|
Since the declaration of the COVID-19 pandemic by the World Health Organization (WHO) on March 11, 2020, over 13.5 billion doses of COVID-19 vaccines have been administered worldwide. This remarkable achievement in vaccine distribution highlights the urgent need for comprehensive vaccine safety monitoring, as very rare adverse events associated with COVID-19 vaccines may only become apparent after widespread administration. To address this need, the Safety Platform for Emergency Vaccines (SPEAC) initiative formulated a list of potential COVID-19 vaccine adverse events of special interest (AESI) in 2020. These AESI were selected based on various factors, including their associations with immunization, vaccine platforms, or adjuvants, as well as theoretical concerns related to immunopathogenesis. One flexible approach for assessing AESI is the comparison of observed AESI rates following vaccine introduction with expected rates based on historical periods pre-vaccine rollout. This method, known as observed vs. expected (OE) analysis, can rapidly detect potential vaccine safety signals. For example, OE analysis played a crucial role in identifying thrombosis with thrombocytopenia syndrome (TTS) as a safety signal, prompting the suspension of the AstraZeneca COVID-19 vaccine in certain countries. To further enhance vaccine safety monitoring, a global cohort study was conducted as part of the Global COVID Vaccine Safety (GCoVS) Project. This project, funded by the Centers for Disease Control and Prevention (CDC), involves multiple nations and aims to monitor COVID-19 vaccine safety on a global scale. Thirteen AESI were selected for evaluation, including neurological, hematologic, and cardiovascular conditions, which are as follows:
The study analyzed data from 10 sites across eight countries, comprising a total vaccinated population of 99,068,901 individuals. Notable findings include a statistically significant increase in Guillain-Barré syndrome (GBS) cases following the administration of the ChAdOx1 (India) vaccine and an increased risk of acute disseminated encephalomyelitis (ADEM) after the mRNA-1273 vaccine (Moderna). Hematologic conditions such as cerebral venous sinus thrombosis (CVST) and immune thrombocytopenia (ITP) also showed elevated risk ratios following certain vaccine doses. Similarly, cardiovascular conditions like myocarditis and pericarditis demonstrated increased risk ratios, particularly after mRNA vaccine doses (Pfizer, Moderna, AstraZeneca). Here is the raw data collected from the study: Here is a chart summarizing the raw data collected in the study: Overall, these findings underscore the importance of ongoing vaccine safety monitoring and highlight the value of global collaboration in assessing vaccine-related adverse events. By leveraging methodologies such as OE analysis and conducting comprehensive cohort studies, public health agencies can swiftly detect and respond to potential vaccine safety signals, ensuring the continued safety and effectiveness of COVID-19 vaccination efforts worldwide. referencesK. Faksova, et al. “COVID-19 Vaccines and Adverse Events of Special Interest: A Multinational Global Vaccine Data Network (GVDN) Cohort Study of 99 Million Vaccinated Individuals.” Vaccine, 1 Feb. 2024, https://doi.org/10.1016/j.vaccine.2024.01.100.
0 Comments
This article challenges the conventional understanding of heart disease, particularly the widely accepted theory that attributes its cause primarily to events occurring in the coronary arteries. Instead, a paradigm shift is proposed, contending that a deeper understanding of heart disease, encompassing angina, unstable angina, and myocardial infarction (heart attack), necessitates a focus on events within the myocardium, the muscular tissue of the heart. Over the past decades, the prevailing belief in the coronary artery theory has led to costly surgical interventions, widespread medication use with questionable benefits, and dietary recommendations that may exacerbate rather than alleviate the problem. By delving into the precise pathophysiological events that underlie heart attacks, we can uncover alternative approaches to prevention and treatment, such as adopting a "Nourishing Traditions"-style diet and utilizing safe and affordable medicines like g-strophanthin. Furthermore, this shift in perspective prompts us to confront broader issues, including the impact of modern lifestyles on human health, the need for a new medical paradigm, and the importance of ecological consciousness. Ultimately, reexamining the root causes of heart disease offers a pathway to addressing this pervasive health challenge and forging a healthier future for all. The information is summarized based on the work of Dr. Thomas Cowan, vice president of the Physicians Association for Anthroposophical Medicine and is a founding board member of the Weston A. Price Foundation. During his career he has studied and written about many subjects in medicine. These include nutrition, homeopathy, anthroposophical medicine, and herbal medicine. Challenging the Conventional model: Revisiting the Causes of Heart AttacksThe traditional understanding of heart attacks, largely centered on arterial blockage due to plaque buildup, has faced challenges in recent years. Initially, it was believed that blockages in the major coronary arteries led to oxygen deficiency in the heart, causing chest pain (angina) and eventually progressing to a heart attack. This simplistic view prompted invasive procedures like angioplasty, stents, and coronary bypass surgery as standard treatments. However, clinical observations and research findings have cast doubts on this approach. Anecdotal evidence (admittedly low quality evidence) from a trial in rural Alabama revealed surprising outcomes among individuals with single artery blockages. Contrary to expectations, less than 10% of those who experienced heart attacks did so in the region of the heart supplied by the blocked artery. Similarly, a comprehensive study conducted by the Mayo Clinic highlighted the limited efficacy of bypass surgery in preventing future heart attacks. While the procedure offered relief from chest pain, it did not significantly reduce the risk of subsequent heart events, except in high-risk patients. Contrary to popular belief, blockages exceeding 90% are often compensated for by collateral blood vessels, which develop over time to ensure uninterrupted blood flow to the heart. This extensive network of collateral vessels serves as a natural bypass system, mitigating the impact of arterial blockages on blood circulation. However, diagnostic procedures like coronary angiograms, which rely on injecting heavy dye into the arteries, often fail to accurately assess the extent of blockages and the true blood flow in the heart. As a result, many patients undergo invasive treatments such as bypass surgery, stents, or angioplasty based on misleading information about the severity of their arterial blockages. Moreover, studies have shown that these procedures provide minimal benefit, if any, to patients, particularly those with minimally symptomatic blockages exceeding 90%. Despite the widespread use of these interventions, their efficacy in restoring blood flow and preventing heart attacks remains questionable. These revelations underscore the need for a reevaluation of