|
This article challenges the conventional understanding of heart disease, particularly the widely accepted theory that attributes its cause primarily to events occurring in the coronary arteries. Instead, a paradigm shift is proposed, contending that a deeper understanding of heart disease, encompassing angina, unstable angina, and myocardial infarction (heart attack), necessitates a focus on events within the myocardium, the muscular tissue of the heart. Over the past decades, the prevailing belief in the coronary artery theory has led to costly surgical interventions, widespread medication use with questionable benefits, and dietary recommendations that may exacerbate rather than alleviate the problem. By delving into the precise pathophysiological events that underlie heart attacks, we can uncover alternative approaches to prevention and treatment, such as adopting a "Nourishing Traditions"-style diet and utilizing safe and affordable medicines like g-strophanthin. Furthermore, this shift in perspective prompts us to confront broader issues, including the impact of modern lifestyles on human health, the need for a new medical paradigm, and the importance of ecological consciousness. Ultimately, reexamining the root causes of heart disease offers a pathway to addressing this pervasive health challenge and forging a healthier future for all. The information is summarized based on the work of Dr. Thomas Cowan, vice president of the Physicians Association for Anthroposophical Medicine and is a founding board member of the Weston A. Price Foundation. During his career he has studied and written about many subjects in medicine. These include nutrition, homeopathy, anthroposophical medicine, and herbal medicine. Challenging the Conventional model: Revisiting the Causes of Heart AttacksThe traditional understanding of heart attacks, largely centered on arterial blockage due to plaque buildup, has faced challenges in recent years. Initially, it was believed that blockages in the major coronary arteries led to oxygen deficiency in the heart, causing chest pain (angina) and eventually progressing to a heart attack. This simplistic view prompted invasive procedures like angioplasty, stents, and coronary bypass surgery as standard treatments. However, clinical observations and research findings have cast doubts on this approach. Anecdotal evidence (admittedly low quality evidence) from a trial in rural Alabama revealed surprising outcomes among individuals with single artery blockages. Contrary to expectations, less than 10% of those who experienced heart attacks did so in the region of the heart supplied by the blocked artery. Similarly, a comprehensive study conducted by the Mayo Clinic highlighted the limited efficacy of bypass surgery in preventing future heart attacks. While the procedure offered relief from chest pain, it did not significantly reduce the risk of subsequent heart events, except in high-risk patients. Contrary to popular belief, blockages exceeding 90% are often compensated for by collateral blood vessels, which develop over time to ensure uninterrupted blood flow to the heart. This extensive network of collateral vessels serves as a natural bypass system, mitigating the impact of arterial blockages on blood circulation. However, diagnostic procedures like coronary angiograms, which rely on injecting heavy dye into the arteries, often fail to accurately assess the extent of blockages and the true blood flow in the heart. As a result, many patients undergo invasive treatments such as bypass surgery, stents, or angioplasty based on misleading information about the severity of their arterial blockages. Moreover, studies have shown that these procedures provide minimal benefit, if any, to patients, particularly those with minimally symptomatic blockages exceeding 90%. Despite the widespread use of these interventions, their efficacy in restoring blood flow and preventing heart attacks remains questionable. These revelations underscore the need for a reevaluation of conventional treatment strategies and a deeper exploration of the underlying mechanisms behind heart attacks. Rather than focusing solely on arterial blockages, a more holistic approach that considers factors beyond plaque buildup may offer greater insights into the prevention and management of heart disease. Beyond the Coronary Artery TheoryThe prevailing focus in cardiology has long been on the stable, progressing plaque within the coronary arteries, deemed responsible for heart attacks. However, recent insights challenge this notion, redirecting attention to the unpredictable nature of unstable plaques. Unlike their calcified counterparts, unstable plaques are soft and prone to rapid evolution, abruptly occluding arteries and triggering downstream oxygen deficits, angina, and ischemia. These vulnerable plaques are believed to be a blend of inflammatory buildup and low-density lipoprotein (LDL), the primary targets of statin drugs. Consequently, the widespread adoption of statin therapy is advocated as a preventive measure against heart attacks, fueled by angiogram studies purportedly showcasing the prevalence of unstable plaques as the leading cause of myocardial infarctions (MIs). Yet, autopsies and pathology studies present a different narrative. Thrombosis, deemed crucial in precipitating MIs, is found in only a fraction of cases upon meticulous examination. Furthermore, measurements of myocardial oxygen levels during MIs reveal no discernible deficit, challenging the conventional understanding of ischemia as the primary mechanism. While thrombosis does occur in conjunction with MIs, its occurrence in less than half of cases underscores the inadequacy of attributing MIs solely to arterial blockages. The timing of thrombosis, often post-MI, begs the question: what