|
Prescription drugs have become a significant public health concern, with overtreatment and misuse leading to an alarming number of deaths. The increasing death rate from these drugs is particularly concerning given that many of these fatalities are preventable. The Scale of the ProblemIn 2013, it was estimated that prescription drugs were the third leading cause of death in the United States, following heart disease and cancer. By 2015, it was noted that psychiatric drugs alone also ranked as the third leading cause of death. However, some estimates place prescription drugs as the fourth leading cause, based on a 1998 meta-analysis that primarily considered in-hospital adverse drug reactions. This analysis likely underestimates the true extent of the problem since most drug-related deaths occur outside of hospitals and involve complications that are not always correctly attributed to drug use. Underreported and Misclassified DeathsMany deaths linked to prescription drugs are misclassified as natural or unknown causes. This issue is particularly prevalent with psychiatric drugs, where sudden deaths in young patients are often labeled as natural despite known risks of fatal heart arrhythmias from neuroleptics. Similarly, deaths from depression drugs in the elderly, caused by falls and fractures, often go unrecognized as drug-related. Specific Drug Categories and Risks
Increasing PolypharmacyPolypharmacy, the use of multiple medications by a single patient, has been on the rise, especially among the elderly. This trend increases the risk of adverse drug interactions and fatalities. For example, combining benzodiazepines with neuroleptics significantly raises mortality rates. Estimates of Annual Drug-Related DeathsCurrent estimates suggest that over 882,000 deaths in the United States annually can be attributed to prescription drugs. This figure includes hospital deaths, psychiatric drug fatalities, opioid overdoses, and deaths from NSAIDs. These numbers highlight the magnitude of the problem and the urgent need for intervention. The Role of Misguided Regulation and Lack of AwarenessThe pharmaceutical industry's influence on drug regulation has led to more permissive policies, exacerbating the issue. Many deaths could be prevented if drugs were prescribed more judiciously. For instance, neuroleptics and antidepressants often show minimal efficacy in trials, yet they are widely prescribed. Similarly, NSAIDs are commonly recommended despite their significant risks, often without sufficient consideration of safer alternatives. The pervasive issue of prescription drug-related deaths necessitates a reevaluation of current medical practices and regulatory policies. With most of these deaths being preventable, a more cautious approach to prescribing and better awareness of the risks associated with these medications could save countless lives. It is crucial for healthcare providers, regulators, and patients to acknowledge the dangers and work towards safer, more effective treatment strategies. In bed with big pharma: A $12 Billion RelationshipA comprehensive analysis by Yale University researchers has revealed that nearly six in ten doctors in the United States have received over $12 billion in payments from pharmaceutical and medical device companies over the past decade. This study sheds light on the pervasive financial relationships between healthcare providers and the medical industry, highlighting potential conflicts of interest. Key Findings from the Study
Largest Recipients by SpecialtyOrthopedic surgeons topped the list, receiving the highest total sum of payments at $1.36 billion. They were followed by:
most profitable Drugs and Devices
most prescribed drugsEvery day, millions of people in the U.S. take prescribed drugs in an effort to help them live their lives. As our understanding of medicine has evolved, we’ve developed drugs to aid with some of the most common medical conditions—from pain and blood pressure drugs to asthma medication, thyroid treatments, and antidepressants. This analysis uses prescribed medicines data from the U.S. Agency for Healthcare Research and Quality, released in 2021 for the 2019 calendar year. It also uses supporting drug and health information from MedlinePlus. Top 10 Most Prescribed Drugs in America (2019)
The most prescribed drug, atorvastatin (sold under the brand name Lipitor), was prescribed to 24.5 million people in the U.S. in 2019, or 7.5% of the population. It was one of many statin medications listed, which are claimed to prevent cardiovascular disease and treat abnormal lipid levels. Prevalent Conditions Treated Most of the top prescribed drugs are used to treat high blood pressure or symptoms of it. This is significant as 108 million, or nearly half of adults in the U.S., have hypertension or high blood pressure.
Combining the total patients for blood pressure and cholesterol medications covers 33% of the U.S. population. Pain and inflammation medications were the most frequent on the top 30 list, prescribed to 13.6% of people. Drug Spending in the U.S.A drug’s total number of patients doesn’t necessarily reflect its importance or cost. For example, levothyroxine, the fourth-most prescribed drug by total patients, was the second-most prescribed by total prescriptions with 102.6 million in 2019 at an average cost of $25.10 per prescription. More specialized medications like fluticasone had fewer total prescriptions (27.9 million) but a higher average cost of $97.68 per prescription. Prices are influenced by factors like demand, patent status, and healthcare system variations. Implications and ConcernsThe study underscores ongoing concerns about financial conflicts of interest in the medical field. Researchers noted that such payments might influence physician prescribing behavior and potentially undermine patient trust in medical professionals. Despite these concerns, the practice of accepting industry payments remains widespread. Data Source and MethodologyThe study utilized data from the Open Payments platform, a national database where drug and medical device companies are required to disclose payments made to physicians. This platform aims to increase transparency and help patients make informed decisions about their healthcare providers. FDA recalls and safety concernsIn a related safety concern, the FDA recalled certain Impella devices in December due to a perforation risk that could cause serious injuries or death. This highlights the ongoing need for vigilance regarding the safety of medical devices widely used in clinical practice. ConclusionThis comprehensive analysis by Yale University researchers provides a clear picture of the substantial financial ties between US doctors and the medical industry, emphasizing the need for ongoing scrutiny and transparency. The relationship between healthcare providers and the medical industry is complex and often financially intertwined. While these financial interactions can support medical education and innovation, they also pose significant ethical and practical challenges. Ensuring transparency and addressing potential conflicts of interest are crucial steps toward maintaining the integrity of medical practice and patient trust. referencesGøtzsche PC. Deadly Medicines and Organised Crime: How Big Pharma Has Corrupted Health Care. London: Radcliffe Publishing; 2013.