conventional treatment strategies and a deeper exploration of the underlying mechanisms behind heart attacks. Rather than focusing solely on arterial blockages, a more holistic approach that considers factors beyond plaque buildup may offer greater insights into the prevention and management of heart disease. Beyond the Coronary Artery TheoryThe prevailing focus in cardiology has long been on the stable, progressing plaque within the coronary arteries, deemed responsible for heart attacks. However, recent insights challenge this notion, redirecting attention to the unpredictable nature of unstable plaques. Unlike their calcified counterparts, unstable plaques are soft and prone to rapid evolution, abruptly occluding arteries and triggering downstream oxygen deficits, angina, and ischemia. These vulnerable plaques are believed to be a blend of inflammatory buildup and low-density lipoprotein (LDL), the primary targets of statin drugs. Consequently, the widespread adoption of statin therapy is advocated as a preventive measure against heart attacks, fueled by angiogram studies purportedly showcasing the prevalence of unstable plaques as the leading cause of myocardial infarctions (MIs). Yet, autopsies and pathology studies present a different narrative. Thrombosis, deemed crucial in precipitating MIs, is found in only a fraction of cases upon meticulous examination. Furthermore, measurements of myocardial oxygen levels during MIs reveal no discernible deficit, challenging the conventional understanding of ischemia as the primary mechanism. While thrombosis does occur in conjunction with MIs, its occurrence in less than half of cases underscores the inadequacy of attributing MIs solely to arterial blockages. The timing of thrombosis, often post-MI, begs the question: what precipitated the event in the first place? These inconsistencies underscore the limitations of existing theories surrounding coronary artery involvement in MIs. As the spotlight shifts away from stable plaques, a pressing question emerges: What truly underlies the genesis of heart attacks? Unveiling the Autonomic Symphony: The Heart's Harmonious BalanceAn accurate understanding of myocardial ischemia necessitates consideration of the primary risk factors associated with heart disease, including gender, diabetes, smoking, and chronic psychological stress. Curiously, none of these risk factors directly implicate coronary artery pathology; instead, they impact capillary health or exert indirect effects. Over the past five decades, key medications in cardiology, such as beta-blockers, nitrates, aspirin, and statins, have demonstrated some benefits for heart patients. However, their mechanisms of action must be scrutinized within a comprehensive theory of myocardial ischemia. A groundbreaking revelation in heart disease prevention and treatment stems from the autonomic nervous system's role in ischemia genesis, as illuminated by heart-rate variability monitoring. The autonomic nervous system comprises two branches—the sympathetic and parasympathetic—responsible for regulating physiological responses. Imbalance between these branches emerges as a significant contributor to heart disease. Studies reveal a notable reduction in parasympathetic activity among patients with ischemic heart disease, particularly preceding ischemic events triggered by physical or emotional stressors. Conversely, abrupt increases in sympathetic activity rarely culminate in ischemia without antecedent parasympathetic decline. Notably, women exhibit stronger vagal activity than men, potentially influencing sex-based disparities in MI incidence. Multiple risk factors, including hypertension, smoking, diabetes, and stress, diminish parasympathetic activity, underscoring the pivotal role of the regenerative nervous system in heart health. Conversely, pharmacological interventions like nitrates, aspirin, and statins stimulate parasympathetic mediators, promoting ANS balance. In essence, while traditional risk factors and interventions influence plaque and stenosis development, their paramount impact lies in restoring ANS equilibrium. Thus, understanding the sequence of events leading to myocardial infarction demands a deeper exploration of autonomic nervous system dynamics. The Underlying pathophysiology of Myocardial IschemiaIn the vast majority of cases, the pathology leading to myocardial infarction (MI) begins with a decreased tonic activity of the parasympathetic nervous system (rest and digest), often exacerbated by physical or emotional stressors. This reduction prompts an increase in sympathetic nervous system activity, triggering heightened adrenaline production and directing myocardial cells to break down glucose via aerobic glycolysis, rather than their preferred fuel source of ketones and fatty acids (often explaining why patients report feeling tired before a MI). Remarkably, despite these metabolic shifts, no change in blood flow, as measured by the myocardial cell oxygen level (pO2), occurs. The shift towards glycolysis results in a surge of lactic acid production within myocardial cells, a phenomenon observed in nearly all MIs. This surge, coupled with localized tissue acidosis, impedes calcium entry into cells, compromising their contractility. Consequently, localized edema ensues, leading to hypokinesis—the hallmark of ischemic disease—and eventual tissue necrosis characteristic of an MI. Moreover, the ensuing tissue edema alters arterial hemodynamics, escalating sheer pressure and exacerbating plaque instability. This process elucidates the rupture of unstable plaques and their role in exacerbating arterial blockage during critical, acute scenarios. This explanation accounts for all the observable phenomena associated with heart disease. Understanding the etiology of heart disease holds profound implications beyond academic curiosity. It informs therapeutic strategies aimed at preserving parasympathetic activity, fostering holistic approaches to heart health, and challenging prevailing "civilized" industrial lifestyles. Central to this paradigm shift is the recognition of the vital role played by g-strophanthin—a hormone derived from the strophanthus plant. G-strophanthin is an endogenous hormone made in the adrenal cortex from cholesterol, whose production is inhibited by statin drugs, that does two things that are crucial for heart health and are done by no other medicine. G-strophanthin uniquely stimulates the production of acetylcholine, the primary neurotransmitter of the parasympathetic nervous system, while also converting lactic acid—the metabolic poison implicated in ischemic processes—into pyruvate, a preferred myocardial cell fuel. Perhaps this “magic” is why Chinese medicine practitioners say that the kidneys (i.e., adrenals, where ouabain is made) nourish the heart. Embracing this understanding not only guides therapeutic interventions but also underscores the imperative of dietary modifications. A diet abundant in healthful fats and fat-soluble nutrients, while low in processed carbohydrates and sugars, emerges as a cornerstone of heart health—a departure from the industrialized diets synonymous with modern civilization. In essence, unraveling the metabolic symphony orchestrating myocardial ischemia offers a transformative lens through which to perceive heart disease, fostering a holistic approach that transcends conventional paradigms and embraces the profound interconnectedness of mind, body, and environment. referencesGiorgio Baroldi. The Etiopathogenesis of Coronary Heart Disease. CRC Press EBooks, Informa, 20 Jan. 2004. Accessed 29 Mar. 2024.
