|
The human gut is teeming with a diverse array of bacteria collectively known as the gut microbiota. Among its many functions, one of the most vital is colonization resistance—the ability to prevent harmful pathogens from taking up residence in the gut and causing disease. However, understanding which microbiota communities are protective and which allow pathogens to thrive has long been a challenge. In a groundbreaking study led by Spragge et al., researchers shed light on the complex dynamics of gut microbiota and their role in colonization resistance against two significant bacterial pathogens: Klebsiella pneumoniae and Salmonella enterica serovar Typhimurium. Their findings, published in Science, unveil the critical importance of microbiome diversity in safeguarding against pathogenic invasion. Traditionally, it was believed that certain individual bacterial species might confer colonization resistance. However, Spragge et al. discovered that the true protective power lies in the collective diversity of the microbiota. They conducted meticulous experiments both in vitro and in gnotobiotic mice (mice that have been raised in a controlled environment where the microbial composition of their gut is precisely known and controlled), evaluating the ability of single bacterial species and increasingly diverse microbiota communities to resist pathogen colonization. Surprisingly, the researchers found that single species alone provided limited protection against the pathogens. It was only when these species were combined into diverse communities consisting of up to 50 different species that colonization resistance was significantly enhanced. This underscores the importance of ecological diversity in promoting gut health. Moreover, the study identified certain key species within these diverse communities that played a pivotal role in bolstering colonization resistance, even though they offered little protection on their own. These key species acted by consuming nutrients required by the pathogens, thereby depriving them of essential resources for growth and establishment in the host. Importantly, Spragge et al. demonstrated that microbiome diversity not only increases the probability of protection against pathogens but also enhances the overlap in nutrient utilization profiles between the microbiota community and the pathogen. This nutrient blocking mechanism serves as a potent defense strategy against pathogenic invasion. The implications of these findings are profound. They provide compelling evidence for the health benefits of a diverse gut microbiome and offer insights into the rational design of pathogen-resistant microbiota communities. By harnessing the protective power of microbiome diversity, we may pave the way for innovative strategies to combat infectious diseases and promote overall gut health. In conclusion, Spragge et al.'s study unveils the intricate interplay between microbiome diversity and colonization resistance, highlighting the collective strength of diverse bacterial communities in defending against pathogenic threats. This research not only expands our understanding of gut microbiota dynamics but also holds promise for the development of novel therapeutics aimed at fortifying the body's natural defenses against infections. referencesSpragge, Frances, et al. “Microbiome Diversity Protects against Pathogens by Nutrient Blocking.” Science, vol. 382, no. 6676, 15 Dec. 2023, https://doi.org/10.1126/science.adj3502.
0 Comments
In our modern world, where convenience often comes at a cost, the prevalence of obesogens – chemicals that disrupt the body's normal metabolism and contribute to weight gain – has emerged as a growing concern. From everyday products to industrial pollutants, obesogens permeate our environment, exerting subtle yet profound effects on our health and well-being. Commonly encountered obesogensAmong the many obesogens encountered in daily life, several stand out for their widespread use and potential health impacts:
Mechanisms of ActionObesogens exert their effects through various mechanisms, including:
Disruption of Metabolism via MitochondriaObesogens, through their pervasive presence in our environment, exert insidious effects on metabolic function, including the intricate workings of mitochondria – the cellular powerhouses responsible for energy production. By disrupting mitochondrial function, obesogens can contribute to metabolic dysregulation and, ultimately, weight gain. Mitochondria play a central role in energy metabolism, converting nutrients into adenosine triphosphate (ATP), the primary source of cellular energy. However, exposure to obesogens can impair mitochondrial function through various mechanisms, including:
The disruption of mitochondrial function by obesogens can have profound implications for metabolic health and contribute to obesity through several pathways:
causative relationship with health conditionsThe impact of obesogens on human health extends beyond weight gain, with associations documented with various health conditions, including:
Additionally, obesogens are highly related to the following health conditions and physiologic imbalances:
Unraveling the Role of Dysfunctional Adipose TissueRelatively little is known about the extent to which obesogen exposure programs dysfunctional adipose tissue that may store but not mobilize fat. However, emerging evidence suggests that obesogens may contribute to adipocyte dysfunction, leading to altered fat storage and metabolism. One potential underlying factor is suboptimal liver detoxification pathways due to inadequate micronutrient cofactors. Inadequate levels of essential micronutrients, such as vitamins and minerals, can impair liver detoxification pathways responsible for metabolizing and eliminating obesogens from the body. As a result, obesogens may accumulate in adipose tissue, disrupting metabolic function and contributing to weight gain. Additionally, micronutrient deficiencies can compromise mitochondrial function, further exacerbating metabolic dysfunction and obesity risk. A Layman's Overview of Obesogens: Redefining the Weight Loss ParadigmIn the quest for weight loss, many of us often find ourselves fixating on calorie counting, fad diets, or intense workout regimens. However, what if I told you that the key to achieving a healthy weight isn't solely about shedding pounds but rather fixing your metabolism? Enter obesogens – a lesser-known yet influential factor in the obesity epidemic. As mentioned, obesogens are chemicals found in our environment, ranging from pesticides and plastics to food additives and personal care products. These substances have the uncanny ability to disrupt our body's natural weight-regulating mechanisms, leading to weight gain and metabolic dysfunction. Instead of solely blaming calories in versus calories out, it's essential to recognize the role obesogens play in shaping our metabolism. The Better Question: Fixing MetabolismRather than constantly asking ourselves, "How do I lose weight?" a more pertinent question would be: "How do I fix my metabolism?" Fixing metabolism involves addressing the root cause of weight gain – obesogen exposure and metabolic disruption. By eliminating or reducing our exposure to obesogens and ensuring our bodies receive essential micronutrients, we can optimize metabolic function and promote overall health. The Two-Fold SolutionTo achieve optimal health and maintain a healthy weight, a two-fold approach is necessary: 1. Reduce Toxin Exposure: Minimize exposure to obesogens by making conscious choices in our daily lives. This includes opting for organic produce, using natural cleaning and personal care products, and avoiding plastic containers and food packaging whenever possible. By participating in a structured evidenced-based detoxification program, we in turn lower our toxic burden, and we can mitigate the adverse effects of obesogens on our metabolism. 2. Consume Micronutrients: Vital micronutrients, such as vitamins and minerals, serve as essential cofactors in metabolic pathways. Ensuring adequate intake of these micronutrients through a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support optimal metabolic function. Additionally, supplementation may be necessary to address any deficiencies and promote metabolic health. The conventional approach to weight loss often overlooks the critical role obesogens play in metabolic dysfunction. Instead of solely focusing on calorie restriction or intense exercise, shifting our focus to fixing metabolism through toxin reduction and micronutrient consumption offers a more holistic and sustainable solution to achieving optimal health. By addressing the underlying factors contributing to metabolic disruption, we can pave the way for lasting weight management and overall well-being. the harm of environmental toxinsThe disruption of metabolic and mitochondrial function by obesogens represents a significant public health concern, with implications for obesity and metabolic disease. By understanding the mechanisms through which obesogens impair mitochondrial function and contribute to weight gain, researchers can develop targeted interventions to mitigate their adverse effects on metabolic health. Moreover, addressing underlying factors such as suboptimal liver detoxification pathways and micronutrient deficiencies is essential in combating the detrimental impact of obesogens on metabolic function and obesity prevalence. The pervasive presence of obesogens in our environment underscores the need for greater awareness and regulation of these harmful chemicals. By minimizing exposure to obesogens and advocating for safer alternatives, we can mitigate their adverse effects on human health and combat the rising tide of obesity and metabolic disease. As we navigate the complexities of modern living, vigilance and informed consumer choices are essential in safeguarding our health and well-being against the hidden threats of obesogens. Taking Action: The Integral Wellness ProgramFor those seeking tangible solutions to combat the effects of obesogens and improve their overall well-being, the Integral Wellness Program offers a comprehensive approach to optimizing health and vitality. This flagship service provides personalized guidance and support in key areas of movement, nutrition, and lifestyle to directly enhance quality of life. Online/In-Person Guidance One of the standout features of the Integral Wellness Program is its flexibility, offering both online and in-person consultations tailored to individual preferences and needs. Whether you prefer the convenience of virtual sessions or the hands-on approach of in-person coaching, our team of experienced wellness professionals is dedicated to supporting you every step of the way. Movement, Nutrition, and Lifestyle The Integral Wellness Program takes a holistic approach to health, addressing modifiable factors and behaviors in three core areas:
Augmenting the Health Process By participating in the Integral Wellness Program, you'll not only gain valuable knowledge and skills to navigate the challenges of modern living but also receive ongoing support and accountability to stay on track towards your health goals. Through targeted interventions aimed at eliminating obesogen exposure and promoting healthy behaviors, you can unlock your body's full potential and thrive in all aspects of life. The Integral Wellness Program offers a transformative journey towards optimal health and vitality. By prioritizing movement, nutrition, and lifestyle modifications, participants can take proactive steps to combat the effects of obesogens and reclaim control over their well-being. With the guidance and support of our dedicated wellness professionals, you'll embark on a path of self-discovery, empowerment, and lasting transformation. referencesRecent breakthrough studies have shone a light on the intriguing link between our microbiome – the diverse community of microorganisms residing in our gut and mouth – and the secret to a longer, healthier life. Scientists have long suspected that our genes, environment, and internal factors like the microbiome play a role in determining how long we live, but the specifics remained elusive. Now, thanks to cutting-edge research, we're getting closer to unraveling the mysteries of longevity. In this groundbreaking exploration, scientists employed a sophisticated approach called Mendelian randomization (MR) to delve into the intricate relationships between the human microbiome and longevity. By analyzing genetic data from large cohorts, they uncovered some compelling associations that shed light on the microbial players in the quest for a longer life. The Gut Chronicles: Microbial Superstars and CulpritsThe gut microbiome, a bustling metropolis of bacteria, has been a focal point in the quest for longevity. The study identified certain gut microbes as potential champions in the battle against aging. Microbial heroes like Coriobacteriaceae, Oxalobacter, and the probiotic Lactobacillus amylovorus were found to be positively linked to increased odds of longevity. On the flip side, a few gut microbes emerged as potential antagonists, with names like Fusobacterium nucleatum, Coprococcus, Streptococcus, Lactobacillus, and Neisseria negatively associated with longevity. These microbial foes might have a role in determining how gracefully we age. Oral Health: More Than Just a Pretty SmileThe study didn't stop at the gut; it extended its gaze to the oral microbiome, a less-explored but equally important realm. The findings suggested a fascinating connection between the oral microbiome and longevity. Specific oral bacteria were identified as potential influencers in the longevity game. Interestingly, the research hinted at a lower gut microbial diversity among centenarians (diversity appears to lower with age), but no significant difference in their oral microbiota. This finding underscores the importance of tracking the movements of these beneficial microbes across different parts of the body for a longer and healthier life. Decoding the Genetic Blueprint for LongevityThe study leveraged Mendelian randomization to unravel the causality between the microbiome and longevity. This approach, using genetic variants as tools, allowed scientists to explore the potential causal links between specific microbial features and the length of our lives. The bidirectional analyses provided a wealth of information, not only pinpointing specific microbes associated with longevity but also revealing the microbial preferences of genetically longevous individuals. For instance, genetic predisposition to longevity correlated with a higher abundance of Prevotella and a lower abundance of Bacteroides, suggesting a potential link between dietary choices and a longer life. Microbes and Diseases: Unraveling the We The study didn't just stop at longevity; it ventured into the realm of diseases. Certain microbes associated with longevity were found to have correlations with specific diseases. For example, Coriobacteriaceae, linked to longevity, was significantly reduced in patients with heart failure, suggesting a potential protective role against cardiovascular diseases. This "microbiota—disease—longevity" axis provides a nuanced understanding of how our microbial companions might influence not only our lifespan but also our susceptibility to various health conditions. What's Next in the Quest for a Longer LifeWhile the study opens exciting new avenues, there are some limitations to consider. The identified causalities didn't all reach statistical significance due to the vast number of microbial features tested. However, the robustness of the findings was supported by the replication of several identified causal links in independent datasets. Moving forward, researchers aim to collect more comprehensive individual-level data, including microbiome profiles, genetics, socio-economic factors, behaviors, and environmental influences. This holistic approach will help tease apart the individual contributions of these factors to longevity. In conclusion, this pioneering study, using Mendelian randomization, has provided us with a roadmap to explore the intricate connections between our microbiome and the quest for a longer, healthier life. As we unlock the secrets hidden in our genes and microbes, we inch closer to personalized approaches for healthy aging and interventions that could extend our time on this planet. referencesLiu, Xiaomin, et al. “Mendelian Randomization Analyses Reveal Causal Relationships between the Human Microbiome and Longevity.” Scientific Reports, vol. 13, no. 1, 29 Mar. 2023, p. 5127, www.nature.com/articles/s41598-023-31115-8, https://doi.org/10.1038/s41598-023-31115-8.