Gøtzsche PC. Deadly Psychiatry and Organised Denial. Copenhagen: People’s Press; 2015. Schroeder MO. Death by Prescription: By one estimate, taking prescribed medications is the fourth leading cause of death among Americans. US News 2016; Sept 27. Light DW, Lexchin J, Darrow JJ. Institutional corruption of pharmaceuticals and the myth of safe and effective drugs. J Law Med Ethics 2013;41:590-600. Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA 1998;279:1200–5. FAERS Reporting by Patient Outcomes by Year. FDA 2015;Nov 10. Gøtzsche PC. Mental Health Survival Kit and Withdrawal From Psychiatric Drugs. Ann Arbor: L H Press; 2022. Hubbard R, Farrington P, Smith C, et al. Exposure to tricyclic and selective serotonin reuptake inhibitor antidepressants and the risk of hip fracture. Am J Epidemiol 2003;158:77-84. Thapa PB, Gideon P, Cost TW, et al. Antidepressants and the risk of falls among nursing home residents. N Engl J Med 1998;339:875-82. Ebbesen J, Buajordet I, Erikssen J, et al. Drug-related deaths in a department of internal medicine. Arch Intern Med 2001;161:2317–23. James JTA. A new, evidence-based estimate of patient harms associated with hospital care. J Patient Saf 2013;9:122-8. Ho JY. Life Course Patterns of Prescription Drug Use in the United States. Demography 2023;60:1549-79. Gøtzsche PC. Long-term use of antipsychotics and antidepressants is not evidence-based. Int J Risk Saf Med 2020;31:37-42. Gøtzsche PC. Long-Term Use of Benzodiazepines, Stimulants and Lithium is Not Evidence-Based. Clin Neuropsychiatry 2020;17:281-3. Forbruget af antipsykotika blandt 18-64 årige patienter, med skizofreni, mani eller bipolar affektiv sindslidelse. København: Sundhedsstyrelsen; 2006. Hughes S, Cohen D, Jaggi R. Differences in reporting serious adverse events in industry sponsored clinical trial registries and journal articles on antidepressant and antipsychotic drugs: a cross-sectional study. BMJ Open 2014;4:e005535. Schneider LS, Dagerman KS, Insel P. Risk of death with atypical antipsychotic drug treatment for dementia: meta-analysis of randomized placebo-controlled trials. JAMA 2005;294:1934–43. FDA package insert for Risperdal (risperidone). Accessed 30 May 2022. Koponen M, Taipale H, Lavikainen P, et al. Risk of Mortality Associated with Antipsychotic Monotherapy and Polypharmacy Among Community-Dwelling Persons with Alzheimer’s Disease. J Alzheimers Dis 2017;56:107-18. Whitaker R. Lure of Riches Fuels Testing. Boston Globe 1998; Nov 17. Whitaker R. Mad in America: Bad science, Bad medicine, and the Enduring Mistreatment of the Mentally Ill. Cambridge: Perseus Books Group; 2002:page 269. Vanderburg DG, Batzar E, Fogel I, et al. A pooled analysis of suicidality in double-blind, placebo-controlled studies of sertraline in adults. J Clin Psychiatry 2009;70:674-83. Hengartner MP, Plöderl M. Newer-Generation Antidepressants and Suicide Risk in Randomized Controlled Trials: a Re-Analysis of the FDA Database. Psychother Psychosom 2019;88:247-8. Hengartner MP, Plöderl M. Reply to the Letter to the Editor: “Newer-Generation Antidepressants and Suicide Risk: Thoughts on Hengartner and Plöderl’s ReAnalysis.” Psychother Psychosom 2019;88:373-4. Weich S, Pearce HL, Croft P, et al. Effect of anxiolytic and hypnotic drug prescriptions on mortality hazards: retrospective cohort study. BMJ 