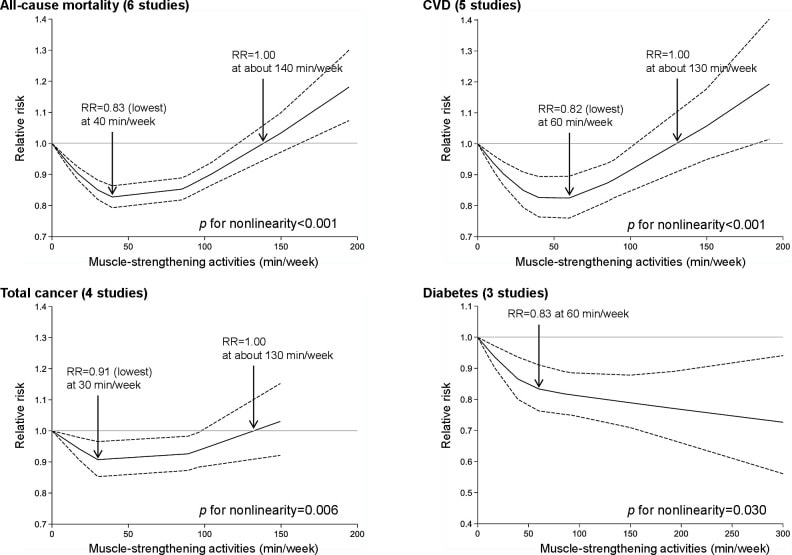
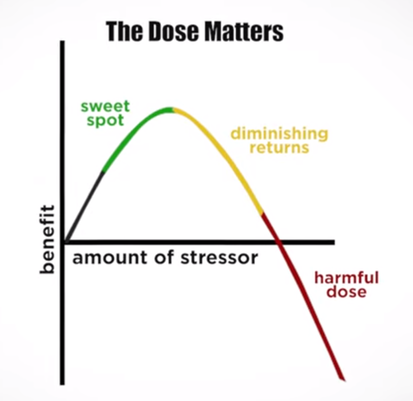
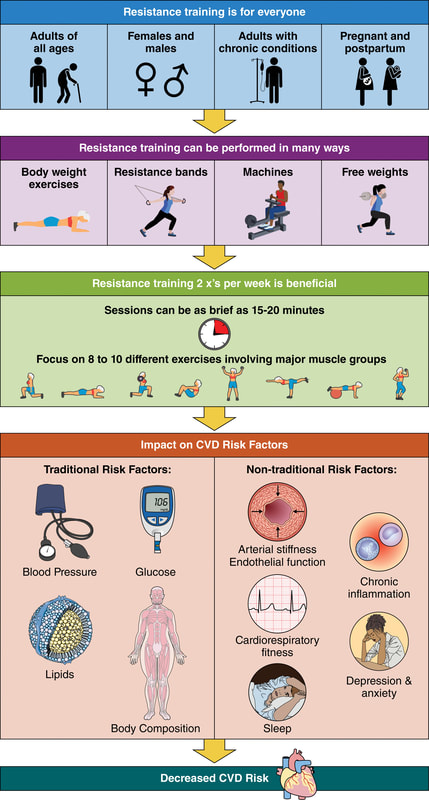
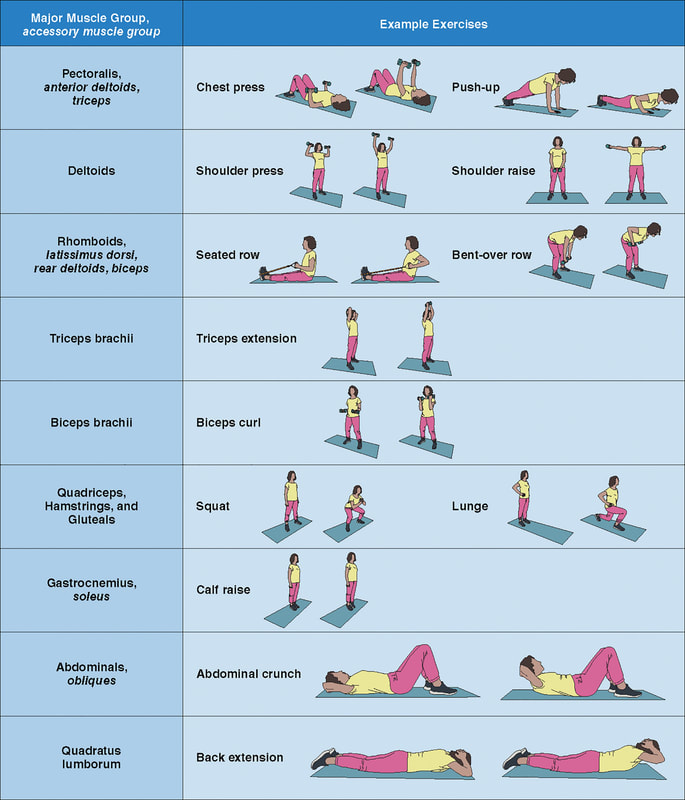
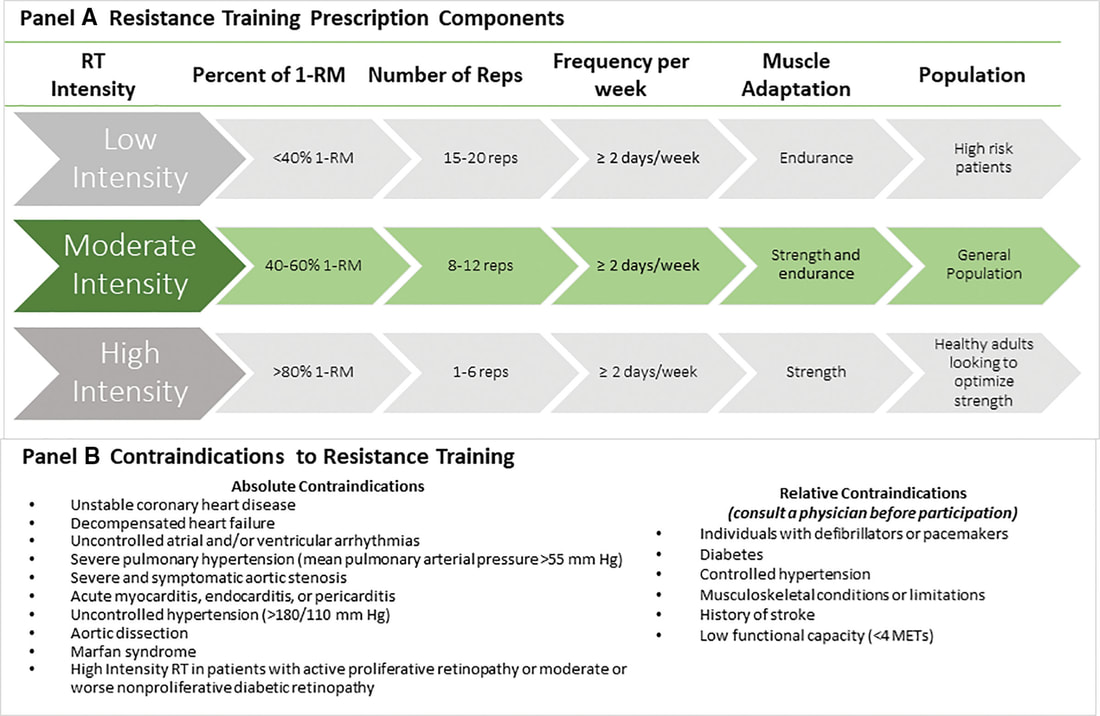
Sroka K. On the genesis of myocardial ischemia. Z Kardiol. 2004 Oct;93(10):768-83. doi: 10.1007/s00392-004-0137-6. PMID: 15492892. Helfant, R. H., et al. “Coronary Heart Disease. Differential Hemodynamic, Metabolic, and Electrocardiographic Effects in Subjects with and without Angina Pectoris during Atrial Pacing.” Circulation, vol. 42, no. 4, 1 Oct. 1970, pp. 601–610, www.ncbi.nlm.nih.gov/pubmed/11993303., https://doi.org/10.1161/01.cir.42.4.601. Takase, B., Kurita, A., Noritake, M., Uehata, A., Maruyama, T., Nagayoshi, H., ... & Nakamura, H. (1992). Heart rate variability in patients with diabetes mellitus, ischemic heart disease, and congestive heart failure. Journal of electrocardiology, 25(2), 79-88. Sroka, K., Peimann, C. J., & Seevers, H. (1997). Heart rate variability in myocardial ischemia during daily life. Journal of electrocardiology, 30(1), 45-56. Scheuer, J., & Brachfeld, N. (1966). Coronary insufficiency: relations between hemodynamic, electrical, and biochemical parameters. Circulation Research, 18(2), 178-189. Schmid, P. G., Greif, B. J., Lund, D. D., & Roskoski Jr, R. O. B. E. R. T. (1978). Regional choline acetyltransferase activity in the guinea pig heart. Circulation Research, 42(5), 657-660. Katz, A. M. (1971). Effects of ischemia on the cardiac contractile proteins. Cardiology, 56(1-6), 276-283. Manunta, Paolo, et al. “Endogenous Ouabain in Cardiovascular Function and Disease.” Journal of Hypertension, vol. 27, no. 1, 1 Jan. 2009, pp. 9–18, journals.lww.com/jhypertension/Abstract/2009/01000/Endogenous_ouabain_in_cardiovascular_function_and.3.aspx, https://doi.org/10.1097/HJH.0b013e32831cf2c6. Doepp, Manfred. “May Strophanthin Be a Valuable Cardiac Drug ? .” American Journal of Medical and Clinical Research & Reviews, vol. 2, no. 9, 15 Sept. 2023, pp. 1–6, ajmcrr.com/index.php/pub/article/view/75/74, https://doi.org/10.58372/2835-6276.1069. Accessed 29 Mar. 2024. Thayer, J. F., Yamamoto, S. S., & Brosschot, J. F. (2010). The relationship of autonomic imbalance, heart rate variability and cardiovascular disease risk factors. International journal of cardiology, 141(2), 122-131. In an update to its 2007 scientific statement, the American Heart Association (AHA) emphasizes the significant and multifaceted benefits of resistance training (RT) on cardiovascular health. Contrary to the misconception that RT solely enhances muscle mass and strength, the statement highlights the favorable physiological and clinical effects of this form of exercise on cardiovascular disease (CVD) and associated risk factors. The scientific statement aims to provide comprehensive insights into the impact of RT, either alone or in combination with aerobic training, on traditional and nontraditional CVD risk factors. More is not always betterEpidemiological evidence suggests that RT is associated with a lower risk of all-cause mortality and CVD morbidity and mortality. Adults who participate in RT have ≈15% lower risk of all-cause mortality and 17% lower risk of CVD, compared with adults who report no RT. Approximately 30 to 60 minutes per week of RT is associated with the maximum risk reduction for all-cause mortality and incident CVD. Notice this "U" shape in the curve when examining the relationship between RT and morbidity and mortality. This curve suggests that some RT is clearly beneficial, but has the volume of RT increases past a certain point the benefits drop and it becomes harmful. The concept of a "biphasic response" is fundamental to understanding hormesis. It describes the characteristic dose-response relationship observed in hormetic processes, where a substance or stressor elicits opposite effects at low and high doses. The response can be visualized as a U-shaped or J-shaped curve, illustrating the beneficial effects at low doses and potential harm at higher doses. Benefits of RT on Traditional CVD Risk FactorsThe AHA's scientific statement underscores the positive influence of RT on traditional CVD risk factors, including blood pressure (BP), glycemia, lipid profiles, and body composition. Numerous studies indicate that engaging in RT is associated with reduced resting BP, improved glycemic control, and favorable alterations in lipid profiles, contributing to a lower risk of all-cause mortality and CVD morbidity. Despite recommendations suggesting 2 days per week of RT, only 28% of U.S. adults adhere to this guideline, highlighting the need for increased awareness and promotion. RT and resting blood pressureRT has demonstrated the ability to reduce resting BP across diverse populations, with notable benefits observed in individuals with prehypertension and hypertension. The mechanisms behind these benefits include enhancements in endothelial function, vasodilatory capacity, and vascular conductance. The reductions in BP achieved through RT are comparable to those achieved with antihypertensive medications. RT and GlycemiaRT shows promise in improving glycemia and insulin resistance, leading to a lower incidence of diabetes. The evidence suggests a nonlinear dose-response association, with up to 60 minutes per week of RT associated with the maximum risk reduction for diabetes. RT and Lipid ProfilesWhile the effect on lipid profiles is modest, RT results in favorable changes in high-density lipoprotein cholesterol, total cholesterol, and triglycerides. These improvements are more pronounced in older adults and those with elevated cardiometabolic risk. Rt, Body composition, and weightRT positively influences body composition by increasing lean body mass and reducing body fat percentage. It is particularly effective in overweight or obese individuals, contributing to increased metabolic rate and mitigating weight gain over time. Benefits of RT on Nontraditional CVD Risk FactorsIn addition to traditional risk factors, the scientific statement highlights the potential mechanisms by which RT positively affects nontraditional CVD risk factors. These include increased cardiorespiratory fitness, improved endothelial function, and potential benefits for sleep quality, psychological health, and well-being. The AHA's updated scientific statement reinforces the pivotal role of resistance training in cardiovascular health, providing a comprehensive overview of its impact on both traditional and nontraditional risk factors. As the evidence supporting RT's benefits continues to grow, the statement serves as a valuable resource for clinicians and public health professionals, offering practical strategies for promoting and prescribing resistance training to enhance cardiovascular health in diverse populations. ReferencesPaluch, Amanda E, et al. “Resistance Exercise Training in Individuals with and without Cardiovascular Disease: 2023 Update: A Scientific Statement from the American Heart Association.” Circulation, 7 Dec. 2023, https://doi.org/10.1161/cir.0000000000001189. Accessed 11 Dec. 2023.