precipitated the event in the first place? These inconsistencies underscore the limitations of existing theories surrounding coronary artery involvement in MIs. As the spotlight shifts away from stable plaques, a pressing question emerges: What truly underlies the genesis of heart attacks? Unveiling the Autonomic Symphony: The Heart's Harmonious BalanceAn accurate understanding of myocardial ischemia necessitates consideration of the primary risk factors associated with heart disease, including gender, diabetes, smoking, and chronic psychological stress. Curiously, none of these risk factors directly implicate coronary artery pathology; instead, they impact capillary health or exert indirect effects. Over the past five decades, key medications in cardiology, such as beta-blockers, nitrates, aspirin, and statins, have demonstrated some benefits for heart patients. However, their mechanisms of action must be scrutinized within a comprehensive theory of myocardial ischemia. A groundbreaking revelation in heart disease prevention and treatment stems from the autonomic nervous system's role in ischemia genesis, as illuminated by heart-rate variability monitoring. The autonomic nervous system comprises two branches—the sympathetic and parasympathetic—responsible for regulating physiological responses. Imbalance between these branches emerges as a significant contributor to heart disease. Studies reveal a notable reduction in parasympathetic activity among patients with ischemic heart disease, particularly preceding ischemic events triggered by physical or emotional stressors. Conversely, abrupt increases in sympathetic activity rarely culminate in ischemia without antecedent parasympathetic decline. Notably, women exhibit stronger vagal activity than men, potentially influencing sex-based disparities in MI incidence. Multiple risk factors, including hypertension, smoking, diabetes, and stress, diminish parasympathetic activity, underscoring the pivotal role of the regenerative nervous system in heart health. Conversely, pharmacological interventions like nitrates, aspirin, and statins stimulate parasympathetic mediators, promoting ANS balance. In essence, while traditional risk factors and interventions influence plaque and stenosis development, their paramount impact lies in restoring ANS equilibrium. Thus, understanding the sequence of events leading to myocardial infarction demands a deeper exploration of autonomic nervous system dynamics. The Underlying pathophysiology of Myocardial IschemiaIn the vast majority of cases, the pathology leading to myocardial infarction (MI) begins with a decreased tonic activity of the parasympathetic nervous system (rest and digest), often exacerbated by physical or emotional stressors. This reduction prompts an increase in sympathetic nervous system activity, triggering heightened adrenaline production and directing myocardial cells to break down glucose via aerobic glycolysis, rather than their preferred fuel source of ketones and fatty acids (often explaining why patients report feeling tired before a MI). Remarkably, despite these metabolic shifts, no change in blood flow, as measured by the myocardial cell oxygen level (pO2), occurs. The shift towards glycolysis results in a surge of lactic acid production within myocardial cells, a phenomenon observed in nearly all MIs. This surge, coupled with localized tissue acidosis, impedes calcium entry into cells, compromising their contractility. Consequently, localized edema ensues, leading to hypokinesis—the hallmark of ischemic disease—and eventual tissue necrosis characteristic of an MI. Moreover, the ensuing tissue edema alters arterial hemodynamics, escalating sheer pressure and exacerbating plaque instability. This process elucidates the rupture of unstable plaques and their role in exacerbating arterial blockage during critical, acute scenarios. This explanation accounts for all the observable phenomena associated with heart disease. Understanding the etiology of heart disease holds profound implications beyond academic curiosity. It informs therapeutic strategies aimed at preserving parasympathetic activity, fostering holistic approaches to heart health, and challenging prevailing "civilized" industrial lifestyles. Central to this paradigm shift is the recognition of the vital role played by g-strophanthin—a hormone derived from the strophanthus plant. G-strophanthin is an endogenous hormone made in the adrenal cortex from cholesterol, whose production is inhibited by statin drugs, that does two things that are crucial for heart health and are done by no other medicine. G-strophanthin uniquely stimulates the production of acetylcholine, the primary neurotransmitter of the parasympathetic nervous system, while also converting lactic acid—the metabolic poison implicated in ischemic processes—into pyruvate, a preferred myocardial cell fuel. Perhaps this “magic” is why Chinese medicine practitioners say that the kidneys (i.e., adrenals, where ouabain is made) nourish the heart. Embracing this understanding not only guides therapeutic interventions but also underscores the imperative of dietary modifications. A diet abundant in healthful fats and fat-soluble nutrients, while low in processed carbohydrates and sugars, emerges as a cornerstone of heart health—a departure from the industrialized diets synonymous with modern civilization. In essence, unraveling the metabolic symphony orchestrating myocardial ischemia offers a transformative lens through which to perceive heart disease, fostering a holistic approach that transcends conventional paradigms and embraces the profound interconnectedness of mind, body, and environment. referencesGiorgio Baroldi. The Etiopathogenesis of Coronary Heart Disease. CRC Press EBooks, Informa, 20 Jan. 2004. Accessed 29 Mar. 2024.