In an update to its 2007 scientific statement, the American Heart Association (AHA) emphasizes the significant and multifaceted benefits of resistance training (RT) on cardiovascular health. Contrary to the misconception that RT solely enhances muscle mass and strength, the statement highlights the favorable physiological and clinical effects of this form of exercise on cardiovascular disease (CVD) and associated risk factors. The scientific statement aims to provide comprehensive insights into the impact of RT, either alone or in combination with aerobic training, on traditional and nontraditional CVD risk factors. More is not always betterEpidemiological evidence suggests that RT is associated with a lower risk of all-cause mortality and CVD morbidity and mortality. Adults who participate in RT have ≈15% lower risk of all-cause mortality and 17% lower risk of CVD, compared with adults who report no RT. Approximately 30 to 60 minutes per week of RT is associated with the maximum risk reduction for all-cause mortality and incident CVD. Notice this "U" shape in the curve when examining the relationship between RT and morbidity and mortality. This curve suggests that some RT is clearly beneficial, but has the volume of RT increases past a certain point the benefits drop and it becomes harmful. The concept of a "biphasic response" is fundamental to understanding hormesis. It describes the characteristic dose-response relationship observed in hormetic processes, where a substance or stressor elicits opposite effects at low and high doses. The response can be visualized as a U-shaped or J-shaped curve, illustrating the beneficial effects at low doses and potential harm at higher doses. Benefits of RT on Traditional CVD Risk FactorsThe AHA's scientific statement underscores the positive influence of RT on traditional CVD risk factors, including blood pressure (BP), glycemia, lipid profiles, and body composition. Numerous studies indicate that engaging in RT is associated with reduced resting BP, improved glycemic control, and favorable alterations in lipid profiles, contributing to a lower risk of all-cause mortality and CVD morbidity. Despite recommendations suggesting 2 days per week of RT, only 28% of U.S. adults adhere to this guideline, highlighting the need for increased awareness and promotion. RT and resting blood pressureRT has demonstrated the ability to reduce resting BP across diverse populations, with notable benefits observed in individuals with prehypertension and hypertension. The mechanisms behind these benefits include enhancements in endothelial function, vasodilatory capacity, and vascular conductance. The reductions in BP achieved through RT are comparable to those achieved with antihypertensive medications. RT and GlycemiaRT shows promise in improving glycemia and insulin resistance, leading to a lower incidence of diabetes. The evidence suggests a nonlinear dose-response association, with up to 60 minutes per week of RT associated with the maximum risk reduction for diabetes. RT and Lipid ProfilesWhile the effect on lipid profiles is modest, RT results in favorable changes in high-density lipoprotein cholesterol, total cholesterol, and triglycerides. These improvements are more pronounced in older adults and those with elevated cardiometabolic risk. Rt, Body composition, and weightRT positively influences body composition by increasing lean body mass and reducing body fat percentage. It is particularly effective in overweight or obese individuals, contributing to increased metabolic rate and mitigating weight gain over time. Benefits of RT on Nontraditional CVD Risk FactorsIn addition to traditional risk factors, the scientific statement highlights the potential mechanisms by which RT positively affects nontraditional CVD risk factors. These include increased cardiorespiratory fitness, improved endothelial function, and potential benefits for sleep quality, psychological health, and well-being. The AHA's updated scientific statement reinforces the pivotal role of resistance training in cardiovascular health, providing a comprehensive overview of its impact on both traditional and nontraditional risk factors. As the evidence supporting RT's benefits continues to grow, the statement serves as a valuable resource for clinicians and public health professionals, offering practical strategies for promoting and prescribing resistance training to enhance cardiovascular health in diverse populations. ReferencesPaluch, Amanda E, et al. “Resistance Exercise Training in Individuals with and without Cardiovascular Disease: 2023 Update: A Scientific Statement from the American Heart Association.” Circulation, 7 Dec. 2023, https://doi.org/10.1161/cir.0000000000001189. Accessed 11 Dec. 2023.
Momma H, Kawakami R, Honda T, Sawada SS. Muscle-strengthening activities are associated with lower risk and mortality in major non-communicable diseases: a systematic review and meta-analysis of cohort studies. Br J Sports Med. 2022 Jul;56(13):755-763. doi: 10.1136/bjsports-2021-105061. Epub 2022 Feb 28. PMID: 35228201; PMCID: PMC9209691. Nasal Breathing: A Breath of Fresh Air for Cardiovascular Wellness – Insights from New Research2/4/2024 The leading cause of death in the United States is cardiovascular disease, and the risk of cardiovascular issues can be predicted by factors such as blood pressure, heart rate variability, blood pressure variability, and cardiac vagal baroreflex sensitivity. The interplay between the cardiovascular and respiratory systems is highlighted, with a particular emphasis on how respiration affects key prognostic cardiovascular variables. This study explores the impact of nasal breathing compared to oral breathing on cardiovascular health in young adults. Nasal breathing is associated with humidification, warming, and filtration of inhaled air, potentially leading to bronchodilation and improved breathing efficiency. While past research has shown nasal breathing to have positive effects on resting metabolic demands, its influence on cardiovascular markers is not well-understood. The primary hypothesis is that nasal breathing, as opposed to oral breathing, will result in decreased blood pressure, improved heart rate variability, reduced blood pressure variability, and increased cardiac vagal baroreflex sensitivity at rest. The study aims to contribute to the understanding of how breathing patterns influence prognostic cardiovascular variables, aligning with the broader interest in the impact of breathing pace and training on cardiovascular health. The secondary hypothesis focuses on the effects of nasal breathing during submaximal exercise. The expectation is that nasal breathing, by attenuating the ventilatory response and metabolic demands, will lead to reduced blood pressure responses, improved heart rate variability, and decreased blood pressure variability during exercise. This aspect is particularly relevant due to the association between elevated exercise blood pressure and the risk of developing hypertension and cardiovascular disease. FindingsThe study findings are summarized, focusing on the impact of nasal vs. oral breathing on physiological and subjective variables at rest and during exercise. At rest, nasal breathing is associated with lower mean and diastolic blood pressure, improved heart rate variability metrics, reduced LF/HF ratio, and lower ratings of perceived exertion (RPE) and breathlessness (RPB). However, it increased systolic blood pressure average real variability. During submaximal exercise, differences between nasal and oral breathing were observed for RPB, suggesting a modest effect on reducing breathlessness during acute exercise. The discussion delves into the potential clinical significance of these findings, particularly the reduction in diastolic blood pressure during nasal breathing at rest. The study suggests a greater parasympathetic to sympathetic dominance during nasal breathing, indicated by changes in frequency-domain metrics of heart rate variability. Although nasal breathing did not significantly affect beat-to-beat blood pressure variability, there is speculation about potential connections between respiratory variables and blood pressure changes, emphasizing the need for further investigation. The study notes that the impact of nasal breathing on cardiovascular variables may have implications for various populations and suggests avenues for future research, including examining nasal breathing's effects on blood pressure over longer durations, both at rest and during activities like exercise. The discussion also touches on the potential benefits of interventions like mouth-taping overnight, emphasizing the importance of considering nasal breathing in the context of broader health outcomes. In summary, the study highlights the potential benefits of nasal breathing, with improvements in various cardiovascular and subjective measures at rest. While the effects during exercise are more modest, the findings contribute to understanding the nuanced relationship between respiratory patterns and cardiovascular health. referencesWatso, Joseph C., et al. “Acute Nasal Breathing Lowers Diastolic Blood Pressure and Increases Parasympathetic Contributions to Heart Rate Variability in Young Adults.” American Journal of Physiology. Regulatory, Integrative and Comparative Physiology, vol. 325, no. 6, 1 Dec. 2023, pp. R797–R808, pubmed.ncbi.nlm.nih.gov/37867476/, https://doi.org/10.1152/ajpregu.00148.2023.
Navigating Hormesis: Embracing the Balance Between Stress and Strength for Optimal Health12/21/2023 In the intricate dance of biological responses to stress, hormesis emerges as a captivating phenomenon, challenging conventional notions of dose-response relationships. This blog post delves into the fascinating world of hormesis, where the subtle interplay between stressors and adaptive responses shapes our understanding of health and resilience. The Hormetic Curve: Unveiling the U-Shaped StoryExplore the dynamics of hormesis through the lens of a U-shaped or J-shaped curve, where low doses of stressors trigger beneficial responses while high doses lead to toxicity. Understand how this nonlinear relationship challenges traditional toxicological paradigms. Small Doses, Big Impact: Hormetic Responses UnveiledDelve into real-world examples of hormetic responses, from the beneficial effects of low-dose radiation to the adaptive mechanisms activated by moderate exercise. Learn how these responses stimulate resilience, adaptation, and overall well-being. Hormesis in Toxicology: Redefining Risk AssessmentUnravel the complexities of hormesis in toxicology, where the concept challenges established risk assessment practices. Discover how hormesis introduces a nuanced understanding of dose-dependent effects, prompting a reevaluation of regulatory frameworks. Hormesis and Adaptive Learning: "What Doesn't Kill You Makes You Stronger"Connect the dots between hormesis and the age-old adage, "What doesn't kill you makes you stronger." Explore how the hormetic principle aligns with the idea that controlled exposure to stressors can lead to adaptive learning, fostering strength and resilience. Balancing Act: The Importance of ModerationEmphasize the crucial role of balance and moderation in hormesis. Uncover the delicate equilibrium required for stressors to act as catalysts for positive adaptation without tipping into harmful territory. From Sirtuins to Telomeres: Hormesis at the Cellular LevelJourney into the cellular realm and discover how hormesis influences sirtuins, telomeres, and other cellular processes. Explore the implications for cellular repair, mitochondrial function, and the potential impact on longevity. Practical Insights: Applying Hormesis in Everyday LifeGain practical insights into how hormesis can be applied in daily life. Explore lifestyle choices, dietary considerations, and stress management techniques that harness the power of hormetic responses for enhanced well-being. Embark on a journey of discovery as we unravel the layers of hormesis, revealing its impact on biology, health, and our quest for a balanced and resilient life. Embrace the science behind stress and strength, and learn how hormesis invites us to rethink our approach to well-being.
The documentary "War on Ivermectin" explores the contentious landscape surrounding the drug Ivermectin during the COVID-19 pandemic. It delves into the controversy surrounding the use of Ivermectin as a potential treatment for COVID-19 and the challenges it has faced from regulatory bodies and mainstream medical establishments.
The documentary presents perspectives from advocates of Ivermectin, who argue for its efficacy and safety in treating COVID-19. It may shed light on the resistance faced by proponents of Ivermectin, exploring factors such as media portrayal, regulatory decisions, and the broader implications for the treatment landscape. Additionally, the documentary might feature interviews with medical professionals, researchers, and individuals who have been affected by the debate over Ivermectin. It aims to provide a comprehensive overview of the complex and polarized discussions surrounding the drug in the context of the global response to the pandemic. Magnesium deficiency is often misdiagnosed because it does not show up in blood tests - only 1% of the body's magnesium is stored in the blood99% of magnesium is stored inside of cells, of that, 95% is stored in mitochondria. So if your blood magnesium levels are low, your incredibly deficient in magnesium.