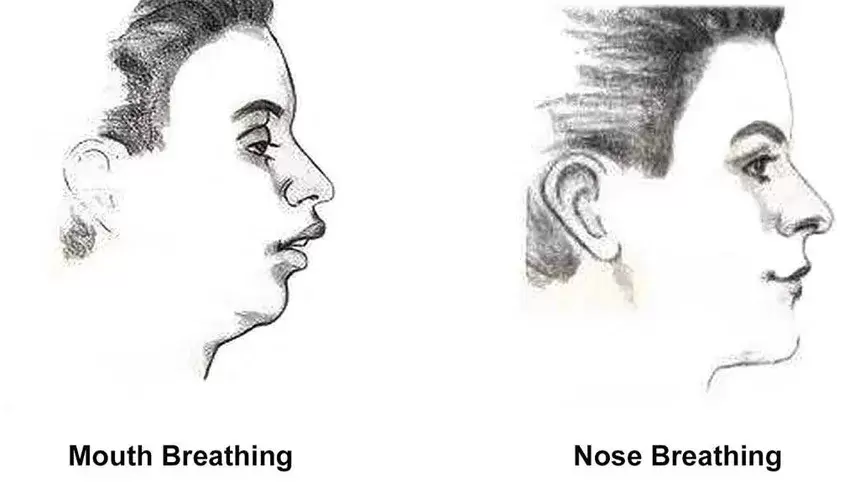
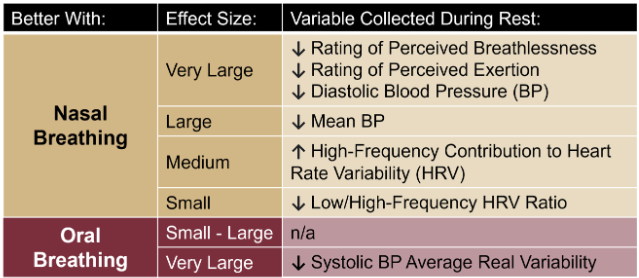
Momma H, Kawakami R, Honda T, Sawada SS. Muscle-strengthening activities are associated with lower risk and mortality in major non-communicable diseases: a systematic review and meta-analysis of cohort studies. Br J Sports Med. 2022 Jul;56(13):755-763. doi: 10.1136/bjsports-2021-105061. Epub 2022 Feb 28. PMID: 35228201; PMCID: PMC9209691. Nasal Breathing: A Breath of Fresh Air for Cardiovascular Wellness – Insights from New Research2/4/2024 The leading cause of death in the United States is cardiovascular disease, and the risk of cardiovascular issues can be predicted by factors such as blood pressure, heart rate variability, blood pressure variability, and cardiac vagal baroreflex sensitivity. The interplay between the cardiovascular and respiratory systems is highlighted, with a particular emphasis on how respiration affects key prognostic cardiovascular variables. This study explores the impact of nasal breathing compared to oral breathing on cardiovascular health in young adults. Nasal breathing is associated with humidification, warming, and filtration of inhaled air, potentially leading to bronchodilation and improved breathing efficiency. While past research has shown nasal breathing to have positive effects on resting metabolic demands, its influence on cardiovascular markers is not well-understood. The primary hypothesis is that nasal breathing, as opposed to oral breathing, will result in decreased blood pressure, improved heart rate variability, reduced blood pressure variability, and increased cardiac vagal baroreflex sensitivity at rest. The study aims to contribute to the understanding of how breathing patterns influence prognostic cardiovascular variables, aligning with the broader interest in the impact of breathing pace and training on cardiovascular health. The secondary hypothesis focuses on the effects of nasal breathing during submaximal exercise. The expectation is that nasal breathing, by attenuating the ventilatory response and metabolic demands, will lead to reduced blood pressure responses, improved heart rate variability, and decreased blood pressure variability during exercise. This aspect is particularly relevant due to the association between elevated exercise blood pressure and the risk of developing hypertension and cardiovascular disease. FindingsThe study findings are summarized, focusing on the impact of nasal vs. oral breathing on physiological and subjective variables at rest and during exercise. At rest, nasal breathing is associated with lower mean and diastolic blood pressure, improved heart rate variability metrics, reduced LF/HF ratio, and lower ratings of perceived exertion (RPE) and breathlessness (RPB). However, it increased systolic blood pressure average real variability. During submaximal exercise, differences between nasal and oral breathing were observed for RPB, suggesting a modest effect on reducing breathlessness during acute exercise. The discussion delves into the potential clinical significance of these findings, particularly the reduction in diastolic blood pressure during nasal breathing at rest. The study suggests a greater parasympathetic to sympathetic dominance during nasal breathing, indicated by changes in frequency-domain metrics of heart rate variability. Although nasal breathing did not significantly affect beat-to-beat blood pressure variability, there is speculation about potential connections between respiratory variables and blood pressure changes, emphasizing the need for further investigation. The study notes that the impact of nasal breathing on cardiovascular variables may have implications for various populations and suggests avenues for future research, including examining nasal breathing's effects on blood pressure over longer durations, both at rest and during activities like exercise. The discussion also touches on the potential benefits of interventions like mouth-taping overnight, emphasizing the importance of considering nasal breathing in the context of broader health outcomes. In summary, the study highlights the potential benefits of nasal breathing, with improvements in various cardiovascular and subjective measures at rest. While the effects during exercise are more modest, the findings contribute to understanding the nuanced relationship between respiratory patterns and cardiovascular health. referencesWatso, Joseph C., et al. “Acute Nasal Breathing Lowers Diastolic Blood Pressure and Increases Parasympathetic Contributions to Heart Rate Variability in Young Adults.” American Journal of Physiology. Regulatory, Integrative and Comparative Physiology, vol. 325, no. 6, 1 Dec. 2023, pp. R797–R808, pubmed.ncbi.nlm.nih.gov/37867476/, https://doi.org/10.1152/ajpregu.00148.2023.
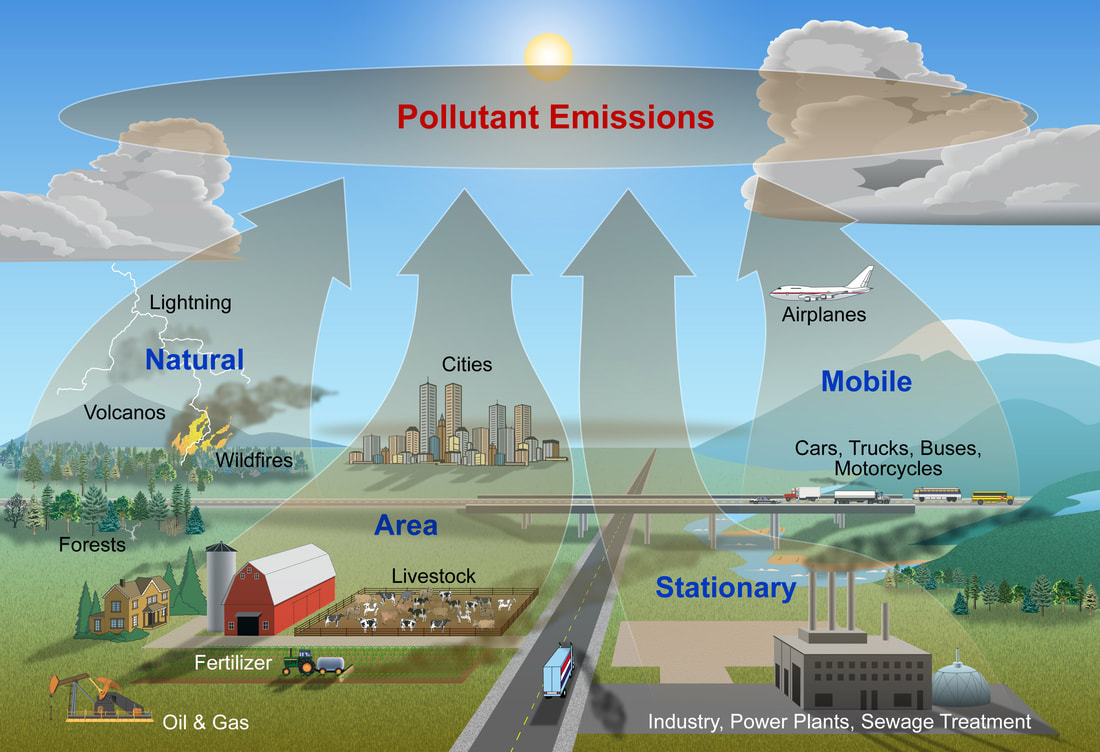
Unveiling the Interplay Between Air Quality and Cardiometabolic Health: A Surprising Connection1/29/2024 In a groundbreaking study, researchers have delved into the intricate relationship between air quality and cardiometabolic health, revealing startling findings that challenge conventional wisdom. Published in Environmental Research, this research sheds light on the impact of air pollutants, even at concentrations below the World Health Organization's (WHO) 2021 guidelines, on various aspects of cardiovascular and metabolic well-being. Key FindingsThe study, conducted over a period of 33 weeks with 82 participants grappling with obesity, examined the associations between air pollutants and cardiometabolic outcomes. Particulate matter emerged as a significant player, demonstrating a strong connection with blood lipids, hormones, and glucose regulation – key markers of cardiometabolic health. Surprisingly, the research also uncovered a potential mitigating factor: diet. The participants' adherence to a Healthy Nordic diet, as measured by the Baltic Sea Diet score, showcased a remarkable ability to modify the impact of air pollution on certain cardiometabolic parameters. Details of the StudyThe study utilized linear mixed-effects models to analyze data gathered during a weight loss and weight loss maintenance intervention. The results revealed 17 significant associations between various air pollutants and 10 distinct cardiometabolic outcomes. The focus was primarily on blood lipids, hormones, and glucose regulation, providing a comprehensive understanding of the multifaceted effects of air pollution. Interestingly, the Baltic Sea Diet score did not appear to mediate the association between air pollution and cardiometabolic outcomes. However, the diet quality factor emerged as a key player in modifying the impact of particulate matter (PM2.5) on total cholesterol. Furthermore, it influenced the associations of nitrogen dioxide (NO) and ozone (O3) with ghrelin, a hormone associated with appetite regulation. ReferencesHealy, Darren R., et al. “Associations of Low Levels of Air Pollution with Cardiometabolic Outcomes and the Role of Diet Quality in Individuals with Obesity.” Environmental Research, vol. 242, 1 Feb. 2024, p. 117637, www.sciencedirect.com/science/article/pii/S0013935123024416, https://doi.org/10.1016/j.envres.2023.117637.