Sroka K. On the genesis of myocardial ischemia. Z Kardiol. 2004 Oct;93(10):768-83. doi: 10.1007/s00392-004-0137-6. PMID: 15492892. Helfant, R. H., et al. “Coronary Heart Disease. Differential Hemodynamic, Metabolic, and Electrocardiographic Effects in Subjects with and without Angina Pectoris during Atrial Pacing.” Circulation, vol. 42, no. 4, 1 Oct. 1970, pp. 601–610, www.ncbi.nlm.nih.gov/pubmed/11993303., https://doi.org/10.1161/01.cir.42.4.601. Takase, B., Kurita, A., Noritake, M., Uehata, A., Maruyama, T., Nagayoshi, H., ... & Nakamura, H. (1992). Heart rate variability in patients with diabetes mellitus, ischemic heart disease, and congestive heart failure. Journal of electrocardiology, 25(2), 79-88. Sroka, K., Peimann, C. J., & Seevers, H. (1997). Heart rate variability in myocardial ischemia during daily life. Journal of electrocardiology, 30(1), 45-56. Scheuer, J., & Brachfeld, N. (1966). Coronary insufficiency: relations between hemodynamic, electrical, and biochemical parameters. Circulation Research, 18(2), 178-189. Schmid, P. G., Greif, B. J., Lund, D. D., & Roskoski Jr, R. O. B. E. R. T. (1978). Regional choline acetyltransferase activity in the guinea pig heart. Circulation Research, 42(5), 657-660. Katz, A. M. (1971). Effects of ischemia on the cardiac contractile proteins. Cardiology, 56(1-6), 276-283. Manunta, Paolo, et al. “Endogenous Ouabain in Cardiovascular Function and Disease.” Journal of Hypertension, vol. 27, no. 1, 1 Jan. 2009, pp. 9–18, journals.lww.com/jhypertension/Abstract/2009/01000/Endogenous_ouabain_in_cardiovascular_function_and.3.aspx, https://doi.org/10.1097/HJH.0b013e32831cf2c6. Doepp, Manfred. “May Strophanthin Be a Valuable Cardiac Drug ? .” American Journal of Medical and Clinical Research & Reviews, vol. 2, no. 9, 15 Sept. 2023, pp. 1–6, ajmcrr.com/index.php/pub/article/view/75/74, https://doi.org/10.58372/2835-6276.1069. Accessed 29 Mar. 2024. Thayer, J. F., Yamamoto, S. S., & Brosschot, J. F. (2010). The relationship of autonomic imbalance, heart rate variability and cardiovascular disease risk factors. International journal of cardiology, 141(2), 122-131.