Consider Dr. Norman Shealy's statements, "Every known illness is associated with a magnesium deficiency" and that, "magnesium is the most critical mineral required for electrical stability of every cell in the body. A magnesium deficiency may be responsible for more diseases than any other nutrient." The truth he states exposes a gapping hole in modern medicine that explains a good deal about iatrogenic death (death caused by "medicine") and disease. Because magnesium deficiency is largely overlooked, millions of Americans suffer needlessly or are having their symptoms treated with expensive drugs when they could be cured with magnesium supplementation. One has to recognize the signs of magnesium thirst or hunger on their own since allopathic medicine is lost in this regard. It is really something much more subtle then hunger or thirst but it is comparable. In a world though where doctors and patients alike do not even pay attention to thirst and important issues of hydration, it is not hopeful that we will find many recognizing and paying attention to magnesium thirst and hunger, which is a dramatic way of expressing the concept of magnesium deficiency. Few people are aware of the enormous role magnesium plays in our bodies. Magnesium is by far the most important mineral in the body. After oxygen, water, and basic food, magnesium may be the most important element needed by our bodies; vitally important, yet hardly known. It is more important than calcium, potassium or sodium and regulates all three of them. Millions suffer daily from magnesium deficiency without even knowing it. In fact, there happens to be a relationship between what we perceive as thirst and deficiencies in electrolytes. I remember a person asking, "Why am I dehydrated and thirsty when I drink so much water?" Thirst can mean not only lack of water but it can also mean that one is not getting enough nutrients and electrolytes. Magnesium, Potassium, Bicarbonate, Chloride and Sodium are some principle examples and that is one of the reasons magnesium chloride is so useful. You know all those years, when doctors used to tell their patients 'its all in your heads,' were years the medical profession was showing its ignorance. It is a torment to be magnesium deficient on one level or another. Even if it's for the enthusiastic sport person whose athletic performance is down, magnesium deficiency will disturb sleep and background stress levels and a host of other things that reflect on the quality of life. Doctors have not been using the appropriate test for magnesium - their serum blood tests just distort their perceptions. Magnesium has been off their radar screens through the decades that magnesium deficiencies have snowballed. Symptoms of Magnesium DeficiencyThe first symptoms of deficiency can be subtle - as most magnesium is stored in the tissues, leg cramps, foot pain, or muscle 'twitches' can be the first sign. Other early signs of deficiency include loss of appetite, nausea, vomiting, fatigue, and weakness. As magnesium deficiency worsens, numbness, tingling, seizures, personality changes, abnormal heart rhythms, and coronary spasms can occur. A full outline of magnesium deficiency was beautifully presented in a recent article by Dr. Sidney Baker. "Magnesium deficiency can affect virtually every organ system of the body. With regard to skeletal muscle, one may experience twitches, cramps, muscle tension, muscle soreness, including back aches, neck pain, tension headaches and jaw joint (or TMJ) dysfunction. Also, one may experience chest tightness or a peculiar sensation that he can't take a deep breath. Sometimes a person may sigh a lot." "Symptoms involving impaired contraction of smooth muscles include constipation; urinary spasms; menstrual cramps; difficulty swallowing or a lump in the throat-especially provoked by eating sugar; photophobia, especially difficulty adjusting to oncoming bright headlights in the absence of eye disease; and loud noise sensitivity from stapedius muscle tension in the ear." "Other symptoms and signs of magnesium deficiency and discuss laboratory testing for this common condition. Continuing with the symptoms of magnesium deficiency, the central nervous system is markedly affected. Symptoms include insomnia, anxiety, hyperactivity and restlessness with constant movement, panic attacks, agoraphobia, and premenstrual irritability. Magnesium deficiency symptoms involving the peripheral nervous system include numbness, tingling, and other abnormal sensations, such as zips, zaps and vibratory sensations." "Symptoms or signs of the cardiovascular system include palpitations, heart arrhythmias, and angina due to spasms of the coronary arteries, high blood pressure and mitral valve prolapse. Be aware that not all of the symptoms need to be present to presume magnesium deficiency; but, many of them often occur together. For example, people with mitral valve prolapse frequently have palpitations, anxiety, panic attacks and premenstrual symptoms. People with magnesium deficiency often seem to be "uptight." Other general symptoms include a salt craving, both carbohydrate craving and carbohydrate intolerance, especially of chocolate, and breast tenderness." Magnesium is needed by every cell in the body including those of the brain. It is one of the most important minerals when considering supplementation because of its vital role in hundreds of enzyme systems and functions related to reactions in cell metabolism, as well as being essential for the synthesis of proteins, for the utilization of fats and carbohydrates. Magnesium is needed not only for the production of specific detoxification enzymes but is also important for energy production related to cell detoxification. A magnesium deficiency can affect virtually every system of the body. One of the principle reason doctors write millions of prescriptions for tranquilizers each year is the nervousness, irritability, and jitters largely brought on by inadequate diets lacking magnesium. Persons only slightly deficient in magnesium become irritable, highly-strung, and sensitive to noise, hyper-excitable, apprehensive and belligerent. If the deficiency is more severe or prolonged, they may develop twitching, tremors, irregular pulse, insomnia, muscle weakness, jerkiness and leg and foot cramps. If magnesium is severely deficient, the brain is particularly affected. Clouded thinking, confusion, disorientation, marked depression and even the terrifying hallucinations of delirium tremens are largely brought on by a lack of this nutrient and remedied when magnesium is given. Because large amounts of calcium are lost in the urine when magnesium is under supplied, the lack of this nutrient indirectly becomes responsible for much rampant tooth decay, poor bone development, osteoporosis and slow healing of broken bones and fractures. With vitamin B6 (pyridoxine), magnesium helps to reduce and dissolve calcium phosphate kidney stones. Magnesium deficiency may be a common factor associated with insulin resistance. Symptoms of MS that are also symptoms of magnesium deficiency include muscle spasms, weakness, twitching, muscle atrophy, an inability to control the bladder, nystagmus (rapid eye movements), hearing loss, and osteoporosis. People with MS have higher rates of epilepsy than controls. Epilepsy has also been linked to magnesium deficiencies.[1] Gastrointestinal UPSET with MagnesiumSome individuals report gastrointestinal upset with magnesium, likely due to the citrate (helpful for endothelial and metabolic function), which typically has a high bioavailability. The nature of magnesium salts is the resulting osmotic effect - the potential laxative effect is due to magnesium (salts) remaining in the intestines causing water to be drawn toward the salts for equilibrium, leading to gastrointestinal distress. While it is often recommended to take magnesium with food, some potential methods to offset the laxative effect would be to consume it fasted, augmenting absorption, and/or improve hydration by consuming more water, ideally prepared by reverse osmosis. Another way you can avoid that laxative effect is stop the consumption of magnesium citrate and taking molecular hydrogen, which contains pure ionic metallic magnesium. early warning symptoms suggestive of magnesium insufficiency
Possible manifestations of magnesium deficiency includeSevere magnesium deficiency can result in low levels of calcium in the blood (hypocalcemia). Magnesium deficiency is also associated with low levels of potassium in the blood (hypokalemia). Magnesium levels drop at night, leading to poor REM (Rapid Eye Movement) sleep cycles and unrefreshed sleep. Headaches, blurred vision, mouth ulcers, fatigue and anxiety are also early signs of depletion. We hear all the time about how heart disease is the number one health crisis in the country, about how high blood pressure is the "silent killer", and about how ever increasing numbers of our citizens are having their lives and the lives of their families destroyed by diabetes, Alzheimer's disease, and a host of other chronic diseases. Signs of severe magnesium deficiency include
Magnesium deficiency is synonymous with diabetes and is at the root of many if not all cardiovascular problems. Magnesium deficiency is a predictor of diabetes and heart disease both; diabetics both need more magnesium and lose more magnesium than most people. In two new studies, in both men and women, those who consumed the most magnesium in their diet were least likely to develop type 2 diabetes, according to a report in the January 2006 issue of the journal Diabetes Care. Until now, very few large studies have directly examined the long-term effects of dietary magnesium on diabetes. Dr. Simin Liu of the Harvard Medical School and School of Public Health in Boston says, "Our studies provided some direct evidence that greater intake of dietary magnesium may have a long-term protective effect on lowering risk," said Liu, who was involved in both studies. The thirst of diabetes is part of the body's response to excessive urination. The excessive urination is the body's attempt to get rid of the extra glucose in the blood. This excessive urination causes the increased thirst. But we have to look at what is causing this level of disharmony. We have to probe deeper into layers of cause. The body needs to dump glucose because of increasing insulin resistance and that resistance is being fueled directly by magnesium deficiency, which makes toxic insults more damaging to the tissues at the same time. When diabetics get too high blood sugars, the body creates "ketones" as a by-product of breaking down fats. These ketones cause blood acidity which causes "acidosis" of the blood, leading to Diabetic Ketoacidosis (DKA), This is a very dangerous condition that can lead to coma and death. It is also called "diabetic acidosis", "ketosis", "ketoacidosis" or "diabetic coma". DKA is a common way for new Type 1 diabetics to be diagnosed. If they fail to seek medical advice on symptoms like urination, which is driving thirst they can die of DKA. Oral magnesium supplements reduce erythrocyte[2] dehydration.[3] In general, optimal balances of electrolytes are necessary to maintain the best possible hydration. Diabetic thirst is initiated specifically by magnesium deficiency with relative calcium excess in the cells. Even water, our most basic nutrient starts having a hard time getting into the cells with more going out through the kidneys. If your magnesium supplementation is not working as desired, it may be due to a lack of available ATP. It would be advised to take a bioavailable form of niacinamide to facilitate NAD+ production, approximately 30 minutes before taking the magnesium supplement. A great bioavailable source of B-vitamins, including niacinamide, is local bee pollen. Autism and Magnesium DeficiencyWhen dealing with ASD and other neurological disorders in children it is important to know the signs of low magnesium: restless, can't keep still, body rocking, grinding teeth, hiccups, noise sensitive, poor attention span, poor concentration, irritable, aggressive, ready to explode, easily stressed. When it comes to children today we need to assume a large magnesium deficiency for several reasons. 1) The foods they are eating are stripped of magnesium because foods in general, as we shall see below are declining in mineral content in an alarming way. 2) The foods many children eat are highly processed junk foods that do not provide real nutrition to the body. 3) Because most children on the spectrum are not absorbing the minerals they need even when present in the gut. Magnesium absorption is dependent on intestinal health, which is compromised totally in leaky gut syndromes and other intestinal problems that the majority of autism syndrome disorders. 4) Because the oral supplements doctors rely on are not easily absorbed, because they are not in the right form and because magnesium in general is not administered easily orally. Modern medicine is supposed to help people not hurt them, but with their almost total ignorance of magnesium doctors end up hurting more than they help for many of the medical interventions drive down magnesium levels when they should be driving them up. Many if not most pharmaceutical drugs drive magnesium levels into very dangerous zones and surgery done without increasing magnesium levels is much more dangerous then surgery done with. The foundation of medical arrogance is actually medical ignorance and the only reason ignorance and arrogance rule the playing field of medicine is a greed lust for power and money. Human nature seems to be at its worst in modern medicine when it should be at its best. It is sad that people have to suffer needlessly and extraordinarily tragic that allopathic medicine has turned its back on the Hippocratic Oath and all that it means. Resources[1] https://www.nhfw.info/magnesium.html
[2] Red blood cells are also known as RBCs, red blood corpuscles (an archaic term), haematids or erythrocytes (from Greek erythros for "red" and kytos for "hollow", with cyte translated as "cell" in modern usage). The capitalized term Red Blood Cells is the proper name in the US for erythrocytes in storage solution used in transfusion medicine. [3] J. Clin. Invest. 100(7): 1847-1852 (1997). doi:10.1172/JCI119713. The American Society for Clinical Investigation
Safe and Effective: A Second Opinion shines a light on Covid-19 vaccine injuries and bereavements, but also takes an encompassing look at the systemic failings that appear to have enabled them. We look at leading analysis of pharmaceutical trials, the role of the MHRA in regulating these products, the role of the SAGE behavioural scientists in influencing policy and the role of the media and Big Tech companies in supressing free and open debate on the subject.