2014;348:g1996. Kripke DF, Langer RD, Kline LE. Hypnotics’ association with mortality or cancer: a matched cohort study. BMJ Open 2012;2:e000850. Coupland C, Dhiman P, Morriss R, et al. Antidepressant use and risk of adverse outcomes in older people: population based cohort study. BMJ 2011;343:d4551. Smoller JW, Allison M, Cochrane BB, et al. Antidepressant use and risk of incident cardiovascular morbidity and mortality among postmenopausal women in the Women’s Health Initiative study. Arch Intern Med 2009;169:2128-39. O’Neill A. Age distribution in the United States from 2012 to 2022. Statista 2024;Jan 25. Olfson M, King M, Schoenbaum M. Antipsychotic Treatment of Adults in the United States. Psychiatrist.com 2015;Oct 21. Maust DT, Lin LA, Blow FC. Benzodiazepine Use and Misuse Among Adults in the United States. Psychiatr Serv 2019;70:97-106. Brody DJ, Gu Q. Antidepressant Use Among Adults: United States, 2015-2018. CDC 2020; Sept. Centers for Disease Control and Prevention. Leading Causes of Death. 2024; Jan 17. Drug Overdose Deaths. Centers for Disease Control and Prevention 2023; Aug 22. Davis JS, Lee HY, Kim J, et al. Use of non-steroidal anti-inflammatory drugs in US adults: changes over time and by demographic. Open Heart 2017;4:e000550. Conaghan PG. A turbulent decade for NSAIDs: update on current concepts of classification, epidemiology, comparative efficacy, and toxicity. Rheumatol Int 2012;32:1491-502. Bally M, Dendukuri N, Rich B, et al. Risk of acute myocardial infarction with NSAIDs in real world use: bayesian meta-analysis of individual patient data. BMJ 2017;357:j1909. Bresalier RS, Sandler RS, Quan H, et al. Cardiovascular Events Associated with Rofecoxib in a Colorectal Adenoma Chemoprevention Trial. N Engl J Med 2005;352:1092-102. Blower AL, Brooks A, Fenn GC, et al. Emergency admissions for upper gastrointestinal disease and their relation to NSAID use. Aliment Pharmacol Ther 1997;11:283–91. Davis C, Lexchin J, Jefferson T, Gøtzsche P, McKee M. “Adaptive pathways” to drug authorisation: adapting to industry? BMJ 2016;354:i4437. van der Hooft CS, Sturkenboom MC, van Grootheest K, et al. Adverse drug reaction-related hospitalisations: a nationwide study in The Netherlands. Drug Saf 2006;29:161-8. Gøtzsche PC. Big marketing hoax: Non-steroidal, anti-inflammatory drugs (NSAIDs) are not anti-inflammatory. Copenhagen: Institute for Scientific Freedom 2022;Nov 10. Perlis R. The time has come for over-the-counter antidepressants. Stat News 2024;April 8. Gøtzsche PC. Critical Psychiatry Textbook. Copenhagen: Institute for Scientific Freedom; 2022. Freely available. Tilley, Caitlin. “Corruption Fears as Report Finds US Doctors Received Record $12bn.” Mail Online, 3 Apr. 2024, www.dailymail.co.uk/health/article-13268371/Corruption-doctors-received-pharma-payments.html. Tanne, Janice Hopkins. “US Doctors Received More than $12bn in Industry Payments between 2013 and 2022, Study Shows.” BMJ, vol. 385, 2 Apr. 2024, p. q781, www.bmj.com/content/385/bmj.q781.full, https://doi.org/10.1136/bmj.q781.
0 Comments
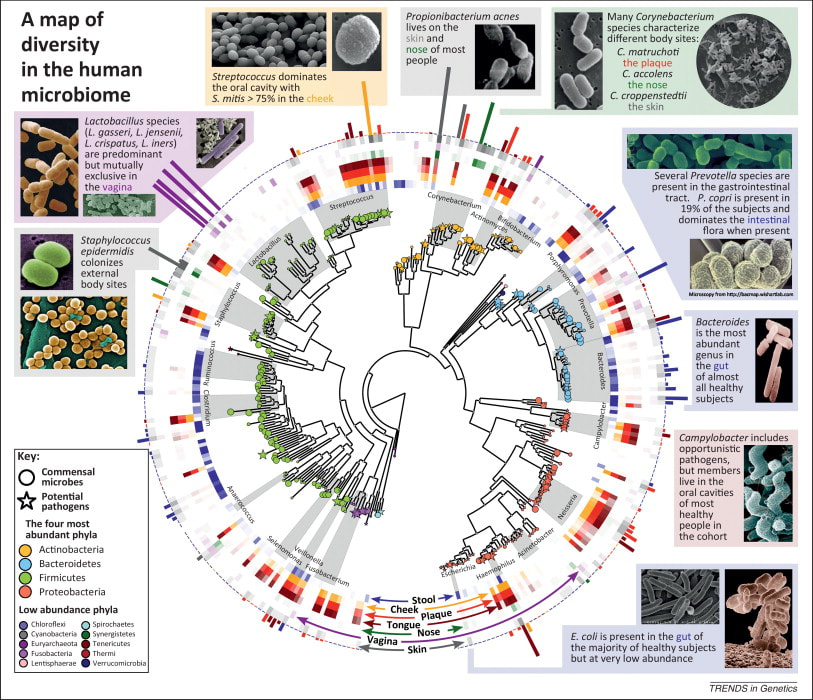