How many hugs have you had today? Neuroeconomist Paul Zak, also known as "Dr. Love," recommends at least eight hugs a day to feel happier and more connected, as well as nurture relationships. As psychotherapist Virginia Satir said: "We need 4 hugs a day for survival. We need 8 hugs a day for maintenance. We need 12 hugs a day for growth." There may very well be a "hug threshold" that allows your body to produce ample amounts of oxytocin, which is released in response to physical touch such as breast-feeding, orgasm, hugs, snuggling, holding hands, partner dance, massage, bodywork, and prayer. The neuropeptide oxytocin, released by your pituitary gland, is a naturally occurring hormone in the body with incredibly powerful, health-giving properties. This "love hormone" is also a key reason why the simple act of hugging is such an incredible way to enhance bonding with others but also boost your physical, and emotional, health. How Hugging Makes You Healthier Hugging increases levels of oxytocin, a neurotransmitter that acts as a hormone. This, in turn, has been observed to have beneficial physiological effects on your cardiovascular health and emotional happiness. One group of researchers observed, for example, a reduction in blood pressure among adults following a brief episode of warm contact with their partner. A 20-second hug, along with 10 minutes of hand-holding, reduces the harmful physical effects of stress, including its impact on your blood pressure and heart rate (Grewen, Anderson, Girdler & Light, 2003). This makes sense, since positive physical contact as hugging and reduces cortisol, increases oxytocin, and lowers systolic blood pressure in stressful situations (Holt-Lunstad, Birmingham & Light, 2008). But researchers suggest there is even more to it than that. The skin contains a network of tiny, egg-shaped rapidly adapting mechanoreceptors called Pacinian corpuscles with a large receptive field that can sense pressure and vibration and which are in contact with the brain through the vagus nerve. The vagus nerve winds its way through the body and provides input and receives sensation from the heart, liver, and digestive tract. (Freberg, 2006). The vagus nerve is also connected to oxytocin receptors. One theory is that stimulation of the vagus triggers an increase in oxytocin, which in turn leads to the cascade of health benefits. A 10-second hug a day can lead to biochemical and physiological reactions in your body that can significantly improve your health. Hugging has been observed to stimulates your nervous system while decreasing feelings of loneliness, combating fear, increasing self-esteem, defusing tension, and showing appreciation. According to researchers, hugging has been observed to (Forsell & Åström, 2012):
The effects of connection There's no doubt that physical touch of all kinds feels good. Whether it is a hug or a handshake, physical touch has a powerful effect on the human psyche resulting in us feeling happy, regardless if you are the toucher or touchee; connection, big or small, results in happiness. Yet, many people are touch-deprived. One poll found that one-third of people receive no hugs on a daily basis while 75 percent said they wanted more hugs. Findings such as these, coupled with the emotional and health benefits of human touch, have led to the emergence of cuddle therapy centers, where people can pay for a lunchtime cuddle. However, some have questioned whether or not physical contact from strangers has the same impact as those from someone you know and trust. While cuddling with a spouse or partner has been shown to boost satisfaction in relationships, some researchers have observed that hugs are only beneficial if trust is involved. Neurophysiologist Jürgen Sandkühler, Head of the Centre for Brain Research at the Medical University of Vienna actually cautioned against worldwide "free hugs" campaigns (where strangers offer hugs to others), saying that this may be perceived as threatening and actually increase emotional burden and stress. However, significant benefits have been found from cuddling with a pet, which shows hugs don't have to only be between humans to be beneficial to your heart and overall health. The Importance of Hugging On average, people spend on hour a month hugging. That doesn't seem like much, but when you consider that the average hug is 3 seconds long, that adds up to be a lot of hugs. And if you had any doubt about the importance of touch, consider that children who lack physical connection have delays in walking, talking, and reading. The act of hugging has a near-immediate impact on health, lowering your heart rate and inducing a calming effect while also leading to a more upbeat mood. Touch is described as a universal language that can communicate distinct emotions with startling accuracy. Researchers observed that touch alone can reveal emotions including anger, fear, disgust, love, gratitude, and sympathy, with accuracy rates of up to 83 percent (Hertenstein, Holmes, McCullough & Keltner, 2009). Hugging is a way to encourage your body to release oxytocin, and the more oxytocin your pituitary gland releases, the better able you are to handle life's stressors. Moreover, oxytocin quite likely plays a role in why pet owners heal more quickly from illness, why couples live longer than singles, and why support groups work for people with addictions and chronic diseases. Oxytocin has also been found to reduce the cravings of drug and alcohol addiction, as well as for sweets. It even has a positive influence on inflammation and wound healing. Even beyond this, regular hugs have the added benefit of:
Do You Need a Hug? Often making a concerted effort to hug the people close to you is one of the best ways to get more hugs in return. This can include your spouse, children, and other family members along with close friends. But even if you're not currently in a life situation conducive to getting daily hugs and producing enough of your own oxytocin on a regular basis, the good news is there are some alternatives you can use to help you deal in a healthy way with your emotional response to stress and anxiety. With the already known and still-to-emerge health and quality of life benefits to be derived from the natural release of oxytocin in your body, your best course of action is to make sure you're cultivating warm, loving, intimate relationships, no matter what stage of life you're in. Additionally, if you have a pet, just a few minutes petting your dog or cat can promote the release of your body's "happiness" hormones, including oxytocin. Since touch anywhere on your body, as well as positive interactions and psychological support, are known to increase oxytocin levels, you might also consider:
