁵¹ ⁵² ⁵³ ⁵⁴ ⁵⁵ ⁵⁶ ⁵⁷ ⁵⁸ ⁵⁹ ⁶⁰
⁶¹ ⁶² ⁶³ ⁶⁴ ⁶⁵ ⁶⁶ ⁶⁷ ⁶⁸ ⁶⁹ ⁷⁰
⁷¹ ⁷² ⁷³ ⁷⁴ ⁷⁵ ⁷⁶ ⁷⁷ ⁷⁸ ⁷⁹ ⁸⁰
⁸¹ ⁸² ⁸³ ⁸⁴ ⁸⁵ ⁸⁶ ⁸⁷ ⁸⁸ ⁸⁹ ⁹⁰
⁹¹ ⁹² ⁹³ ⁹⁴ ⁹⁵ ⁹⁶ ⁹⁷ ⁹⁸ ⁹⁹ ¹⁰⁰