Recent breakthrough studies have shone a light on the intriguing link between our microbiome – the diverse community of microorganisms residing in our gut and mouth – and the secret to a longer, healthier life. Scientists have long suspected that our genes, environment, and internal factors like the microbiome play a role in determining how long we live, but the specifics remained elusive. Now, thanks to cutting-edge research, we're getting closer to unraveling the mysteries of longevity. In this groundbreaking exploration, scientists employed a sophisticated approach called Mendelian randomization (MR) to delve into the intricate relationships between the human microbiome and longevity. By analyzing genetic data from large cohorts, they uncovered some compelling associations that shed light on the microbial players in the quest for a longer life. The Gut Chronicles: Microbial Superstars and CulpritsThe gut microbiome, a bustling metropolis of bacteria, has been a focal point in the quest for longevity. The study identified certain gut microbes as potential champions in the battle against aging. Microbial heroes like Coriobacteriaceae, Oxalobacter, and the probiotic Lactobacillus amylovorus were found to be positively linked to increased odds of longevity. On the flip side, a few gut microbes emerged as potential antagonists, with names like Fusobacterium nucleatum, Coprococcus, Streptococcus, Lactobacillus, and Neisseria negatively associated with longevity. These microbial foes might have a role in determining how gracefully we age. Oral Health: More Than Just a Pretty SmileThe study didn't stop at the gut; it extended its gaze to the oral microbiome, a less-explored but equally important realm. The findings suggested a fascinating connection between the oral microbiome and longevity. Specific oral bacteria were identified as potential influencers in the longevity game. Interestingly, the research hinted at a lower gut microbial diversity among centenarians (diversity appears to lower with age), but no significant difference in their oral microbiota. This finding underscores the importance of tracking the movements of these beneficial microbes across different parts of the body for a longer and healthier life. Decoding the Genetic Blueprint for LongevityThe study leveraged Mendelian randomization to unravel the causality between the microbiome and longevity. This approach, using genetic variants as tools, allowed scientists to explore the potential causal links between specific microbial features and the length of our lives. The bidirectional analyses provided a wealth of information, not only pinpointing specific microbes associated with longevity but also revealing the microbial preferences of genetically longevous individuals. For instance, genetic predisposition to longevity correlated with a higher abundance of Prevotella and a lower abundance of Bacteroides, suggesting a potential link between dietary choices and a longer life. Microbes and Diseases: Unraveling the We The study didn't just stop at longevity; it ventured into the realm of diseases. Certain microbes associated with longevity were found to have correlations with specific diseases. For example, Coriobacteriaceae, linked to longevity, was significantly reduced in patients with heart failure, suggesting a potential protective role against cardiovascular diseases. This "microbiota—disease—longevity" axis provides a nuanced understanding of how our microbial companions might influence not only our lifespan but also our susceptibility to various health