0 Comments
As it turns out, researchers have observed that positive emotions influence endocrinological and immunological responses. In other words, experiencing stressful emotions, such as anger, depression, anxiety, or a state of unworthiness, has the potential to actually pull the genetic trigger, dysregulating cells and creating disease. In 2005, a group of Japanese researchers conducted a study to examine what effect one's mental state might have on disease. The participants consisted of two groups of patients with type 2 diabetes, all of whom were dependent on insulin, a hormone that enables glucose to enter cells to be used as energy. Fasting blood-sugar levels for each group was determined to establish a baseline. The researchers then exposed one of the groups to a comedy show for an hour, while the control group watched a boring lecture. Afterwards, both groups were instructed to consume food, after which their blood-sugar levels were checked again. Of the groups, there was a significant difference between those who watched the comedy show compared to those who viewed the lecture. The researchers measured the blood-sugar levels of those who watched the lecture and observed an average of 123 mg/dl - high enough that they would be required to take insulin. In the group that watched the comedy show, their postprandial blood-sugar levels rose only about half of that amount. The researchers set out to examine the mechanism for why this may be occurring. Initially, they hypothesized that the group experiencing laughter resulting in more time contracting their diaphragm and abdominal muscles, expending more energy, therefore resulting in the lower blood-glucose levels. Upon greater examination, the researchers analyzed the changes in expression of 18,716 genes from blood cells in the patients with type 2 diabetes, which were induced by laughter. Of the 18,716 genes, 23 genes showed significantly different expression changes after listening to the comic story compared to the boring lecture. Eight were relatively upregulated and 15 were downregulated 1.5 hours after the laughter occurred. As it turns out, of the group that experienced laughter, their elevated mental states apparently triggered their brains to send new chemical signals to their cells, activating the genetic sequences to allow their bodies to naturally begin regulating the genes responsible for processing blood sugar. In sum, the researchers demonstrated simply signaling the body with a positive emotion, such as laughter, is linked to gene expression. Emotions are capable of altering body chemistry and signaling new genes, altering their internal environment. And remember, we can create an emotion by thought alone. References Hayashi, T., Urayama, O., Kawai, K., Hayashi, K., Iwanaga, S., Ohta, M., Saito, T. and Murakami, K. (2005). Laughter Regulates Gene Expression in Patients with Type 2 Diabetes. Psychotherapy and Psychosomatics, 75(1), pp.62-65. https://doi.org/10.1159/000089228
Transcript:
Remember that time Ron believed that Harry gave him Liquid Luck? Felix Felicis, known in the wizarding world as Liquid Luck, is a magical potion that gives it’s drinker good fortune. For a period of time, everything the drinker attempts will be successful. So in the following scene we see Ron dominate the quidditch match, and become Gryffindor’s latest hero. But of course there’s a catch, Harry didn’t actually put the potion in Ron’s drink at all. This is a prime example of the placebo effect. A placebo is a treatment with no active therapeutic properties. And it’s often used as the control in clinical trials to test the effectiveness of new pharmaceutical drugs. But the effect refers to the physiological phenomenon that usually happens to the control group who was given the placebo treatment. Their condition improves in a way that is often comparable and sometimes even better than the control group, even though they weren’t given any drugs at all. In cases where the placebo outperforms the drug, researchers come to the conclusion that the pharmaceutical should be deemed ineffective. But why aren’t they more interested in the fact that these people are getting better with no medicine at all? It’s no secret that the healthcare industry needs sick people in order to turn over a profit. In a 2018 report, the investment banking company Goldman Sachs looked into the investment potential of biotech research companies who are attempting to create “one shot cures.” Their conclusion? Cures could be bad for business. They stated “While this proposition carries tremendous value for patients and society, it could represent a challenge for genome medicine developers looking for sustained cash flow.” So should we really be surprised that nobody’s putting money behind self-healing research? You can’t exactly put “belief” in tablet form and sell it to patients. But that’s sort of what placebos are. The examples of miraculous placebo effect results are pretty much endless, so we’ll just look at a few. In 2001, Irving Kirsch from Harvard Medical School used the Freedom of Information Act to obtain data of clinical trials of top antidepressants. He found that in over half of these trials, the drugs didn’t outperform the placebos, and concluded that 80% of the success in those trials was due to the placebo effect. Several studies have shown that the placebo effect can also affect physical performance. In one of these studies, a group of weight lifters were told that they were being given a legal anabolic steroid. Each of those athletes set all-time personal records in every exercise tested after being administered the fake steroid. So we have the ability