References Chillot, R. (2013). The Power of Touch. Retrieved from https://www.psychologytoday.com/us/articles/201303/the-power-touch
Forsell, L., & Åström, J. (2012). Meanings of Hugging: From Greeting Behavior to Touching Implications. Comprehensive Psychology, 1, 02.17.21.CP.1.13. https://doi.org/10.2466/02.17.21.CP.1.13 Freberg, L. (2006). Discovering biological psychology (2nd ed.). Wadsworth: Cengage Learning. Grewen, K., Anderson, B., Girdler, S., & Light, K. (2003). Warm Partner Contact Is Related to Lower Cardiovascular Reactivity. Behavioral Medicine, 29(3), 123-130. https://doi.org/10.1080/08964280309596065 Hertenstein, M., Holmes, R., McCullough, M., & Keltner, D. (2009). The communication of emotion via touch. Emotion, 9(4), 566-573. https://doi.org/10.1037/a0016108 Holt-Lunstad, J., Birmingham, W., & Light, K. (2008). Influence of a “Warm Touch” Support Enhancement Intervention Among Married Couples on Ambulatory Blood Pressure, Oxytocin, Alpha Amylase, and Cortisol. Psychosomatic Medicine, 70(9), 976-985. https://doi.org/10.1097/psy.0b013e318187aef Mercola, J. (2014). How Hugging Makes You Healthier and Happier. Retrieved from https://articles.mercola.com/sites/articles/archive/2014/02/06/hugging.aspx Richardson, J. (2014). 9 Reasons You Need To Be Giving and Receiving Hugs Everyday. Retrieved from http://preventdisease.com/news/14/012314_9-Reasons-Need-Giving-Receiving-Hugs-Everyday.shtml Zhivotovskaya, E. (2012). Oxytocin: Go Out and Touch Someone. Retrieved from https://positivepsychologynews.com/news/emiliya-zhivotovskaya/2012032321636
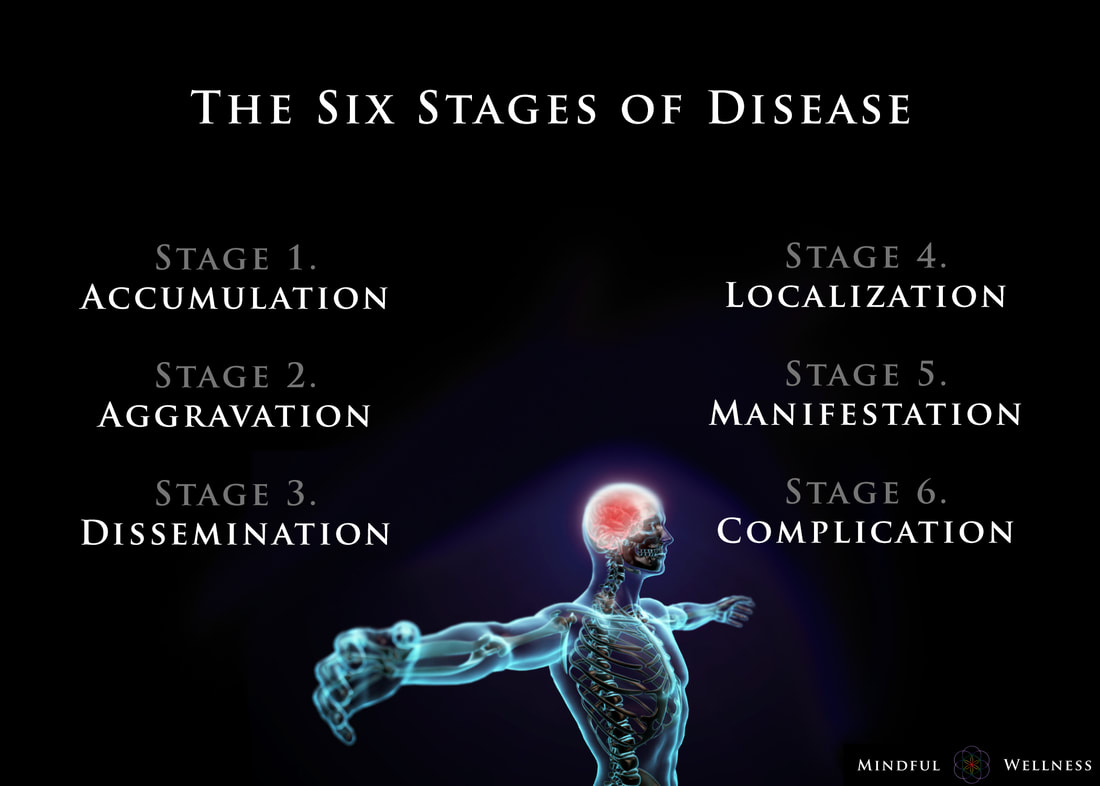
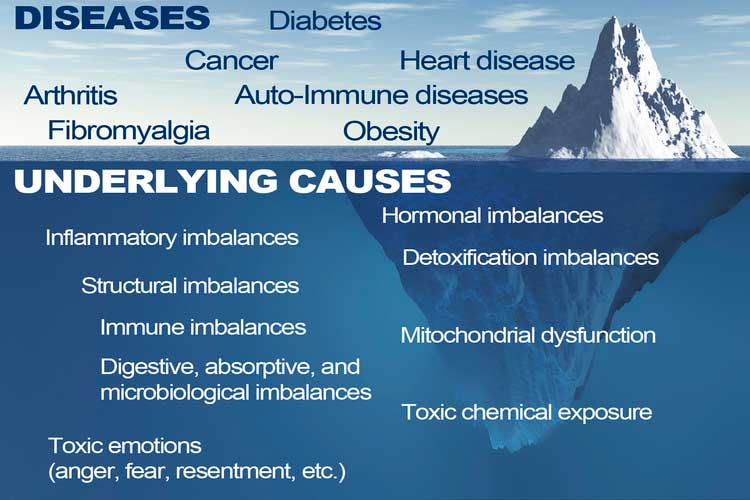
Ayurveda offers insight into the earlier stages and enables those monitoring their health to take care of any small imbalances well before developing any serious illness. The length of the each stage may vary from weeks, to months, even years, depending on the person and the degree of aggravation. The six stages of disease development are:
1. Accumulation The first stage, accumulation, represents imbalance, a build up or collection of something in the body. Being exposed to and acquiring a pathogen via the external environment is an example of accumulation. This stage can also be caused by the internal environment, such as from eating an imbalanced diet leading to excess inflammation or mucous. Accumulation in the body leads to the the next stage, aggravation. 2. Aggravation As the imbalanced elements continue to increase, the symptoms become more aggravated and will begin to be noticed throughout the body. This stage is a sign of continued accumulation. This stage can manifest, as seen in the Kapha state, as loss of appetite, indigestion, nausea, excess saliva, oversleeping, sluggishness; or as seen in the Pitta state, as increased acidity, burning sensations in the abdomen, lowered vitality, or insomnia; or as seen in the Vata state, as pain in the lower abdomen, excess flatulence, and light-headedness. 3. dissemination Once the site of origin is full with excess accumulation and is aggravated, it will begin to overflow into or disseminate throughout the rest of the body using different channels of transportation. Overflow typically begins in the GI tract, then spilling into the circulating plasma and blood, allowing the accumulation to spread systemically, and eventually seeping into the organs and tissues (dhātus). Simultaneously, the symptoms at the site of origin will grow worse. 4. Localization The excess accumulation will then move to wherever a weak site exists in the body. This is where and when diseases begin to develop. This stage is also where genetics matter; the weak spots are determined by genetics - as the saying goes, genetics loads the gun, environment pulls the trigger. This stage can manifest, as seen in the Vata state, as arthritis. In a Pitta state, this can be seen as an ulcer, and in the Kapha state, manifestation may begin in the lungs. At this stage, healing is still regarded as simple. 5. Manifestation This is the first state of the development of illness for which modern Western medicine can detect signs of disease. It is at this stage where diseases progress and become fully developed, showing signs of clinical features. Manifested imbalances are given names at this stage, such as arthrosclerosis, cancer, colitis, etc. It is at this stage where conventional medicine attempts to mask the symptoms by offering pharmaceutical drugs. 6. Complication Complications of the dis-ease begin at this final stage. Often times, conventional medicine attempts to solve the problem by simply removing the affected tissue (e.g., small intenstine, colon, thyroid, etc.) from the body. The symptoms become clear enough so that the elemental cause (i.e., dosha constitution such as Vata, Kapha, Pitta) may be determined. Some medical professionals describe this stage as the chronic phase of development. For example, if one develops inflammation in the manifestation stage, in this stage, complications set in, and the inflammation may grow worse into a chronic problem. Being aware of the stages of the dis-ease process is helpful because one can gain a better understanding in how prevent, and perhaps even reverse, it. To be clear, the information provided here is not claiming to treat, cure or diagnose disease. ReferencesCabral, S. (2018). The 6 Stages of the Disease Process (Ayurvedic Principle). [podcast] The Cabral Concept. Available at: https://itunes.apple.com/us/podcast/cabral-concept-by-stephen/id1071469441?mt=2
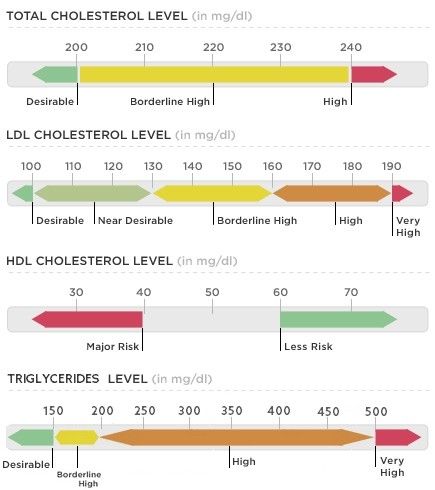
Tirtha, S. (2007). The Āyuveda encyclopedia. Bayville, NY. Ayurveda Holistic Center Press. It's that time: time to test your blood. Most blood tests include a fasting lipid panel to assess one's risk of cardiovascular disease. A lipid panel is a test that measures fats and fatty substances used as a source of energy in the body. Lipids include cholesterol, triglycerides, high-density lipoprotein (HDL) and low-density lipoprotein (LDL). What Are Triglycerides?