conditions. What's Next in the Quest for a Longer LifeWhile the study opens exciting new avenues, there are some limitations to consider. The identified causalities didn't all reach statistical significance due to the vast number of microbial features tested. However, the robustness of the findings was supported by the replication of several identified causal links in independent datasets. Moving forward, researchers aim to collect more comprehensive individual-level data, including microbiome profiles, genetics, socio-economic factors, behaviors, and environmental influences. This holistic approach will help tease apart the individual contributions of these factors to longevity. In conclusion, this pioneering study, using Mendelian randomization, has provided us with a roadmap to explore the intricate connections between our microbiome and the quest for a longer, healthier life. As we unlock the secrets hidden in our genes and microbes, we inch closer to personalized approaches for healthy aging and interventions that could extend our time on this planet. referencesLiu, Xiaomin, et al. “Mendelian Randomization Analyses Reveal Causal Relationships between the Human Microbiome and Longevity.” Scientific Reports, vol. 13, no. 1, 29 Mar. 2023, p. 5127, www.nature.com/articles/s41598-023-31115-8, https://doi.org/10.1038/s41598-023-31115-8.
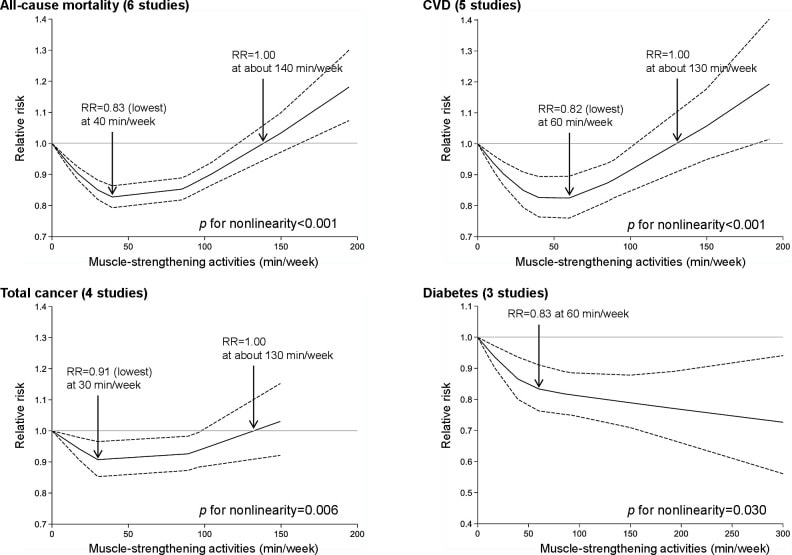
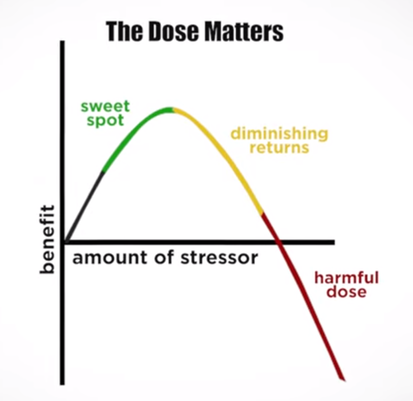
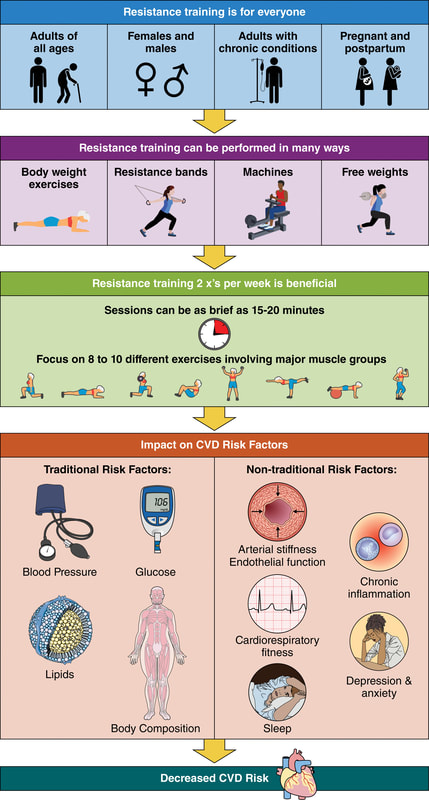
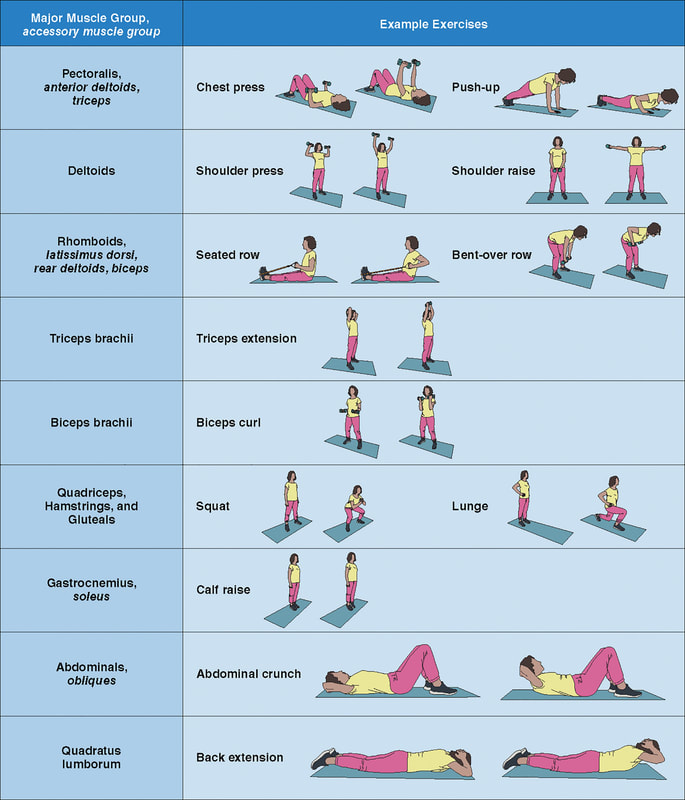
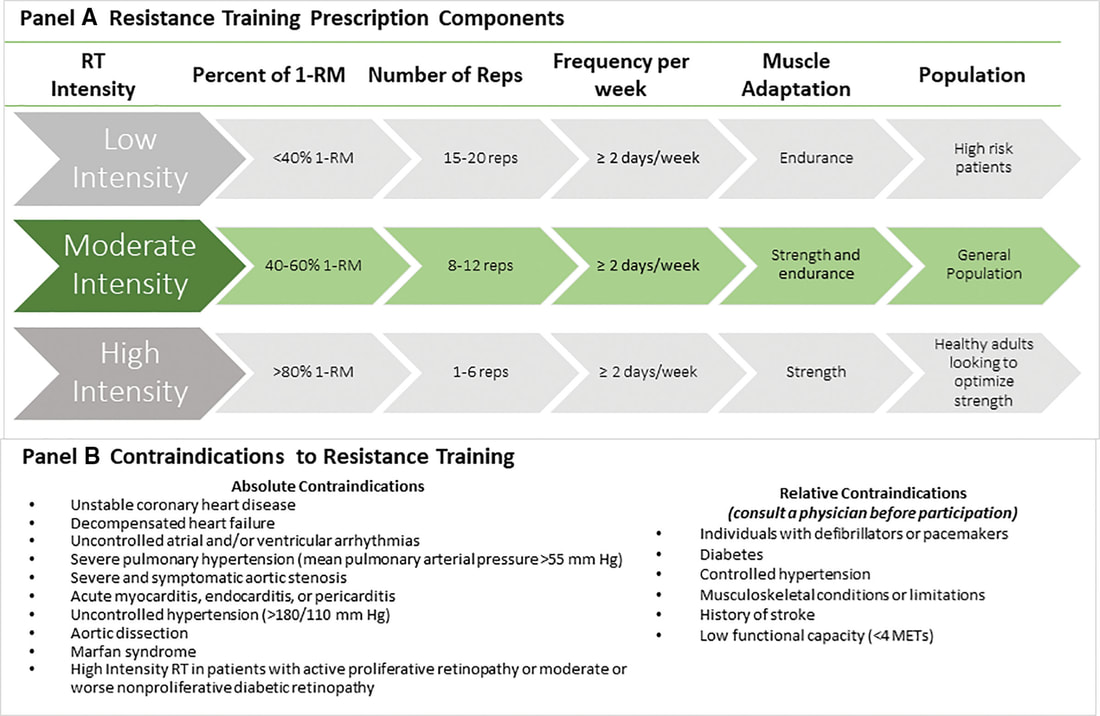
In an update to its 2007 scientific statement, the American Heart Association (AHA) emphasizes the significant and multifaceted benefits of resistance training (RT) on cardiovascular health. Contrary to the misconception that RT solely enhances muscle mass and strength, the statement highlights the favorable physiological and clinical effects of this form of exercise on cardiovascular disease (CVD) and associated risk factors. The scientific statement aims to provide comprehensive insights into the impact of RT, either alone or in combination with aerobic training, on traditional and nontraditional CVD risk factors. More is not always betterEpidemiological evidence suggests that RT is associated with a lower risk of all-cause mortality and CVD morbidity and mortality. Adults who participate in RT have ≈15% lower risk of all-cause mortality and 17% lower risk of CVD, compared with adults who report no RT. Approximately 30 to 60 minutes per week of RT is associated with the maximum risk reduction for all-cause mortality and incident CVD. Notice this "U" shape in the curve when examining the relationship between RT and morbidity and mortality. This curve suggests that some RT is clearly beneficial, but has the volume of RT increases past a certain point the benefits drop and it becomes harmful. The concept of a "biphasic response" is fundamental to understanding hormesis. It describes the characteristic dose-response relationship observed in hormetic processes, where a substance or stressor elicits opposite effects at low and high doses. The response can be visualized as a U-shaped or J-shaped curve, illustrating the beneficial effects at low doses and potential harm at higher doses. Benefits of RT on Traditional CVD Risk FactorsThe AHA's scientific