to improve mental conditions and physical performance with our mind, but can the placebo effect go as far as surgery? According to this study published in the New England Journal of Medicine, yes. A group of 180 patients with osteoarthritis of the knee were split into three groups. One group underwent an operation that shaves down the damaged cartilage, one group received a flushing of the knee joint, and one group received a faux surgery. Complete with pre-op, post-op, small incisions on the knee to produce scars, and audio cues that an operation was taking place. And the results were startling, the patients were followed up with at various times throughout recovery with the last check-in being 24 months after surgery. The data showed that “At no point did either of the intervention groups report less pain or better function than the placebo group.” And they concluded, “Finally, health care researchers should not underestimate the placebo effect, regardless of its mechanism.” Some have argued that the placebo effect boils down to good old fashioned bedside manner. In fact, the Senior Medical Fellow at the American Council on Science and health has claimed that it really just goes back to the soul of medicine — ritual, symbolism, trust, hope, and compassion. And it’s true that the doctor-patient relationship plays a large role in the effectiveness of treatment. Patients with optimistic and compassionate doctors tend to fare better than those who receive treatment from unenthusiastic ones. But it’s doubtful that this can explain the magic of the placebo effect entirely. After all, there’s something going on physiologically. And to get a better understanding of just what that is, we’re going to have to dive a little deeper. Bruce Lipton is a cellular biologist who’s research gives us some insight into the mechanism that allows us to heal ourselves. Once upon a time, the planet was populated with single-celled organisms. They did alright for themselves, the protein building blocks of the cells acted as receptors and effectors that took in environmental information and responded accordingly. But after some time these cells started to join together, forming communities that acted as units. As a means of survival, special cells were tasked with acting as a centralized info processing system or what we would call a brain. In this way, highly evolved animals were able to take in even more information from the environment and relay it to all of the cells throughout the body. This was great for organizing the flow of signal molecules that regulate the cells’ behaviors.But it also meant that individual cells had to relinquish control to the brain. And as proud owners of these brains, we can all attest that sometimes our mind generates emotions that are unrelated to our environment and definitely not necessary or conducive to our survival. And these emotion are so strong that they have the ability to override the system. So that’s great news, right? We can just think happy, healthy, positive thoughts to override the system and cure ourselves of any disease. Well, not exactly. There’s an important distinction to be made about the instructions that our mind is sending to the rest of our body. Some are coming from our conscious mind, but most are coming from our subconscious mind. And unfortunately, the one that we have control over is only driving the bus about 5% of the time. Our conscious mind is where we generate thoughts, but our subconscious mind is actually where most of our instructions are coming from whether we realize it or not. Our subconscious mind acts out of habits and experiences that are formed over a lifetime, but most of which are programmed before we even reach adolescence. It’s where we store all of our fears and past traumas, so it’s no surprise that it might be operating under disempowering programs which conflict with the best intentions of our conscious mind. But it isn’t all doom and gloom. Dr. Lipton believes that these programs can be easily overwritten through things like meditation, hypnotherapy, and various other forms of energy psychologies. But how could these woo woo sounding modalities possibly work better than the chemicals that directly alter the functions and behaviors of particular cells? It turns out that cells respond much better to energy signals than they do to chemical signals. When a chemical bond is made, most of the cell’s energy is wasted through chemical coupling. So very little energy is left to take in information and respond to the signal. On the other hand, energy signals link with a cell’s available energy to relay environmental information which according to Oxford biologist C.W.F. McLare makes them 100% more efficient at receiving and responding to signals. So now the placebo effect results aren’t such a mystery. We see why simply thinking our health will improve can be just as, if not more powerful than a chemical telling our cells to do something different. After all, thoughts are just energetic vibrations. Now all of this isn’t to say that pharmaceuticals shouldn’t have a place in modern medicine or that every disease can be cured simply by positive thinking. But it is important to recognize that we have powerful internal resources to call upon and integrate into our overall health. Humans have an innate desire to believe in magic. That’s why it’s so tempting to turn to magical pills and potions when something in our life isn’t going the way we want it to. But just like we saw before, magic doesn’t necessarily require wands and spells. We’re the drivers of our biology, and we have the ability to rewrite our data. The magic is already within us.