Triglycerides are a powerful cardiovascular risk marker. Elevated triglyceride levels are a hallmark of too many carbohydrates in the diet. 60 percent of fructose is shunted toward the liver, where it is converted to triglycerides (which causes heart disease) (Gundry, 2017). In fact, fructose, which is the sugar found in most processed foods (often in the form of high-fructose corn syrup) can only be metabolized by your liver. If you eat a typical Western-style diet, you consume high amounts of it. The overload of fructose ends up damaging your liver in the same way alcohol and other toxins do (Mercola, 2017). What about Cholesterol? Our culture is obsessed with cholesterol levels, to the point that one in four adults in the U.S. take a statin drug to lower cholesterol levels. Nevertheless, elevated cholesterol levels are rarely a risk factor for heart disease, although elevated triglycerides clearly are. Fortunately, elevated triglycerides can easily be corrected and lowered to an ideal level of below 75 with the proper lifestyle interventions. The following tests can give you a far better assessment of your heart disease risk than your total cholesterol alone:
Influence of Triglycerides on Leptin High triglyceride levels (over 100 mg/dL) is known to cause leptin resistance. Leptin is a hormone located in fat cells, and like most hormones, it's function is complex. Leptin is tied to the coordination of our metabolic, hormonal, and behavioral response to starvation. Leptin essentially controls mammalian metabolism. Leptin decides whether to make us hungry and store more fat or burn fat. In other words, when your stomach is full, fat cells release leptin to tell your brain to stop eating. This is why people with low levels of leptin are prone to overeating. One study observed participants with a 20 percent drop in leptin experienced a 24 percent increase in hunger and appetite, influencing their cravings for calorie-dense, high-carbohydrate foods, especially sweets, salty snacks, and starchy foods. The researchers discovered the drop in leptin was caused by sleep deprivation. Leptin is also a pro-inflammatory molecule - it controls the creation of other inflammatory moleciles in your fat tissue throughout your body. This explains why overweight individuals are susceptible to inflammatory problems. Leptin is ranked highly on the body's chain of command, so imbalances tend to spiral downward and wreak havoc on virtually every system of the body beyond those directly controlled by leptin. Leptin, like insulin, is negatively influenced by carbohydrates. The more refined and processed the carbohydrate, the more imbalanced leptin levels become. When the body is overloaded and overwhelmed by substances that cause continuous surges in leptin, leptin receptors begin to turn off and you become leptin resistant. So even though leptin is now elevated, it doesn't work - it won't signal to your brain that you're full so you can stop eating. Not a single drug or supplement can balance leptin levels. But better sleep, as well as better dietary choices will (Perlmutter, 2013). Causes of High Triglycerides
The main culprit Preventing cardiovascular disease involves reducing chronic inflammation in your body, and a proper diet is an absolute cornerstone. Although saturated fat has taken the blame for causing heart disease for the last several decades, the primary culprit in heart disease is sugar consumption. A 2015 study published in the Journal of the American Medical Association concluded that there is " a significant relationship between added sugar consumption and increased risk for cardiovascular mortality." the 15-year study, which included data for 31,000 Americans, found that those who consumed 25 percent or more of their daily calories as added sugars were more than twice as likely to die form heart disease as those who got less than 10 percent of their calories from sugar. On the whole, the odds of dying from heart disease rose in tandem with the percentage of added sugar in the diet regardless of the age, sex, physical activity level, and body mass index (Dhurandhar & Thomas, 2014). A 2014 study came to very similar conclusions. Here, those who consumed the most sugar - about 25 percent of their daily calories - were twice as likely to die form heart disease as those who limited their sugar intake to 7 percent of their total calories (Yang et al., 2013). A 2013 study, published in the Journal of the Academy of Nutrition and Dietetics, looked at the differing effects of high-fat diets versus low-fat diets on blood lipid levels. The study included 32 studies and found that high-fat diets resulted in significantly greater improvements in reductions of total cholesterol, LDL cholesterol, and triglycerides and benificial increases in HDL cholesterol (Schwingshackl et al., 2013). How to Lower Triglycerides
Consider a Detox
The Dangers of StatinsSo, why are we all obsessed with total cholesterol and LDL cholesterol when we know they aren’t the primary culprits for heart attacks? Because a multi-billion dollar drug industry exists behind the number-one best-selling class of drugs on the market: Statins. Of course, the choice to take medications, if referred by your physician is, and should, always be your choice. However, you have the right to be fully informed of the side effects of consuming anything. With this in mind, it is important to be aware of the unintended side effects of taking statins. A study published in Clinical Cardiology concluded that "Statin therapy is associated with decreased myocardial [heart muscle] function," which often leads to heart failure. The study did not address causes, but it's widely known that statins lower your CoQ10 levels by blocking the pathway involved in cholesterol production -- the same pathway by which Q10 is produced. Statins also reduce the blood cholesterol that transports CoQ10 and other fat-soluble antioxidants. The loss of CoQ10 leads to loss of cell energy and increased free radicals which, in turn, can further damage your mitochondrial DNA, effectively setting into motion an evil circle of increasing free radicals and mitochondrial damage (Mercola, 2011). Moreover, for those at risk of heart disease taking statins who are unwilling or unable to bring down their cholesterol and/or triglyceride levels naturally with dietary changes, the potential for liver or muscle damage should be acknowledged. In addition, the potential for brain-related side effects, such as memory loss and confusion, as well as Parkinson’s-like symptoms is of concern. Statin drugs also appeared to increase the risk of stroke and developing diabetes. In 2013, a study of several thousand breast cancer patients reported that long-term use of statins may as much as double a woman's risk of invasive breast cancer. There are 71 diseases that may be associated with these drugs, and this is only the tip of the iceberg. There are actually over 900 studies showing the risks of statin drugs, which include:
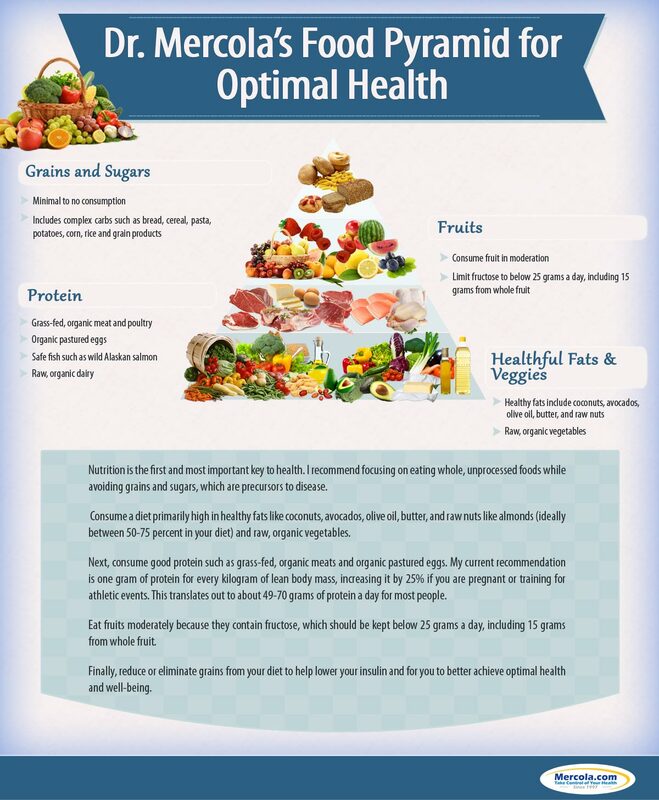
Plant-based diets have been shown to lower cholesterol just as effectively as first-line statin drugs, but without the risks. In fact, the "side effects" of healthy eating tend to be good - less cancer and diabetes risks and protection of the liver and brain (Gregor, 2015). What Should you Eat? ReferencesBaker, A. (2012). What's the real driver of elevated cholesterol? hint: it's not saturated fat! - Nourish Holistic Nutrition. [online] Nourish Holistic Nutrition. Available at: nourishholisticnutrition.com/whats-the-real-driver-of-elevated-cholesterol/ [Accessed 8 Feb. 2019].