statement underscores the positive influence of RT on traditional CVD risk factors, including blood pressure (BP), glycemia, lipid profiles, and body composition. Numerous studies indicate that engaging in RT is associated with reduced resting BP, improved glycemic control, and favorable alterations in lipid profiles, contributing to a lower risk of all-cause mortality and CVD morbidity. Despite recommendations suggesting 2 days per week of RT, only 28% of U.S. adults adhere to this guideline, highlighting the need for increased awareness and promotion. RT and resting blood pressureRT has demonstrated the ability to reduce resting BP across diverse populations, with notable benefits observed in individuals with prehypertension and hypertension. The mechanisms behind these benefits include enhancements in endothelial function, vasodilatory capacity, and vascular conductance. The reductions in BP achieved through RT are comparable to those achieved with antihypertensive medications. RT and GlycemiaRT shows promise in improving glycemia and insulin resistance, leading to a lower incidence of diabetes. The evidence suggests a nonlinear dose-response association, with up to 60 minutes per week of RT associated with the maximum risk reduction for diabetes. RT and Lipid ProfilesWhile the effect on lipid profiles is modest, RT results in favorable changes in high-density lipoprotein cholesterol, total cholesterol, and triglycerides. These improvements are more pronounced in older adults and those with elevated cardiometabolic risk. Rt, Body composition, and weightRT positively influences body composition by increasing lean body mass and reducing body fat percentage. It is particularly effective in overweight or obese individuals, contributing to increased metabolic rate and mitigating weight gain over time. Benefits of RT on Nontraditional CVD Risk FactorsIn addition to traditional risk factors, the scientific statement highlights the potential mechanisms by which RT positively affects nontraditional CVD risk factors. These include increased cardiorespiratory fitness, improved endothelial function, and potential benefits for sleep quality, psychological health, and well-being. The AHA's updated scientific statement reinforces the pivotal role of resistance training in cardiovascular health, providing a comprehensive overview of its impact on both traditional and nontraditional risk factors. As the evidence supporting RT's benefits continues to grow, the statement serves as a valuable resource for clinicians and public health professionals, offering practical strategies for promoting and prescribing resistance training to enhance cardiovascular health in diverse populations. ReferencesPaluch, Amanda E, et al. “Resistance Exercise Training in Individuals with and without Cardiovascular Disease: 2023 Update: A Scientific Statement from the American Heart Association.” Circulation, 7 Dec. 2023, https://doi.org/10.1161/cir.0000000000001189. Accessed 11 Dec. 2023.
Momma H, Kawakami R, Honda T, Sawada SS. Muscle-strengthening activities are associated with lower risk and mortality in major non-communicable diseases: a systematic review and meta-analysis of cohort studies. Br J Sports Med. 2022 Jul;56(13):755-763. doi: 10.1136/bjsports-2021-105061. Epub 2022 Feb 28. PMID: 35228201; PMCID: PMC9209691.