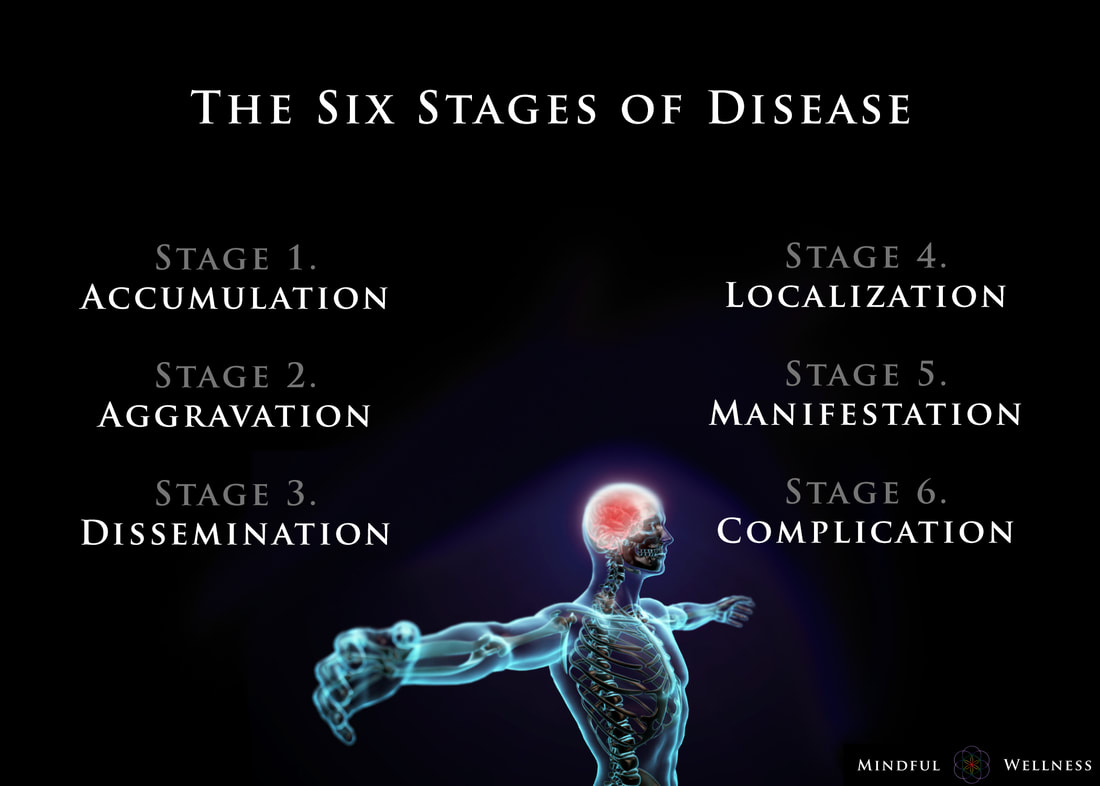
Ayurveda offers insight into the earlier stages and enables those monitoring their health to take care of any small imbalances well before developing any serious illness. The length of the each stage may vary from weeks, to months, even years, depending on the person and the degree of aggravation. The six stages of disease development are:
1. Accumulation The first stage, accumulation, represents imbalance, a build up or collection of something in the body. Being exposed to and acquiring a pathogen via the external environment is an example of accumulation. This stage can also be caused by the internal environment, such as from eating an imbalanced diet leading to excess inflammation or mucous. Accumulation in the body leads to the the next stage, aggravation. 2. Aggravation As the imbalanced elements continue to increase, the symptoms become more aggravated and will begin to be noticed throughout the body. This stage is a sign of continued accumulation. This stage can manifest, as seen in the Kapha state, as loss of appetite, indigestion, nausea, excess saliva, oversleeping, sluggishness; or as seen in the Pitta state, as increased acidity, burning sensations in the abdomen, lowered vitality, or insomnia; or as seen in the Vata state, as pain in the lower abdomen, excess flatulence, and light-headedness. 3. dissemination Once the site of origin is full with excess accumulation and is aggravated, it will begin to overflow into or disseminate throughout the rest of the body using different channels of transportation. Overflow typically begins in the GI tract, then spilling into the circulating plasma and blood, allowing the accumulation to spread systemically, and eventually seeping into the organs and tissues (dhātus). Simultaneously, the symptoms at the site of origin will grow worse. 4. Localization The excess accumulation will then move to wherever a weak site exists in the body. This is where and when diseases begin to develop. This stage is also where genetics matter; the weak spots are determined by genetics - as the saying goes, genetics loads the gun, environment pulls the trigger. This stage can manifest, as seen in the Vata state, as arthritis. In a Pitta state, this can be seen as an ulcer, and in the Kapha state, manifestation may begin in the lungs. At this stage, healing is still regarded as simple. 5. Manifestation This is the first state of the development of illness for which modern Western medicine can detect signs of disease. It is at this stage where diseases progress and become fully developed, showing signs of clinical features. Manifested imbalances are given names at this stage, such as arthrosclerosis, cancer, colitis, etc. It is at this stage where conventional medicine attempts to mask the symptoms by offering pharmaceutical drugs. 6. Complication Complications of the dis-ease begin at this final stage. Often times, conventional medicine attempts to solve the problem by simply removing the affected tissue (e.g., small intenstine, colon, thyroid, etc.) from the body. The symptoms become clear enough so that the elemental cause (i.e., dosha constitution such as Vata, Kapha, Pitta) may be determined. Some medical professionals describe this stage as the chronic phase of development. For example, if one develops inflammation in the manifestation stage, in this stage, complications set in, and the inflammation may grow worse into a chronic problem. Being aware of the stages of the dis-ease process is helpful because one can gain a better understanding in how prevent, and perhaps even reverse, it. To be clear, the information provided here is not claiming to treat, cure or diagnose disease. ReferencesCabral, S. (2018). The 6 Stages of the Disease Process (Ayurvedic Principle). [podcast] The Cabral Concept. Available at: https://itunes.apple.com/us/podcast/cabral-concept-by-stephen/id1071469441?mt=2
Tirtha, S. (2007). The Āyuveda encyclopedia. Bayville, NY. Ayurveda Holistic Center Press. Welcome to the first episode of our brand new docuseries - Remedy: Ancient Medicine for Modern Illness.