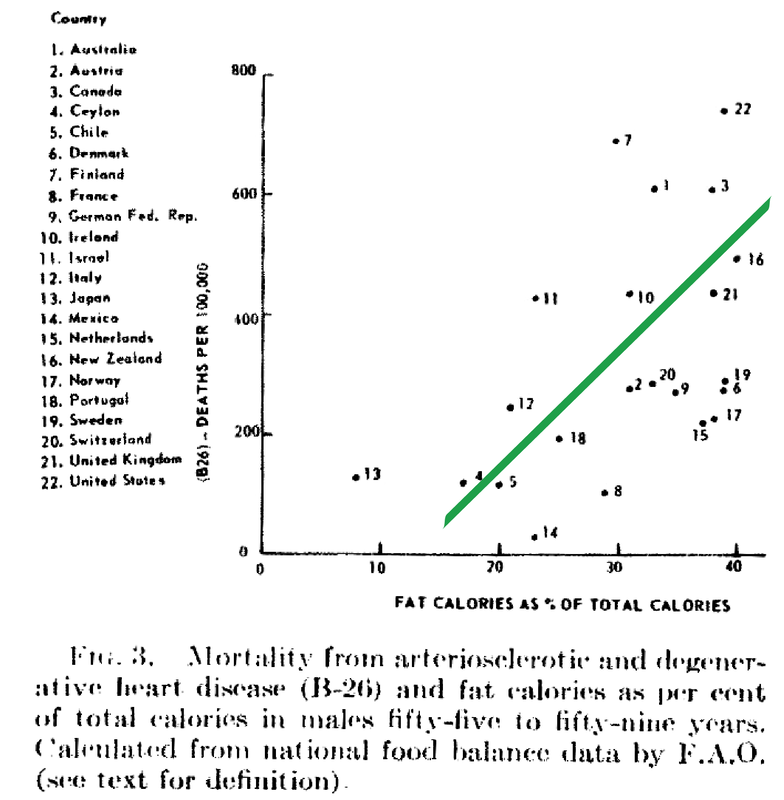
Dhurandhar, N. and Thomas, D. (2015). The Link Between Dietary Sugar Intake and Cardiovascular Disease Mortality. JAMA, 313(9), p.959. https://doi.org/10.1001/jama.2014.18267 [Accessed 8 Feb. 2019]. Gregor, M. (2015) How Not to Die. London: Pan Books Gundry, S. (2017). The Plant Paradox. New York, NY: Harper Wave Hyman, M. (2016). 7 Ways to Optimize Cholesterol. [online] Dr. Mark Hyman. Available at: https://drhyman.com/blog/2016/01/14/7-ways-to-optimize-cholesterol/ [Accessed 8 Feb. 2019]. Mercola, J. (2017). Fat for Fuel. Carlsbad, CA: Hayhouse Inc. Mercola, J. (2011). New Study Shows Using Statins Actually Harms Heart Function. [online] Mercola.com. Available at: https://articles.mercola.com/sites/articles/archive/2011/06/22/new-study-show-using-statins-actually-worsens-your-heart-function.aspx [Accessed 8 Feb. 2019]. Mercola, J. (2015). Conventional Heart Disease Advice May Make Matters Worse. [online] Mercola.com. Available at: https://articles.mercola.com/sites/articles/archive/2015/08/02/heart-disease-risk-factors.aspx [Accessed 8 Feb. 2019]. Perlmutter, D (2013). Grain Brain. New York, NY: Little Brown Ray, K. et al. (2010). Statins and All-Cause Mortality in High-Risk Primary Prevention. Archives of Internal Medicine, 170(12), p.1024. Available at: https://doi.org/10.1001/archinternmed.2010.182 [Accessed 8 Feb. 2019]. Rubinstein, J., Aloka, F. and Abela, G. (2009). Statin Therapy Decreases Myocardial Function as Evaluated Via Strain Imaging. Clinical Cardiology, 32(12), pp.684-689. Available at: https://doi.org/10.1002/clc.20644 [Accessed 8 Feb. 2019]. Schwingshackl, S., et al. (2013). Comparison of Effects of Long-Term Low-Fat vs High-Fat Diets on Blood Lipid Levels in Overweight and Obese Patients: A Systematic Review and Meta-Analysis. Journal of the Academy of Nutrition and Dietetics, 113(12), pp. 1640-61. Available at: https://doi.org/10.1016/j.jand.2013.07.010 [Accessed 8 Feb. 2019]. Wallerwellness.com. (2019). Understanding Triglycerides. [online] Available at: https://www.wallerwellness.com/health-and-aging/understanding-triglycerides [Accessed 8 Feb. 2019]. Williams, J. (2017). How To Lower Dangerously High Triglyceride Levels. [online] Renegade Health. Available at: http://renegadehealth.com/blog/2017/03/31/how-to-lower-dangerously-high-triglycerides-levels [Accessed 8 Feb. 2019]. Yang, Q., et al. (2014). Added Sugar Intake and Cardiovascular Diseases Mortality Among US Adults. JAMA Internal Medicine, 174(4), pp.516-24. Available at: https://doi.org/10.1001/jamainternmed.2013.13563 [Accessed 8 Feb. 2019]. Despite food manufacturers claiming that refined vegetable oils were healthy, Americans experienced an up-rise in heart disease during the early 20th century. Like many new inventions, few questions were initially posited. Unfortunately, an alternate nutrient took the blame due to the research of a single scientist. In 1951, American physiologist and professor Ancel Keys went to Europe in search of the cause of cardiovascular disease. In his quest, he went to observe the eating habits of individuals living Naples, Italy due to reports of a low prevalence of heart disease. During this time, post-war conditions resulted in finite and unusual circumstances in regards to agriculture and infrastructure. Therefore what Keys perceived as a cultural tradition was dubbed the "Mediterranean diet". Keys observed the residents in Naples consumed primarily pasta and plain pizza, with vegetables, olive oil, cheese, fruit for dessert, a moderate amount of wine, and very little meat (except among individuals belonging to a higher socioeconomic status). Through an informal study measuring cholesterol serum levels among Rotary club members (those who could not afford meat, but could afford cheese) conducted by Keys's wife, whom at the time was a medical technologist, Keys deduced that avoiding meat resulted in a lower incidence of heart attacks. Ancel Keys continued on his biased search for proof that a diet high in saturated fat is correlated with a higher risk of cardiovascular disease. He eventually compiled data from six more countries with high rates of heart disease and diets typically high in saturated fat. At first glance, Keys's research seemed logical and compelling. The evidence was based on the premise that individuals in America, who consumed high amounts of saturated fat, died from heart disease at a higher rate than individuals in Japan, who consumed low amounts of saturated fat.
Unfortunately, Keys had gained the interest of people in positions of power. Upon President Eisenhower's heart attack in 1955, Keys proposed his theory to the president's primary care physician, Paul Dudley White. Days following, White began to advise to the public to reduce the consumption of saturated fat and cholesterol in an effort to prevent cardiovascular disease. Through his connections and influence, Keys soon joined the nutrition committee of the American Heart Association (AHA) which, based on Keys's research, released a report in 1961 that advised patients with a high risk of cardiovascular disease to reduce their consumption of saturated fat. (Interestingly enough, the AHA began its rise to prominence in 1948, the same year Proctor & Gamble donated over $1.7 million to the organization - resulting in the AHA indebted to Crisco.) In 1961, Time magazine placed Ancel Keys on the front cover touting him as "the twenthiest century's most influential nutrition expert." By 1970, Keys published the Seven Countries Study, which detailed his original research - this study has now been cited in over a million other scientific publications. While Keys associative observations between saturated fat and cardiovascular disease never proved causation, he had won the battle of public opinion. With the help of Ancel Keys, the American medical community and mainstream media has advised consumers to stop eating the animal products that have been consumed for centuries, replacing them with bread, pasta, margarine, low-fat dairy, and vegetable oil. This was the dietary shift that was codified by the United States government in the late 1970s. References Central Committee for Medical And Community Program of the American Heart Association. (1961). Dietary Fat and Its Relation to Heart Attacks and Strokes. Circulation [online] 23, pp.133-36. Available at: https://circ.ahajournals.org/content/circulationaha/23/1/133.full.pdf [Accessed 26 Jan. 2019]
Keys, A. (1953). Atherosclerosis: A Problem in Newer Public Health. Journal of Mt. Sinai Hospital, [online] 20(2), pp.118-39. Keys, A. (1970). Coronary Heart Disease in Seven Countries. Circulation. 41 (1), pp.1186-95. Keys, A. (1995). Mediterranean Diet and Public Health: Personal Reflections. American Journal of Clinical Nutrition, [online] 61 (6), pp.1321S-1323S. Available at: https://dx.doi.org/10.1093/ajcn/61.6.1321s [Accessed 26 Jan. 2019] Marvin, H. (1964). The 40 Year War on Heart Disease. New York: American Heart Association. Mercola, J. (2017). Fat For Fuel. Carlsbad, California: Hay House. Teichholz, N. (2014). The Big Fat Surprise. New York: Simon & Schuster, pp.32-33. |
The Awareness domain contains research, news, information, observations, and ideas at the level of self in an effort to intellectualize health concepts.
The Lifestyle domain builds off intellectual concepts and offers practical applications.
Taking care of yourself is at the core of the other domains because the others depend on your health and wellness.
Archives
May 2024
Categories
All
|





 RSS Feed
RSS Feed