We’ve built an entire economy, not just in the United States but the entire Western civilization, on healthcare. For thousands of years, real control over populations has been around their food. Today, with billions of souls on the planet, controlling food has become a massive business and a means of ultimate political control. Between 1982 and 2000, something changed in our environment, overwhelming the immune system of the population. Diseases in different organ systems started going epidemic simultaneously, challenging the notion of a thousand different diseases.
In the late 1800s, we changed the way we farmed, leading to a disrespect for crop rotation and soil health. This disrespect for soil health resulted in the Dust Bowl of the 1920s and 30s, pushing us to outsource our food production and rely on imported food. After World War II, with a surplus of petroleum, we started producing chemical-based fertilizers, leading to the Green Revolution. While plants turned green due to nitrogen and phosphorus, they lacked essential nutrients and medicine. This deficiency weakened plants, making them susceptible to diseases and pests. The chemical industry introduced pesticides and herbicides (including #Glyphosate), creating a co-dependent relationship between farmers and chemical solutions. Similarly, in healthcare, we’ve become dependent on drugs to manage symptoms, creating a cycle of side effects and more medications. The epidemic rise in diseases like autism, Alzheimer’s, Parkinson’s, and autoimmune disorders signals a deeper problem, challenging our understanding of the root cause of diseases. It’s time to reconsider our approach to health, starting with understanding the importance of soil health and nutrition. Just as respecting soil is crucial for healthy crops, prioritizing our body’s nutritional needs is fundamental for overall well-being. Let’s shift our focus from symptom management to addressing the root cause, promoting a holistic approach to health. Zach Bush, MD is triple board-certified physician specializing in internal medicine, endocrinology and hospice care. He is the founder of Seraphic Group, an organization devoted to developing root-cause solutions for human and ecological health in the sectors of big farming, big pharma, and Western Medicine at large. And he is also the founder of Farmers Footprint https://farmersfootprint.us/, a non-profit coalition of farmers, educators, doctors, scientists, and business leaders aiming to expose the deleterious human and environmental impacts of chemical farming and pesticide reliance - while simultaneously offering a path forward through regenerative agricultural practices.
Geert Vanden Bossche, PhD, DVM, is an internationally recognized vaccine research expert and developer. He has a long list of companies and organizations he’s worked with on vaccine discovery and preclinical research, including the head of the Vaccine Development Office at the German Centre for Infection Research, GSK, Novartis, Solvay Biologicals, and Bill & Melinda Gates Foundation. Dr Vanden Bossche also coordinated the Ebola vaccine program at GAVI (Global Alliance for Vaccines and Immunization) and contributed to the implementation of an integrated vaccine work plan in collaboration with Global Health Partners (WHO, Bill & Melinda Gates Foundation, CDC, UNICEF), regulators (FDA) and vaccine manufacturers to enable timely deployment or stockpiling of Ebola vaccine candidates.
He is board-certified in Virology and Microbiology, the author of over 30 publications, and inventor of a patent application for universal vaccines. He currently works as an independent vaccine research consultant. In this following video, he shares his perspective on mass vaccination of SARS-CoV2, and highlights the principle of using a prophylactic vaccine in the midst of a pandemic, which is likely to create more viral variants in the process. Bossche states that the multiple emerging, “much more infectious” viral variants, are already examples of “immune escape” from our ‘innate immunity’, and were most-likely created by the government interventions themselves; the so-called Non-Pharmacological Interventions (NPIs) – i.e. lockdowns and cloth facial coverings. Unofficially, but also more aptly known as the Non-Scientific Interventions. He believes that:
He states that to “fully escape”, the highly mutable virus, “only needs to add another few mutations in its receptor-binding domain”. Below is his open letter to the WHO, issued March 6th, 2021. Open Letter to the World Health Organization
Geert Vanden Bossche, DMV, PhD, independent virologist and vaccine expert, formerly employed at GAVI and The Bill & Melinda Gates Foundation.
To all authorities, scientists and experts around the world, to whom this concerns: the entire world population. I am all but an antivaxxer. As a scientist I do not usually appeal to any platform of this kind to make a stand on vaccine-related topics. As a dedicated virologist and vaccine expert I only make an exception when health authorities allow vaccines to be administered in ways that threaten public health, most certainly when scientific evidence is being ignored. The present extremely critical situation forces me to spread this emergency call. As the unprecedented extent of human intervention in the Covid-19- pandemic is now at risk of resulting in a global catastrophe without equal, this call cannot sound loudly and strongly enough. As stated, I am not against vaccination. On the contrary, I can assure you that each of the current vaccines have been designed, developed and manufactured by brilliant and competent scientists. However, this type of prophylactic vaccines are completely inappropriate, and even highly dangerous, when used in mass vaccination campaigns during a viral pandemic. Vaccinologists, scientists and clinicians are blinded by the positive short-term effects in individual patents, but don’t seem to bother about the disastrous consequences for global health. Unless I am scientifically proven wrong, it is difficult to understand how current human interventions will prevent circulating variants from turning into a wild monster. Racing against the clock, I am completing my scientific manuscript, the publication of which is, unfortunately, likely to come too late given the ever increasing threat from rapidly spreading, highly infectious variants. This is why I decided to already post a summary of my findings as well as my keynote speech at the recent Vaccine Summit in Ohio on LinkedIn. Last Monday, I provided international health organizations, including the WHO, with my analysis of the current pandemic as based on scientifically informed insights in the immune biology of Covid-19. Given the level of emergency, I urged them to consider my concerns and to initiate a debate on the detrimental consequences of further ‘viral immune escape’. For those who are no experts in this field, I am attaching below a more accessible and comprehensible version of the science behind this insidious phenomenon. While there is no time to spare, I have not received any feedback thus far. Experts and politicians have remained silent while obviously still eager to talk about relaxing infection prevention rules and 'springtime freedom'. My statements are based on nothing else but science. They shall only be contradicted by science. While one can barely make any incorrect scientific statements without being criticized by peers, it seems like the elite of scientists who are currently advising our world leaders prefer to stay silent. Sufficient scientific evidence has been brought to the table. Unfortunately, it remains untouched by those who have the power to act. How long can one ignore the problem when there is at present massive evidence that viral immune escape is now threatening humanity? We can hardly say we didn't know - or were not warned. In this agonizing letter I put all of my reputation and credibility at stake. I expect from you, guardians of mankind, at least the same. It is of utmost urgency. Do open the debate. By all means: turn the tide! PUBLIC HEALTH EMERGENCY OF INTERNATIONAL CONCERN Why mass vaccination amidst a pandemic creates an irrepressible monster THE key question is: why does nobody seem to bother about viral immune escape? Let me try to explain this by means of a more easily understood phenomenon: Antimicrobial resistance. One can easily extrapolate this scourge to resistance to our self-made ‘antiviral antibiotics’. Indeed, antibodies (Abs) produced by our own immune system can be considered self-made antiviral antibiotics, regardless of whether they are part of our innate immune system (so-called ‘natural’ Abs’) or elicited in response to specific pathogens (resulting in so-called ‘acquired’ Abs). Natural Abs are not germ-specific whereas acquired Abs are specifically directed at the invading pathogen. At birth, our innate immune system is ‘unexperienced’ but well-established. It protects us from a multitude of pathogens, thereby preventing these pathogens from causing disease. As the innate immune system cannot remember the pathogens it encountered (innate immunity has no so-called ‘immunological memory’), we can only continue to rely on it provided we keep it ‘trained’ well enough. Training is achieved by regular exposure to a myriad of environmental agents, including pathogens. However, as we age, we will increasingly face situations where our innate immunity (often called ‘the first line of immune defense’) is not strong enough to halt the pathogen at the portal of entry (mostly mucosal barriers like respiratory or intestinal epithelia). When this happens, the immune system has to rely on more specialized effectors of our immune system (i.e., antigen-specific Abs and T cells) to fight the pathogen. So, as we grow up, we increasingly mount pathogen-specific immunity, including highly specific Abs. As those have stronger affinity for the pathogen (e.g., virus) and can reach high concentrations, they can quite easily outcompete our natural Abs for binding to the pathogen/virus. It is precisely this type of highly specific, high affinity Abs that current Covid-19 vaccines are inducing. Of course, the noble purpose of these Abs is to protect us against Covid-19. So, why then should there be a major concern using these vaccines to fight Covid-19? Well, similar to the rules applying to classical antimicrobial antibiotics, it is paramount that our self-made ‘antiviral antibiotics’ are made available in sufficient concentration and are tailored at the specific features of our enemy. This is why in case of bacterial disease it is critical to not only chose the right type of antibiotic (based on the results from an antibiogram) but to also take the antibiotic for long enough (according to the prescription). Failure to comply with these requirements is at risk of granting microbes a chance to survive and hence, may cause the disease to fare up. A very similar mechanism may also apply to viruses, especially to viruses that can easily and rapidly mutate (which is, for example, the case with Coronaviruses); when the pressure exerted by the army’s (read: population’s) immune defense starts to threaten viral replication and transmission, the virus will take on another coat so that it can no longer be easily recognized and, therefore, attacked by the host immune system. The virus is now able to escape immunity (so-called: ‘immune escape’). However, the virus can only rely on this strategy provided it still has room enough to replicate. Viruses, in contrast to the majority of bacteria, must rely on living host cells to replicate. This is why the occurrence of ‘escape mutants’ isn’t too worrisome as long as the likelihood for these variants to rapidly find another host is quite remote. However, that’s not particularly the case during a viral pandemic! During a pandemic, the virus is spreading all over the globe with many subjects shedding and transmitting the virus (even including asymptomatic ‘carriers’). The higher the viral load, the higher the likelihood for the virus to bump into subjects who haven’t been infected yet or who were infected but didn’t develop symptoms. Unless they are sufficiently protected by their innate immune defense (through natural Abs), they will catch Covid-19 disease as they cannot rely on other, i.e., acquired Abs. It has been extensively reported, indeed, that the increase in S (spike)-specific Abs in asymptomatically infected people is rather limited and only short-lived. Furthermore, these Abs have not achieved full maturity. The combination of viral infection on a background of suboptimal Ab maturity and concentration enables the virus to select mutations allowing it to escape the immune pressure. The selection of those mutations preferably occurs in the S protein as this is the viral protein that is responsible for viral infectiousness. As the selected mutations endow the virus with increased infectious capacity, it now becomes much easier for the virus to cause severe disease in infected subjects. The more people develop symptomatic disease, the better the virus can secure its propagation and perpetuation (people who get severe disease will shed more virus and for a longer period of time than asymptomatically infected subjects do). Unfortunately enough, the short-lived rise in S-specific Abs does, however, suffice to bypass people’s innate/natural Ab. Those are put out of business as their affinity for S is lower than the affinity of S-specific Abs. This is to say that with an increasing rate of infection in the population, the number of subjects who get infected while experiencing a momentary increase in Specific Abs will steadily increase. Consequently, the number of subjects who get infected while experiencing a momentary decrease in their innate immunity will increase. As a result, a steadily increasing number of subjects will become more susceptible to getting severe disease instead of showing only mild symptoms (i.e., limited to the upper respiratory tract) or no symptoms at all. During a pandemic, especially youngsters will be affected by this evolution as their natural Abs are not yet largely suppressed by a panoply of ‘acquired’, antigen-specific Abs. Natural Abs, and natural immunity in general, play a critical role in protecting us from pathogens as they constitute our first line of immune defense. In contrast to acquired immunity, innate immune responses protect against a large spectrum of pathogens (so don’t compromise or sacrifice your innate immune defense!). Because natural Abs and innate immune cells recognize a diversified spectrum of foreign (i.e., non-self) agents (only some of which have pathogenic potential), it’s important, indeed, to keep it sufficiently exposed to environmental challenges. By keeping the innate immune system (which, unfortunately, has no memory!) TRAINED, we can much more easily resist germs which have real pathogenic potential. It has, for example, been reported and scientifically