(If you are not registered for the full Remedy docuseries yet, click this link to join us for all 9 episodes - https://remedy.thesacredscience.com/r... ) Episode 1 is called “The Quest For Lost Medicine” and it lays the groundwork for the entire series - some of what you will witness may shock you… Over the 9-part Remedy series, we’ll be uncovering powerful herbal remedies for major diseases - but first, we need to understand why this vital healing information has been kept from us. Here’s some of what we will reveal in this first episode…
This eye-opening episode sets the stage for everything else we cover in the Remedy docuseries. Again, if you are not registered for the full series, click here - https://remedy.thesacredscience.com/r... Wim Hof is an autodidact and taught himself how to control his heart rate, breathing and blood circulation. All this is regulated by the autonomic nervous system. Conventional science says that the autonomic nervous system is a part of the body you just can´t control, yet Wim can, by steering his hypothalamus (an area in the brain which regulates the body temperature). Where the body temperature of an untrained person drops dangerously after exposing it to extreme cold, Wim is able to retain his core temperature around 37 degrees Celsius, constantly. Even after 1 hour and 52 minutes sitting in ice, Wim’s core temperature stays the same. Scientists around the world baffled by this exceptional performance. In the Netherlands, Prof. Maria Hopman of the UMC St Radboud Nijmegen examined Wim’s physiology as he was affected by the cold, while he was up to his neck in a cylinder filled with ice cubes.
Wim Hof, aka "The Iceman" holds the world record for the longest ice bath lasting over one hour and 52 minutes and 20 other world records for feats performed while withstanding the cold. He has climbed Mount Everest and Mount Kilimanjaro in just shorts and shoes. His method enables him to control his core body temperature and immune system, which can be learned by anyone including. Wim's ultimate goals are to end all disease to facilitate a paradigm shift towards health to promote care for our planet and to bring back love and happiness for all people by encouraging them to get in touch with the cold, and he plans to do all this under the scrutiny of science. A growing body of evidence suggests that exercise is one of the most effective prevention and treatment strategies for depression. A recent study, conducted over the course of 11 years, was designed to address whether exercise provides protection against new-onset depression and anxiety and if so, the intensity and amount of exercise required to gain protection and, lastly, the mechanisms that underlie any association. Researchers evaluated and followed 33,908 adults, which were selected on the basis of having no symptoms of common mental disorder or limiting physical health conditions. The researchers observed that regular leisure-time exercise was associated with reduced incidence of future depression but not anxiety. The majority of this protective effect occurred at low levels of exercise and was observed regardless of intensity. After adjusting for confounding variables, the results suggests that 12% of future cases of depression could have been prevented if all participants had engaged in at least 1 hour of physical activity each week. The social and physical health benefits of exercise explained a small proportion of the protective effect. ReferencesHarvey, S., Øverland, S., Hatch, S., Wessely, S., Mykletun, A. and Hotopf, M. (2017). Exercise and the Prevention of Depression: Results of the HUNT Cohort Study. American Journal of Psychiatry, pp.appi.ajp.2017.1. https://doi.org/10.1176/appi.ajp.2017.16111223
|
The Awareness domain contains research, news, information, observations, and ideas at the level of self in an effort to intellectualize health concepts.
The Lifestyle domain builds off intellectual concepts and offers practical applications.
Taking care of yourself is at the core of the other domains because the others depend on your health and wellness.
Archives
May 2024
Categories
All
|


 RSS Feed
RSS Feed