Of those 34 eligible studies, 24 qualified for inclusion in the meta-analysis. They were separated into three groups: lockdown stringency index studies, shelter-in-placeorder (SIPO) studies, and specific NPI studies. An analysis of each of these three groups support the conclusion that lockdowns have had little to no effect on COVID-19 mortality. More specifically, stringency index studies find that lockdowns in Europe and the United States only reduced COVID-19 mortality by 0.2% on average. SIPOs were also ineffective, only reducing COVID-19 mortality by 2.9% on average. Specific NPI studies also find no broad-based evidence of noticeable effects on COVID-19 mortality. While this meta-analysis concludes that lockdowns have had little to no public health effects, they have imposed enormous economic and social costs where they have been adopted. In consequence, lockdown policies are ill-founded and should be rejected as a pandemic policy instrument.
Over the course of the past century, the Western culture has faced numerous health epidemics, from obesity to opioids. Today we are facing an epidemic of a different nature. The epidemic of loneliness. We're more connected than ever, but are we feeling more alone? In the last 50 years, rates of loneliness have doubled in the United States. In a survey of over 20,000 American adults, it was found that almost half of respondents reported feeling alone, left out, and isolated. Further, one in four Americans shared that they rarely feel understood, and one in five people believe they rarely or never feel not close to people. Loneliness is on the rise for Americans regardless of geographic location, gender, race, or ethnicity. Human beings did not evolve to be alone. Sociality plays a fundamental part in the wellbeing of Homo sapiens. Conversely, social isolation and loneliness are known risk factors for premature death, more so than being obese (Holt-Lunstad et al., 2015). Individuals who feel socially isolated and alone also have higher rates of cardiovascular disease, alcoholism and suicidality, physical diseases related to stress and compromised immune function, and in later life, greater risk of degenerative dementia. Even worse, researchers have observed that geriatric individuals who are considered lonely have a 45% increased risk of mortality (Leland, 2012; Perissinotto, Stijacic Cenzer and Covinsky, 2012). Moreover, lonely individuals experience reductions in reasoning and creativity. In addition to these reduced abilities, loneliness affects workplace productivity, as lonely individuals report less job satisfaction and are more likely to face unemployment. Not surprisingly, loneliness is commonly correlated with mental health concerns such as anxiety and depression. Similarly, loneliness is often associated with poor coping mechanisms, such as compulsive technology use, smoking, and self-harm. In other words, loneliness has both physical and psychological implications, many of which could be long term. Alone versus Lonely Before determining yourself as lonely, there is a difference between being alone and feeling lonely. Being alone and feeling lonely are not mutually dependent. Loneliness is a subjective experience, a feeling of sadness stemming from isolation or abandonment. But, a person can be alone without feeling lonely, since alone describes a state of being and lonely describes an emotional response to one's circumstance. For example, most people don't feel sad when they go to the restroom by themselves. A person can be alone in the sense that no other people are present, or alone in the sense that they are unaccompanied, even in a crowd. When assessing loneliness, introverted and extroverted personalities should be taken into account, because some people enjoy the presence of being alone with themselves, whereas others are dependent on others to cope with not being by themselves. Being at either end of the spectrum, whether it is total isolation or complete dependence, is not considered a healthy behavioral pattern. Factors Influencing LonelinessThe predictors of loneliness is the basis for the identification of factors that cause and contribute to loneliness. The are three broad categories that influence the feeling of loneliness:
These categories may be subdivided into multiple factors that increase loneliness:
While it is impossible to avoid loneliness completely, it may be alleviated. It is recommended to investigate the contributory factors towards loneliness because knowledge of these may substantially lessen the impact of loneliness on people's mental health status. Such knowledge will contribute to an improved quality of life, productivity and health. Sleep Deprivation-Induced Loneliness The "loneliness phenotype" can be triggered by sleep deprivation. Researchers have observed that a lack of sleep induces critical changes within the brain, altering behavior and emotions, while also disturbing essential metabolic processes and influencing the expression of immune-related genes. The end result is that people who are sleep-deprived avoid social interaction. This asocial profile is recognizable by other people, who, in turn, shun the sleep-deprived people in a psychosocial loop that perpetuates in a vicious cycle of loneliness and other mental health disorders. Some Solutions to Loneliness REferences Ali, S. (2018). What You Need to Know About the Loneliness Epidemic. [online] Psychology Today. Available at: https://www.psychologytoday.com/us/blog/modern-mentality/201807/what-you-need-know-about-the-loneliness-epidemic [Accessed 1 Sep. 2019].