proven that exposure to other, quite harmless Coronaviruses causing a ‘common cold ’ can provide protection, although short-lived, against Covid-19 and its loyal henchmen (i.e., the more infectious variants). Suppression of innate immunity, especially in the younger age groups, can, therefore, become very problematic. There can be no doubt that lack of exposure due to stringent containment measures implemented as of the beginning of the pandemic has not been beneficial to keeping people’s innate immune system well trained. As if this was not already heavily compromising innate immune defense in this population segment, there comes yet another force into play that will dramatically enhance morbidity and mortality rates in the younger age groups: MASS VACCINATION of the ELDERLY. The more extensively the later age group will be vaccinated and hence, protected, the more the virus is forced to continue causing disease in younger age groups. This is only going to be possible provided it escapes to the S-specific Abs that are momentarily raised in previously asymptomatically infected subjects. If the virus manages to do so, it can benefit from the (momentarily) suppressed innate immunity, thereby causing disease in an increasing number of these subjects and ensuring its own propagation. Selecting targeted mutations in the S protein is, therefore, the way to go in order for the virus to enhance its infectiousness in candidates that are prone to getting the disease because of a transient weakness of their innate immune defense. But in the meantime, we’re also facing a huge problem in vaccinated people as they’re now more and more confronted with infectious variants displaying a type of S protein that is increasingly different from Author: Geert Vanden Bossche, DVM, PhD (March 6, 2021) – https://www.linkedin.com/in/geertvandenbossche/ the S edition comprised with the vaccine (the later edition originates from the original, much less infectious strain at the beginning of the pandemic). The more variants become infectious (i.e., as a result of blocking access of the virus to the vaccinated segment of the population), the less vaccinal Abs will protect. Already now, lack of protection is leading to viral shedding and transmission in vaccine recipients who are exposed to these more infectious strains (which, by the way, increasingly dominate the field). This is how we are currently turning vaccines into asymptomatic carriers shedding infectious variants. At some point, in a likely very near future, it’s going to become more profitable (in term of ‘return on selection investment’) for the virus to just add another few mutations (maybe just one or two) to the S protein of viral variants (already endowed with multiple mutations enhancing infectiousness) in an attempt to further strengthen its binding to the receptor (ACE-2) expressed on the surface of permissive epithelial cells. This will now allow the new variant to outcompete vaccinal Abs for binding to the ACE receptor. This is to say that at this stage, it would only take very few additional targeted mutations within the viral receptor-binding domain to fully resist specific anti-Covid-19 Abs, regardless whether the later are elicited by the vaccine or by natural infection. At that stage, the virus will, indeed, have managed to gain access to a huge reservoir of subjects who have now become highly susceptible to disease as their S-specific Abs have now become useless in terms of protection but still manage to provide for long-lived suppression of their innate immunity (i.e., natural infection, and especially vaccination, elicit relatively long-lived specific Ab titers). The susceptible reservoir comprises both, vaccinated people and those who’re left with sufficient S-specific Abs due to previous Covid-19 disease). So, MISSION ACCOMPLISHED for Covid-19 but a DISASTROUS SITUATION for all vaccinated subjects and Covid-19 seropositive people as they’ve now lost both, their acquired and innate immune defense against Covid-19 (while highly infectious strains are circulating!). That’s ‘one small step for the virus, one giant catastrophe for mankind’, which is to say that we’ll have whipped up the virus in the younger population up to a level that it now takes little effort for Covid-19 to transform into a highly infectious virus that completely ignores both the innate arm of our immune system as well as the adaptive/acquired one (regardless of whether the acquired Abs resulted from vaccination or natural infection). The effort for the virus is now becoming even more negligible given that many vaccine recipients are now exposed to highly infectious viral variants while having received only a single shot of the vaccine. Hence, they are endowed with Abs that have not yet acquired optimal functionality. There is no need to explain that this is just going to further enhance immune escape. Basically, we’ll very soon be confronted with a super-infectious virus that completely resists our most precious defense mechanism: The human immune system. From all of the above, it’s becoming increasingly difficult to imagine how the consequences of the extensive and erroneous human intervention in this pandemic are not going to wipe out large parts of our human population. One could only think of very few other strategies to achieve the same level of efficiency in turning a relatively harmless virus into a bioweapon of mass destruction. It’s certainly also worth mentioning that mutations in the S protein (i.e., exactly the same protein that is subject to selection of escape mutations) are known to enable Coronaviruses to cross species barriers. This is to say that the risk that vaccine-mediated immune escape could allow the virus to jump to other animal species, especially industrial livestock (e.g., pig and poultry farms), is not negligible. These species are already known to host several different Coronaviruses and are usually housed in farms with high stocking density. Similar to the situation with influenza virus, these species could than serve as an additional reservoir for SARS-COVID-2 virus. As pathogens have co-evolved with the host immune system, natural pandemics of acute self-limiting viral infections have been shaped such as to take a toll on human lives that is not higher than strictly required. Due to human intervention, the course of this pandemic has been thoroughly disturbed as of the very beginning. Widespread and stringent infection prevention measures combined with mass vaccination campaigns using inadequate vaccines will undoubtedly lead to a situation where the pandemic is getting increasingly ‘out of control’. Paradoxically, the only intervention that could offer a perspective to end this pandemic (other than to let it run its disastrous course) is …VACCINATION. Of course, the type of vaccines to be used would be completely different of conventional vaccines in that they’re not inducing the usual suspects, i.e., B and T cells, but NK cells. There is, indeed, compelling scientific evidence that these cells play a key role in facilitating complete elimination of Covid-19 at an early stage of infection in symptomatically infected subjects. NK cells are part of the cellular arm of our innate immune system and, alike natural Abs, they are capable of recognizing and attacking a broad and diversified spectrum of pathogenic agents. There is a sound scientific rationale to assume that it is possible to ‘prime’ NK cells in ways for them to recognize and kill Coronaviruses at large (include all their variants) at an early stage of infection. NK cells have increasingly been described to be endowed with the capacity to acquire immunological memory. By educating these cells in ways that enable them to durably recognize and target Coronavirus-infected cells, our immune system could be perfectly armed for a targeted attack to the universe of Coronaviruses prior to exposure. As NK cell-based immune defense provides sterilizing immunity and allows for broadspectrum and fast protection, it is reasonable to assume that harnessing our innate immune cells is going to be the only type of human intervention left to halt the dangerous spread of highly infectious Covid-19 variants. If we, human beings, are committed to perpetuating our species, we have no choice left but to eradicate these highly infectious viral variants. This will, indeed, require large vaccination campaigns. However, NK cell-based vaccines will primarily enable our natural immunity to be better prepared (memory!) and to induce herd immunity (which is exactly the opposite of what current Covid-19 vaccines do as those increasingly turn vaccine recipients into asymptomatic carriers who are shedding virus). So, there is not one second left for gears to be switched and to replace the current killer vaccines by life-saving vaccines. I am appealing to the WHO and all stakeholders involved, no mater their conviction, to immediately declare such acton as THE SINGLE MOST IMPORTANT PUBLIC HEALTH EMERGENCY OF INTERNATIONAL CONCERN. Zach Bush MD is a physician specializing in internal medicine, endocrinology and hospice care. He is an internationally recognized educator and thought leader on the microbiome as it relates to health, disease, and food systems. Dr Zach founded Seraphic Group and the nonprofit Farmer’s Footprint to develop root-cause solutions for human and ecological health. His passion for education reaches across many disciplines, including topics such as the role of soil and water ecosystems in human genomics, immunity, and gut/brain health. His education has highlighted the need for a radical departure from chemical farming and pharmacy, and his ongoing efforts are providing a path for consumers, farmers, and mega-industries to work together for a healthy future for people and planet.
Show Notes
In this conversation, Dr. Tom Cowan and Sally Fallon Morrell discuss The Contagion Myth.
The official explanation for today’s COVID-19 pandemic is a “dangerous, infectious virus.” This is the rationale for isolating a large portion of the world’s population in their homes so as to curb its spread. From face masks to social distancing, from antivirals to vaccines, these measures are predicated on the assumption that tiny viruses can cause serious illness and that such illness is transmissible person-to-person. It was Louis Pasteur who convinced a skeptical medical community that contagious germs cause disease; his “germ theory” now serves as the official explanation for most illness. However, in his private diaries, he states unequivocally that in his entire career he was not once able to transfer disease with a pure culture of bacteria (he obviously wasn’t able to purify viruses at that time). He admitted that the whole effort to prove contagion was a failure, leading to his famous death bed confession that “the germ is nothing, the terrain is everything.” While the incidence and death statistics for COVID-19 may not be reliable, there is no question that many people have taken sick with a strange new disease—with odd symptoms like gasping for air and “fizzing” feelings—and hundreds of thousands have died. Many suspect that the cause is not viral but a kind of pollution unique to the modern age—electromagnetic pollution. Today we are surrounded by a jangle of overlapping and jarring frequencies—from power lines to the fridge to the cell phone. It started with the telegraph and progressed to worldwide electricity, then radar, then satellites that disrupt the ionosphere, then ubiquitous Wi-Fi. The most recent addition to this disturbing racket is fifth-generation wireless—5G. In The Contagion Myth: Why Viruses (including Coronavirus) are Not the Cause of Disease, bestselling authors Thomas S. Cowan, MD, and Sally Fallon Morell tackle the true causes of COVID-19. On September 26, 2019, 5G wireless was turned on in Wuhan, China (and officially launched November 1) with a grid of about ten thousand antennas—more antennas than exist in the whole United States, all concentrated in one city. A spike in cases occurred on February 13, the same week that Wuhan turned on its 5G network for monitoring traffic. Illness has subsequently followed 5G installation in all the major cities in America. Since the dawn of the human race, medicine men and physicians have wondered about the cause of disease, especially what we call “contagions,” numerous people ill with similar symptoms, all at the same time. Does humankind suffer these outbreaks at the hands of an angry god or evil spirit? A disturbance in the atmosphere, a miasma? Do we catch the illness from others or from some outside influence? As the restriction of our freedoms continues, more and more people are wondering whether this is true. Could a packet of RNA fragments, which cannot even be defined as a living organism, cause such havoc? Perhaps something else is involved—something that has upset the balance of nature and made us more susceptible to disease? Perhaps there is no “coronavirus” at all; perhaps, as Pasteur said, “the germ is nothing, the terrain is everything.” A group is suing Tulsa Mayor G.T. Bynum and Tulsa Health Department Executive Director Bruce Dart, saying the city’s mask mandate is harmful to healthy people.
Optometrist Robert Zoellner, Clay Clark, Dr. James Meehan, MD, and other Tulsa-based business owners are asking the city to immediately repeal the mask mandate which was passed by city council last month. The group alleges wearing masks is causing healthy people to become sick while trying to prevent the spread of a disease that is not a deadly threat to children and much of the public. “On the OSHA website it states that employers shouldn’t make employees work in an environment where they have less than a 19.5 percent oxygen level,” said Clayton Clark, one of the plaintiffs. “And the mandated masks cause employees to dip below a 19.5 percent oxygen level within 10 seconds of wearing a mask, so I don’t want to make my healthy employees sick.” From @ShawnModel:
Working with top experts, reviewing university and hospital databases, and scouring over an additional 50 peer-reviewed studies... what I discovered nearly left me speechless. What I happened upon was so surprising that I decided to examine the entire history of mask usage in medicine and study the peer-reviewed evidence that's been gathered since their inception. There was so much data available that I was even more speechless. In fact, the outcomes of some of these studies was so shocking that I couldn't believe public health officials weren't talking about them. So, I put a team together, collected all of the data, and put it all together for you here in this video. Additionally, you can access all of the studies at themodelhealthshow(dot)com/maskfacts or just hit the link in my bio. This is truly one of the most important moments in human history. It’s time to take action to get this information into the hands of our communities. And it’s time for us to stand up and change our world for the better!