Harris, R. (2015). Are we lonelier than ever?. [online] The Independent. Available at: https://www.independent.co.uk/life-style/health-and-families/features/the-loneliness-epidemic-more-connected-than-ever-but-feeling-more-alone-10143206.html [Accessed 1 Sep. 2019]. Holt-Lunstad, J., Smith, T., Baker, M., Harris, T. and Stephenson, D. (2015). Loneliness and Social Isolation as Risk Factors for Mortality. Perspectives on Psychological Science, 10(2), pp.227-237. https://doi.org/10.1177/1745691614568352 Leland, K. (2012). Loneliness Linked to Serious Health Problems and Death Among Elderly. [online] UC San Francisco. Available at: https://www.ucsf.edu/news/2012/06/98644/loneliness-linked-serious-health-problems-and-death-among-elderly [Accessed 1 Sep. 2019]. Perissinotto, C., Stijacic Cenzer, I. and Covinsky, K. (2012). Loneliness in Older Persons. Archives of Internal Medicine, 172(14). https://doi.org/10.1001/archinternmed.2012.1993 Ben Simon, E. and Walker, M. (2018). Sleep loss causes social withdrawal and loneliness. Nature Communications, 9(1). https://doi.org/10.1038/s41467-018-05377-0
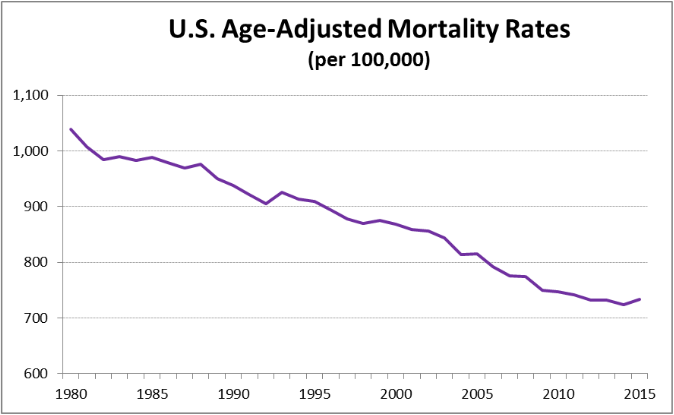
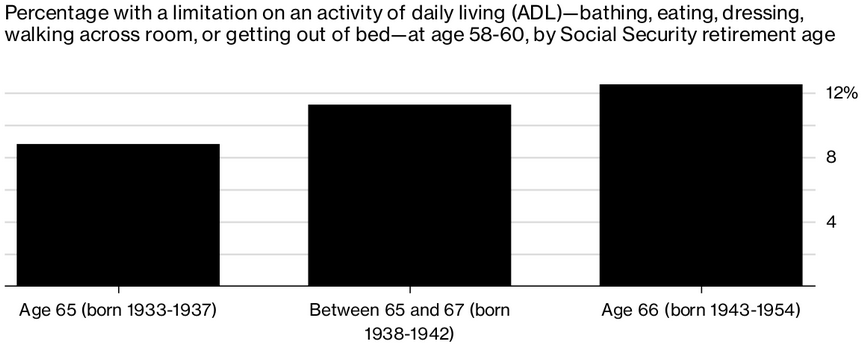
At the same time that Americans’ life expectancy is stalling, the age at which people can claim their full Social Security benefits is gradually moving up, from 65 for those retiring in 2002 to 67 in 2027. Almost one in three Americans age 65 to 69 is still working, along with almost one in five in their early 70s. Meanwhile, Americans in their late 50s already have more serious health problems than people at the same ages did 10 to 15 years ago, (Choi & Schoeni, 2017). Researchers analyzed survey data to compare middle-age Americans’ health. A key measure is whether people have trouble with an “activity of daily living” (ADL), such as walking, dressing and bathing themselves, eating, or getting in or out of bed. The researchers observed that the number of middle-age Americans with ADL limitations has increased; 12.5% of Americans at the current retirement age of 66 had an ADL limitation in their late 50s, an increase from 8.8% for people with a retirement age of 65. At the current retirement age of 66, 25% of Americans age 58 to 60 rated themselves in “poor” or “fair” health. That’s up 2.6% from the group who could retire with full benefits at 65, the researchers found. Cognitive skills have also declined over time, according to the study. For those with a retirement age of 66, 11% already had some kind of dementia or other cognitive decline at age 58 to 60; an increase from 9.5% of Americans with a retirement age between 65 and 66. While death rates can fluctuate from year to year, this study is being added to a growing body of evidence that suggests the health of Americans deteriorating. References Choi, H. and Schoeni, R. (2017). Health Of Americans Who Must Work Longer To Reach Social Security Retirement Age. Health Affairs, 36(10), pp.1815-1819. https://doi.org/10.1377/hlthaff.2017.0217
Society of Actuaries. (2017). Mortality Improvement Scale 2017. [online] Available at: https://www.soa.org/Files/Research/Exp-Study/mortality-improvement-scale-mp-2017.pdf [Accessed 28 Oct. 2017]. Steverman, B. (2017). Americans Are Retiring Later, Dying Sooner and Sicker In-Between. [online] Bloomberg.com. Available at: https://www.bloomberg.com/news/articles/2017-10-23/americans-are-retiring-later-dying-sooner-and-sicker-in-between [Accessed 28 Oct. 2017]. |
The Awareness domain contains research, news, information, observations, and ideas at the level of self in an effort to intellectualize health concepts.
The Lifestyle domain builds off intellectual concepts and offers practical applications.
Taking care of yourself is at the core of the other domains because the others depend on your health and wellness.
Archives
May 2024
Categories
All
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||








 RSS Feed
RSS Feed