From The Ben Greenfield Podcast:
Jay: "Hello, everybody. It's your beloved sidekick co-host of the Ben Greenfield Fitness Podcast, or at least that's what I like to tell myself at night to help me sleep better. I'm Dr. Jay Wiles. And Ben actually decided to fully turn over the podcast in its entirety to me and rename this podcast to the Dr. Jay Wiles Awesome Extravaganza Podcast. While I am by and large kidding, you are actually stuck with me today as we take a deep dive into all things heart rate variability or HRV. In the health and wellness and longevity sector, HRV has become a metric that has been highly discussed but is still quite misunderstood by many. So, I'm here to clear up the air and give you an in-depth explanation of HRV physiology, the metrics, and practical implications because it seems like every quantifying device nowadays has an HRV measure. And because of this and with my background, I'm constantly inundated with questions about this metric, and what it means, and how we can utilize it, and how we can actually implement it from a practical standpoint. Just so you know, you can find all today's shownotes at BenGreenfieldFitness.com/hrvpodcast. With all that said, let me see if I can set the stage as to why you should even listen to me in regards to the science of HRV and its utilization. Let me give you a little bit of a background on my clinical experience and personal usage of biofeedback. So, when I'm not podcasting, my day job is working as a clinical health psychologist with a specialty in complementary and integrative health, and namely, in psychophysiology or biofeedback. You might already be asking yourself, what is biofeedback? Well, in short, biofeedback is the use of your physiology to enhance self-awareness in order to promote self-regulation. Another way of putting this is that we become more mindfully aware of our physiological response via feedback so that we can inherently change our physiology through numerous techniques. My background is doing this with individuals who are suffering from physiological ailments such as chronic pain, tension-type headaches, migraines, hypertension, or other systemic problems of their physiology. I also see a large array of individuals for more psychological problems such as chronic and systemic stress, anxiety, depression, PTSD, and other symptomology. In the more growing body of research and in my own clinical practice, I'm working with individuals who are looking to enhance peak cognitive and physical performance. I've been working with numerous elite professional athletes and executives that have found HRV training to be the most effective behavioral intervention for enhancing performance. I'm board-certified in biofeedback and heart rate variability biofeedback and I have specialty training in the field of psychophysiology. This means that I've procured a specialized knowledge base alongside practical clinical skills in helping my patients through numerous biofeedback techniques, as well as an in-depth understanding of the bi-directional relationship between our psychological processes and physiological processes. One way or another way to think of biofeedback is to think about it as a learning process, like learning to play a musical instrument, a sport, or even a video game. We perform an action, then we observe the results and then repeat this action throughout the day in an effort to continue to attain the positive result or enhance the result. I've also heard some individuals refer to biofeedback as a psychophysiological mirror that will teach the individual to monitor, understand, and change their physiology. If I had to boil biofeedback down to its most simple terms, we are trying to teach the concept of self-regulation, which would be learning how to control behavior efficiently and immediately without the feedback. I'll get back to this in just a bit, but I wanted to set the stage for the upcoming talk. One of the key features of any biofeedback clinician will be through the teaching of self-regulatory skills and heart rate variability or HRV. Indeed, this is actually the most foundational skill to self-regulation in biofeedback. Within my company, which is called Thrive Wellness and Performance, I work with many different types of individuals ranging from those who are battling with significant stress and fatigue or burnout, or those who are looking to optimize peak performance like many elite athletes and executives. In this role, I provide a comprehensive HRV consultation and individual follow-up HRV coaching sessions to help individuals take back their health and improve overall health outcomes or peak performance. I only have my clients using what I have found to be the top HRV measuring devices and data collection available, which I will talk about later. But after this podcast, you might consider what a biofeedback coach might look like for you on your own personal journey towards health and well-being, longevity, and peak performance. So, today, I want to take a deep dive into the field of psychophysiology, into the field of metrics of heart rate variability, in resonance frequency training, heart rate variability and well-being, performance and recovery, how we interpret data from the wearables that we buy, and some of the pitfalls to devices that provide us maybe with some inaccurate measurement and artefact inclusion. I want this to be a one-stop-shop for all things heart rate variability, a podcast that you come back to when you have a question about heart rate variability. But I must say that there are entire Ph.D. programs in the field of psychophysiology, so we are going to just barely scratch the surface. But for the most part, that will actually look like a deep dive. So, with that said, let's jump on in. I feel like it is necessary to set the stage for why this even matters. In other words, I figured that you would all like some buy-in. From a consumer and a clinician standpoint, I'm normally bought into a topic area when there is vast robust research on that topic area. It's really interesting when you start to peruse the internet and PubMed for HRV studies. As you will see that there were actually minimal studies on this topic about 20 to 30 years ago. But from the '90s until especially the past decade, we have seen exponential advancements in how we practically utilize the important metric of HRV. Indeed, research has demonstrated some significant outcomes as to how we use HRV in predicting cardiac outcomes, especially after a myocardial infarction, which is a heart attack. HRV, over the course of a 24-hour period, is actually the greatest predictor for future heart attacks and is one of the, if not, the most reliable predictors that cardiologists will use. We also see in research how HRV is correlated with increased risk for cerebral vascular accident, which is a stroke, especially after someone has already had a stroke. We can also see a direct link between HRV and sleep, HRV and stress and cortisol production, HRV and depression, HRV and cognitive performance and in sports performance. All of these links and much more have been identified in peer-reviewed journal articles. So, this is just not some unstudied woo-woo metric. We have a lot of confounding data to support our use of this metric for many things. However, I do not want you to think that this is some panacea metric and can be used for any and every outcome. So, what have we found in research in regarding to how we can use HRV as a metric of our physiology? We have found that knowing our HRV and modifying our HRV can lead to improved mental health and well-being. It optimizes our ability to recover and adapt after exercise. It can lead to improved mental and cognitive performance, improved sleep insight into our nervous system and our nervous system-mediated pain, its insight into increased homeostasis of the nervous system that leads to improved stress outcomes, and can be a detection system of dysregulation in the central and peripheral nervous systems. An example of this is that a group of researchers found that individuals with chronic stress-related neck pain had significantly lower HRV scores than the normative population, which was found due to autonomic dysregulation, which I will explain later what that means, after 10 weeks of HRV biofeedback, these individuals were able to significantly increase their HRV which resulted in improved perceived health, increased vitality alongside reduced pain outcomes and improved social functioning. A study performed with physically fit men and women that assessed HRV in the relationship between anxiety and stress and one's engagement in physical exercise found that both men and women that perceive themselves as having higher stress had lower HRV scores regardless of their physical activity. So, while physical activity plays a significant role in HRV modulation, meaning that the more physically fit you are, the higher the HRV unless you are overtraining, emotional or psychological stress likely plays a more significant role in mediating HRV. A meta-analysis was performed in 2014 demonstrated that anxiety disorders are associated with significant reductions in HRV. From a sports performance perspective, an article in the Journal of Sport Science and Medicine in 2014 indicated that we are able to gain accurate insight into recovery via ultra-short-term HRV measurements, anything as low as 60 seconds. HRV has also been found to be associated with aerobic capacity, as researchers have identified, that those with lower aerobic capacity tend to have lower HRV scores. Additionally, those who report as more sedentary have lower HRV when compared to a more active population. And numerous studies have also indicated that a high HRV is associated with better general health due to it allowing the person to better adjust to both internal and external stimuli and that a low HRV is a predictor of cardiovascular disease and metabolic diseases and increases the overall risk for mortality. This does not even begin to scratch the surface but should go to show you that this metric is both highly useful. And I would argue, it is imperative for us to know our numbers and make necessary modifications. I also want to quickly highlight a few studies that demonstrate how we can use HRV biofeedback, which would be the use of strategies to enhance self-awareness and self-regulation of HRV. In the study of scientific literature on HRV, and more specifically on HRV biofeedback efficacy, we must turn to the most trusted organization for determining efficacy, which is the Association for Applied Psychophysiology and Biofeedback or AAPB. They provide a ranking system for HRV biofeedback efficacy from an analysis of outcome studies performed on HRV biofeedback for certain symptoms and disorders. The ranking system goes from level 1, which means that it is not empirically supported, all the way to level 5, which means that it is both efficacious and specific and has been statistically shown to be superior to credible sham therapy pill or alternative bona fide treatments in at least two independent study research settings. From a clinical standards perspective, you really want to stay within the level 3 to level 5 range, which level 4 being kind of where most effective treatments lie. Think of level 5 as saying that there is clear evidence that this is the standard modality for that disorder for treatments. That should always be the first line of treatment. Therefore, this is not seen very frequently. An example of this in the biofeedback world is a neurofeedback for those with ADHD. This is considered a level 5 treatment. Now, what does the literature say about HRV biofeedback for certain disorder sets? Well, there is robust research to support HRV biofeedback as a level 4 practice indicating high efficacy outcomes for depression and anxiety, hypertension which is high blood pressure, pre-hypertension, preeclampsia, IBS or irritable bowel syndrome, and chronic muscle pain. In the performance world, we see HRV biofeedback as a level 3 for optimized performance in baseball, basketball, dance, and in golf. And this is not to say that it cannot be utilized for other performance avenues, but this is where we have the most robust research. Another study in the Journal of Applied Psychophysiology and Biofeedback found that HRV biofeedback is an effective, safe, and easy to learn and apply method for both athletes and coaches in order to improve sports performance. In order to have an understanding of how we utilize HRV practically, we must understand the what and the why of our measurement. In order to gain an understanding of why HRV is important, we must take a dive into the field of psychophysiology. Like I alluded to earlier, psychophysiology is studying the interrelationship or the bi-directional relationship between psychological and physiological processes. We have to think of this relationship as both dynamic and bi-directional in nature. This means that it is constantly changing depending on the state of the organism and communicates in both directions. What I mean by this is that what happens within our psychological processes can influence our physiological processes and vice versa. Let me give you an easy-to-understand example. Let's think about hypertension or high blood pressure. It has been long determined that psychological stress can influence hypertension and cardiovascular disease outcomes. This means that somebody's psychological stress experience can inherently increase blood pressure, which is associated with numerous negative health outcomes. The interesting thing about this process though is that it is bi-directional. This means that as someone experiences an increase in blood pressure, which may not be necessarily due to psychological stressors, this physiological change can increase the anxiety or stress response of the individual. Basically, from an ancestral perspective, physiological changes in blood pressure send communication to the brain that there must be a threat. That is resulting in vascular constriction, increased heart rate and increased blood pressure. Therefore, our limbic system, and more specifically, our amygdala in the brain sends our body and our brain into an action-oriented response so that we can either fight or flee from the threat that's in front of us. This is both a conscious and an unconscious response. Another way that we can view this is through the lens of what is called the psychophysiological principle. This principle states that every change in the physiological state is accompanied by an appropriate change in the mental-emotional state, and this is again conscious or unconscious. And then conversely, every change in our emotional or mental state, both conscious or unconscious, is accompanied by an appropriate change in the physiological state. Again, these interconnected and bi-directional relationships. Yet another example of this is when we think about the role that facial muscle contraction can have an influencing emotion and how emotion can influence facial muscle contraction. So, someone that may get a Botox injection, which would actually paralyze facial muscles to treat wrinkles can actually reduce the intensity of a person's emotional experience. Yes, we have a lot of interesting research on this topic. One thing to remember at the foundation of our physiology is that each and every human being is striving for homeostasis, which is the maintenance of the body's internal environment with healthy physiological limits. A state of homeostasis is synonymous with the body striving for a process called allostasis. So, allostasis is a state of maintenance of stability through change and is a process that complements homeostasis. We achieved this state of allostasis through different mechanisms that anticipate challenges and adapt through behavior, a process of learning and then a physiological change. You can think of high HRV as evidence of our ability to adapt to stressors and maintain homeostasis. When we increase our HRV, this provides us with the ability to move in and out of a parasympathetic and sympathetic state as needed and as quickly and as efficiently as possible. I also refer to this as autonomic fortitude. The ability to shift in and out of a sympathetic and parasympathetic state demonstrates high HRV resilience or high heart rate variability resilience and is less likely to lead to things like adrenal fatigue, chronic stress, overtraining, and will yield better recovery. Unfortunately, the state of homeostasis and allostasis is combated with what we call a state of allostatic load. This is when our physiological, psychological, and spiritual adaptations have been significantly taxed, and now we are experiencing the deleterious effects as a result. You can kind of think of this as a balanced scale. In a state of homeostasis, we are adapting to change and challenge effectively. As we experience stressors and challenges that are too taxing on our physiology such as things like chronic pain, stress, depression, overexertion in exercise, toxic relationships, work stress, financial strain, and so forth, the scales become unbalanced and we can have systemic physiological and psychological problems that will arise. Let's think about this from an ancestral perspective. You may have heard of the comparison of how our ancestors may have experienced rapid, acute, and transient states of high stress such as being chased by a mountain lion while hunting and gathering. But when they return to their homelands, their stress response would come back down to baseline. Therefore, there was an activation of the HPA axis or the hypothalamic-pituitary-adrenal axis, and that resulted in an increase–I should say an acute release of adrenaline and cortisol and other glucocorticoids. These levels which can be highly inflammatory would typically come back down after the perceived threat was mitigated and an increased sense of safety was established. However, in our modern society, one that has us entrenched and engulfed in our work and our perceived worth, we have found ourselves in a constant state of physiological arousal and stress, all of which turns on our fight-or-flight response to perceive threat. In a sense, it's almost like perceiving that the mountain lion is continuously chasing us in our modern society. When this occurs day after day, decade after decade, this is going to take a tremendous toll on our psychological, physiological, and spiritual well-being. That is why it is imperative for us to be continuously self-monitoring and mindful of what we have in our lives and how we live our lives and the potential detriment that this may be causing over time. Physiological states of arousal or the state of fight-or-flight is there for our survival and is much needed. However, at some point in time, we begin to experience this imbalance, which tells our brain that a threat is always going to occur, never shutting off or blunting the fight-or-flight response. And this is why we need to take a deep dive into what helps us maintain balance or allostasis and homeostasis. I think the best framework of HRV training is always through the lens of autonomic balance and psychological and physiological resilience. This turns us to the topic of the central nervous system and the peripheral nervous system. We cannot have a conversation on HRV without a conversation on the central nervous system and the peripheral nervous system. The simple way to think about the two is that the central nervous system consists of the brain and the spinal cord, while the peripheral nervous system consists of all the nerves that run out of the central nervous system and innervate every area of our body. You can think of this as all of our organs, all of our limbs, and the skin. Therefore, these two are interconnected and have a bi-directional relationship. The peripheral nervous system has two distinct branches. These are the somatic nervous system and the autonomic nervous system. You can think of the somatic nervous system as being in control of the skeletal muscles and will transmit different somatosensory information back to the central nervous system. Our autonomic nervous system regulates certain aspects of our physiology that occur automatically. These would be things like regulating our cardiac and smooth muscle or heart functioning and respiration. We can then divide the autonomic nervous system into three main systems or three main branches. These are the sympathetic division, the parasympathetic division, and the enteric division. In the study of biofeedback, and specifically heart rate variability, we are focused predominantly on the autonomic nervous system, and more specifically, the parasympathetic and sympathetic branches or divisions. Now, let's break down both of these divisions as there tends to be some confusion in this area. I will start by discussing the sympathetic nervous system. This is the division of our nervous system that readies us for action, challenge, and will regulate the activities that expand or expend energy. The sympathetic nervous system is in direct connection with our endocrine system and regulates certain hormonal responses. This is what helps us to respond to threats to our safety through mobilization, the fight-or-flight response, or a process of active avoidance. In comparison to the parasympathetic response, which I'll speak about later, the sympathetic nervous system responds more slowly and for longer periods of time. For instance, it takes the parasympathetic vagus system less than a second to respond, while the sympathetic nervous system takes about five seconds or greater. From a physiological standpoint, sympathetic nervous system cells are found in the gray matter of the thoracic and lumbar segments of the spinal cord. The sympathetic nervous system also directly innervates our adrenal medulla, which is the central portion of the adrenal gland. The adrenal medulla is actually responsible for the release of the neurotransmitters, epinephrine and norepinephrine when they are stimulated. In response, this reinforces the sympathetic activation of our visceral organs. When we release these neurotransmitters due to a stimulated stress response, this will increase muscular blood flow and will convert stored nutrients into glucose to power skeletal muscle contraction. Basically, this causes the release of neurotransmitters that can put us into action. When the sympathetic nervous system is activated, this can be considered a fight-or-flight response. When this happens on a short-term or acute or transient state, this can be quite effective in increasing performance, helping us to escape a threat, or helping us to fight a threat. There is common misperception and misconception that the sympathetic nervous system is detrimental due to the release of glucocorticoids and stress hormones. We have to keep in mind that while chronic states of glucocorticoid secretion and stress hormone secretion can be a detriment to the body. Transient and acute activation of glucocorticoids and stress hormones can be quite beneficial. If you haven't done so already, I would highly encourage you to check out Dr. Craig Koniver's podcast that he did with Ben on cortisol and read one of the most–and I would also encourage you, I should say, to read one of the most thorough explanations on stress adaptation in a book called “Why Zebras Don't Get Ulcers” by Dr. Robert Sapolsky. From a physiological standpoint, there are many things that occur in our biology when our sympathetic state is kicked into high gear. In this state, we see a dilation of the pupils, an increased heartbeat, relaxed airways, inhibition of activity with the enteric nervous system, which is our gut. Of course, there is the secretion of epinephrine and norepinephrine, and then we also have a relaxed bladder. This is why someone might urinate on themselves if the sympathetic nervous system is activated extremely quickly in a tense situation. Think about it this way. When we perceive a threat in our environment, our body and brain directly communicate with one another and can shut off certain systems depending on what we need to take on the perceived threat. For instance, in a stress response, we have no use for reproduction. So, our reproductive organs are shut down. We do not want to expend blood in the gut to break down food because we do not need it and we need it elsewhere, like in our lungs, in our heart, and in our brain. And therefore, we deactivate our digestive systems. Now that we have a better understanding of the sympathetic nervous system, let's talk about the parasympathetic nervous system, which works in tandem with the sympathetic nervous system. I may need to also clarify that when we talk about the concept of autonomic balance, we are talking about a balancing of the two nervous systems. There's this notion that the sympathetic nervous system is the villain and the parasympathetic nervous system is the hero. This indeed is a fallacy and is a misunderstanding of the complex interrelationship between both divisions of our autonomic nervous system when in fact, it is a balance of these two divisions that is going to increase heart rate variability and demonstrate better overall health outcomes. You wouldn't want have an overly active parasympathetic nervous system just like you would not want to have a chronically activated sympathetic nervous system. I will get back to more on this later, but for now, let's discuss the parasympathetic nervous system and division of the autonomic nervous system. The parasympathetic division helps to regulate activities that will naturally increase the body's energy reserves. When you think about this branch of the nervous system, we might consider it like the inhibitory reactor, whose attendance is to pull us towards homeostasis. That's when we experience that state of allostatic load that I was talking about earlier. The other thing that you might already be aware of that you will want to pair with the parasympathetic nervous system is with our tenth cranial nerve, which is referred to as the vagus nerve. The parasympathetic nervous system cell bodies are found in the nuclei of four of the cranial nerves, but also in the sacral region of the spinal cord. We see this in the vagus nerve, which innervates many of our primary organs such as our heart, our lungs, our esophagus, the stomach, pancreas, liver, and the intestines. This means that it has direct communication to affect change in these organ systems. Its main chemical messenger is a neurotransmitter called acetylcholine. While acetylcholine can act as an excitatory neurotransmitter in certain parts of the brain such as exciting the basal ganglia for movement, acetylcholine actually acts predominantly as an inhibitory neurotransmitter within the parasympathetic division. When I say that it acts as an inhibitory neurotransmitter, this means that it results in reduced firing of nerve cells, which is going to be in direct opposition to the sympathetic activation that may be occurring. The parasympathetic nervous system is primarily mediated by the vagus nerve and has been referred to as the rest and digest branch of the autonomic nervous system. Some predominant researchers, particularly Dr. Stephen Porges, has found that the vagus nerve is mediated by a sense of safety and security. And I'll talk a lot more about this later. One way I like to think of this is that when we can intentionally create a safe space physically and psychologically, we are going to exhibit action in the vagus nerve. Another example of this would be how breathwork can modulate the parasympathetic nervous system and increase HRV on an acute level. If we take the time and we are able to take an intentional slow diaphragmatic breath, this is communicating to both our mind and body that we are in a safe place and we are able to engage in this behavior. This may not occur, let's say, if we are being chased by a mountain lion. For our survival, we do not want to pump the brakes and give our mind and body the message to relax in that case. It is a time where we need all of our resources and faculties to get out of the situation. One more thing that I will say about the parasympathetic nervous system is that it indeed works as a brake to the sympathetic nervous system. You can think of it as working similarly to a car. When the car is put in park, it will–or I should say when the car is put into drive, it will automatically accelerate without you having to press the gas pedal. This natural acceleration is like your sympathetic nervous system. It's always on. You're never going to be able to turn it off completely, but that's a good thing. It is scanning the environment for threats, which keeps us vigilant and keeps us safe. Now, you can floor the gas pedal and that would be like activating the sympathetic nervous system, and this is helpful in the immediate situations, but would be detrimental and result in a loss of fuel in a very long-term period. Whereas the parasympathetic nervous system works as that brake. It slows us down. The brake is leveraging the vagus nerve as the primary mediator. So, stimulating activation of the vagus nerve results in a cascade of beneficial psychophysiological outcomes when it's done at the right time. The last aspect of psychophysiology that is immensely important in the relationship between HRV is the process that we refer to as the baroreflex mechanism. One of the ways we maintain homeostasis is through a fully functional baroreflex response or baroreflex mechanism. This is actually a negative feedback loop that helps us to maintain homeostatic or stable blood pressure. Not only is this paramount to our survival as a species, but is also one of the primary areas of focus for heart rate variability biofeedback. This is because the aim of HRV biofeedback, which again is self-regulation of HRV, is to exercise the baroreceptor reflex to enhance homeostatic regulation and executive functions. The pathway is to modify our physiology by exercising the baroreflex in order to restore the dynamic autonomic balance of our nervous system. So, let me break it down in its most simplistic forms. Baroreflex or baroreceptors are these blood pressure receptors that are located in the aortic arch and the internal carotid arteries, which contribute to overall HRV. These receptors are referred to as stretch receptors or detection receptors. When you inhale, your heart rate is going to naturally increase. This will result in a rise in blood pressure about five seconds after this heart rate is increased. This increase in blood pressure will cause a stretch in the carotid arteries alongside the aortic arch causing the baroreceptors to fire action potentials at a very rapid rate. This rapid firing is sent through your tenth cranial nerve which is the vagus nerve, and the ninth cranial nerve which is the glossopharyngeal nerve to a part of our hindbrain referred to as the medulla, and more specifically, the nucleus of the solitary tract. This area of our brain will receive the signaling from the baroreceptors and will then subsequently activate the parasympathetic nervous system, which is, of course, our rest and digest branch of the nervous system. This process will also inhibit the sympathetic nervous system from signaling. The signaling of the parasympathetic nervous system will then result in a release of the neurotransmitter acetylcholine, which I said is again an inhibitory neurotransmitter, which inhibits and works on our pacemaker cells found in the sinoatrial node or the SA node of the heart. This will result in vasodilation, which is the opening of blood vessels to allow the increase of blood flow and will result in subsequent decreased blood pressure. Because of this mechanism, the heart rate will be brought back down to stable functioning. So, conversely, when someone has a sudden drop in blood pressure, the decreased blood pressure will then signal the medulla to inhibit the parasympathetic nervous system and will initiate action in the sympathetic nervous system. The sympathetic nervous system will begin to release norepinephrine and epinephrine, which will act again on that same area, the SA node of the heart to increase heart rate and will result in vasoconstriction, which will increase blood pressure. So, all in all, the baroreflex response is a sudden response and is a response to sudden changes in blood pressure that helps our bodies to regulate the impact of everyday activities and changes in emotional states. If, for instance, these things are not well-managed and result in hypertension, what the body will do is it will actually adjust and begin to see these elevations as the new normal levels because the body is always looking to adapt and create a new set point and the thermostat that we call homeostasis. The end result is that yes, you have high blood pressure, but you also have lower HRV. This is why modulating HRV by exercising our baroreflex and signaling the parasympathetic nervous system has a vast importance. Alright. So, now, it's time to link everything that we've discussed thus far into the topic of heart rate variability or HRV. In its most simplistic form, HRV or heart rate variability refers to the beat to beat variation in the time intervals between heart contractions. When we think about the oscillations of a healthy heart, they are actually quite complex. The healthy heart is typically seen as one that can rapidly adjust to sudden physical and psychological challenges. HRV is absolutely crucial to our overall health, resilience, and may be increased through different behavioral activations and practices like effortless breathing, exercise, compassion practices, and mindfulness practices. Within the research field of HRV, we define HRV as the fluctuation in time intervals between each adjacent heartbeat. Like I mentioned earlier, this is referred to as an interbeat interval and is typically measured in milliseconds. If you have any device that measures heart rate variability, it is probably utilizing a software algorithm that is probably calculating the interbeat interval between successive R spikes or the peaks of blood volume pulse. An R wave or an R spike would be read via an ECG or an electrocardiogram output, and this is the spike in electrical activity due to the depolarization of the ventricles of the heart. From an electrical standpoint, every heartbeat starts at what's called the SA node that I mentioned earlier, the sinoatrial node, which is also considered the heart's pacemaker. Interestingly enough, the natural pace of the heart without a fully functioning SA node is around 100 beats per minute, which by most standards, clinically, would be a form of tachycardia or a fast heartbeat. It is the SA node that helps to keep the heart on pace. The electrical signaling is what results in a cascade of complex events, which we call heartbeat. When we are measuring HRV on a majority of wearable devices, the algorithm is looking at peaks and blood volume through a device called photoplethysmography or PPG. These typically utilize infrared light sensors that shine through the skin and detect fluctuations in blood volume via the heart changes and pulse. Either measure that you're examining, one of the things that we know about the heart is that it is not a metronome. Indeed, if we see a heart that has consistent times in the interbeat intervals, we know that something is incredibly wrong with this individual's cardiovascular or nervous system. This is because at the heart of HRV is resilience. What I mean by this is that HRV's highest representation as a metric is on how resilient your physiology is to change. We have to keep in mind that we have trillions, yes, trillions among trillions of physiological processes occurring every moment within our biology. This means that the heart has a lot to keep up with. If the heart starts to regulate itself, kind of like a metronome, it is essentially the heart crying out for help, and sang aloud, I have no other choice but to regulate something amidst chaos. This sounds a little bit counterintuitive as it would seem like homeostasis would mean that the heart rate or heart rate variability would be consistent, but this is in fact very far from the truth. What we know from research is that heart rate variability is one of the most studied and highly accurate measurements and metrics for assessing the stress response, cardiovascular-related mortality and mobility and performance recovery. So, what are the sources of HRV? So, HRV is produced by two distinct overlapping processes. First is the concept of autonomic balance, which we talked about earlier. But to remind you, that is the complex relationship between both the parasympathetic and sympathetic divisions of the autonomic nervous system. The other are the regulatory mechanisms that control heart rate via a few processes. These include a process called respiratory sinus arrhythmia, the baroreflex, and rhythmic changes in vascular tone. I've already discussed the baroreflex. So, now let's talk about respiratory sinus arrhythmia or RSA. So, RSA is an extremely important concept in HRV regulation and optimization. We can actually use this process to manipulate our overall heart rate variability. You can do this. Anyone can do this. Respiratory sinus arrhythmia is the speeding and slowing of the heart across the breathing cycle. When we slow our breathing pattern down, we see a couple of things occurring physiologically. First, as we inhale, our heart rate will naturally incline to its peak. And when we exhale, and as we exhale, the heart will lower to its trough point. This makes sense if we think about it. As we are inhaling, the body is receiving usable oxygen to be delivered throughout the body into the brain. Therefore, the heart needs to utilize this immediately and will increase its cardiac output for the delivery of oxygen and gas exchange throughout the body. As we increase RSA, this rhythm, through low and slow breathing, we can actually stimulate vagal tone and, which again that's the vagus nerve, and we can lower blood pressure through the baroreflex mechanism. So, now let's shift to the metrics of HRV. It's likely if you have any HRV measuring devices that you have seen that this device calculates HRV through a means of SDNN or RMSSD, or it may measure low-frequency or high-frequency, and it's likely that you have no idea what this means or have had to look it up and still do not understand what it means. I want to clarify these measurements and give you my opinion on what you should be looking for and how to base your numbers on the norms and your own baselines. First of all, we need to differentiate between the types of HRV measurement. There are two predominant types of measurements that I'm going to talk about today. One is the time domain measurement, and the other is a frequency band or frequency domain measurement. Both of these are looking at different metrics. So, now, let's start with the time-domain measurement. When I speak about time-domain HRV measurements, I'm talking about a measurement that is calculated based on time intervals between each adjacent heartbeat. A little while ago, I mentioned how the heart does not function like a metronome. There are different time intervals in between each adjacent heartbeat where one heartbeat to another may be 800 milliseconds and the next adjacent heartbeat may only be 750 milliseconds. This shows variability in the time intervals. The difference between those two that I just mentioned is 50 milliseconds. And so therefore, we can say that there was 50 milliseconds of variability between the two sets of heartbeats. Now, as with anything in science, we're not going to base our HRV score on two sets of interbeat intervals as this is much too small of a sample size to give us any relevant or usable data. You would never base it on that. This is why we have to assess HRV over a period of time intervals. The amount of time needed for different calculations is going to vary depending on the type of time domain index you are interested in examining. For instance, the two primary usable time domain indices that we see most commonly are SDNN and RMSSD, and I'm going to explain the difference in just a minute. These both require different time domains to get accurate measurement or usable data. So, SDNN, for example, requires a minimum of five minutes, but in reality, it's really only clinically relevant if we assess over 24-hour period, and I'll explain more about what I mean about that in a second. While the RMSSD metric has actually been shown to provide valuable interpretations at as low as 10 seconds, 30 seconds, and 180 seconds. However, like SDNN, RMSSD is most accurate over a five-minute period. So, it will be important for you to know what you are calculating and what timeframe you need to measure or to provide or ensure accurate measurement. So, let's dive into the primary time domains. We will start with what is considered the gold standard of HRV measurement, which is SDNN. So, SDNN stands for the standard deviation of the interbeat intervals of normal sinus beats, which is measured again in milliseconds. Remember that this is measuring normal sinus beats and not artifact. This is one of the things that really irks me more than others is that we have a lot of devices that use the SDNN algorithm but do not remove artifact beats, which are essentially like ectopic beats or false or error beats due to things like movement, electrical interference, or changes in lining. And when that happens, you have data that's fairly void and unusable. And actually, technically, you cannot say that you are calculating SDNN if you do not remove artifact. That would actually be another metric called SDRR. So, unfortunately, many devices that calculate SDNN either do not have this artifacting built-in or it is based on very poor removal resulting in fairly inaccurate HRV data. I'd say that I'm quite the HRV snob, so it's something that I always look into. A similar measurement, which I just mentioned earlier, is SDRR, and that calculates all the sinus beats, even abnormal or false beats. The problem with this measurement though, which in a lot of our wearables, is that you can have abnormal beats that reflect cardiac dysfunction or even noise, but it will masquerade as HRV. So, I never use the SDRR data. But back to SDNN, when we talk about the standard deviation of interbeat intervals, what we are talking about is how much on average does each beat differ from the next. The reason this is considered the gold standard of HRV measurement is because it has been found to have contributions from both the sympathetic nervous system and parasympathetic nervous system. So, we can get full insight into our autonomic response with this measurement. Like I mentioned before, SDNN is most accurate when it is assessed over 24 hours than during short periods because the longer periods can provide data about cardiac reactions to a great range of environmental stimulation, or lack thereof in the case of sleep. It is also the 24-hour recordings that allow us to assess the sympathetic nervous system contribution to SDNN. For assessing cardiac risk, SDNN is almost always used and can be a valuable predictor of both morbidity and mortality. And looking at 24-hour recordings, an SDNN less than 50 milliseconds has been demonstrated in those classified as unhealthy. Those with 50 milliseconds to 100 milliseconds is a classification for compromised health, and 100 milliseconds and above is considered a healthy individual from a cardiac standpoint. When we look at heart attack survivors, those who have had a higher classification had a greater risk of living–or sorry, I should say a greater probability of living during a 31-month follow-up period. One study demonstrated that individuals with an SDNN greater than 100 milliseconds had a 5.3 times lower risk of mortality at follow-up than those with values less than 50 milliseconds. We can actually correlate the SDNN metric with other frequency domains that I will discuss later. SDNN is correlated with the ultra-low-frequency band, the very low-frequency band, and the low-frequency band. Now, let's turn to another time-domain index for HRV. And for short-term time-domain evaluation, it's probably my most preferred measure, which is the RMSSD metric. So, RMSSD is the root mean square of successive differences between normal heartbeats. And now that I have sufficed in spinning your heads, let me explain it. In order to calculate this value, we must calculate each successive time difference between adjacent interbeat intervals in terms of milliseconds. Then each of these values is squared and the result is then averaged before the square root of the total is obtained. Now, that is a lot of what we do in research. So, I wanted to give you that equation, but for the sake of practicality, it may not be necessarily that important. The measurement is mediated or provides us insight into the workings of our parasympathetic nervous system and is highly correlated with the high-frequency band. We actually know that RMSSD is more influenced by the parasympathetic branch than SDNN. While a five-minute measurement is the gold standard for RMSSD, you can get usable data in ultra-short-term domains that I mentioned at the beginning of this podcast. This makes it really good as an on-the-go measurement. One thing that I like about RMSSD is that it is not mediated by respiratory sinus arrhythmia like SDNN is. What I mean by this is that with SDNN, you can affect change in this number by taking those low and slow diaphragmatic breaths. Whereas RMSSD does not appear to be mediated by respiration or slow breathing and may provide more insight into recovery as it is primarily assessing tonic or relaxed or static HRV. So, if you want to gain insight into your recovery and remove the effects of respiration to assess non-manipulated HRV, RMSSD is the way to go. So, that's the one I use for recovery. This is one of the best measures of vagal tone due to the lack of manipulation of respiration. This is why I actually like the use of the Oura ring to assess HRV at night while I sleep, but more about that later. Another one that is used quite frequently and is very easy to assess in the HRV time domains is something called HRV amplitude. This is a very simple measurement that is an average of the difference between the highest and lowest heart rate during each respiratory cycle. So, remember, RSA or respiratory sinus arrhythmia is the fluctuation of heart rate from the start to the finish of a breath cycle. Normal RSA occurs when you inhale and your heart rate increases, and when you exhale, your heart rate decreases. If you subtract the peak heart rate in the cycle and the lowest heart rate at the end of the cycle, this will provide HRV amplitude. So, this is not a great index of vagal tone as it can be mediated by respiration. This measure normally depends on both age and fitness level. As we age, HRV, and especially amplitude, tends to go down. The more sedentary we are, the lower the amplitude we are likely to have. In elite athletes, I have seen amplitude as high as 50 to 60 beats per minute. This means that at the start of their exhale, their heart rate is at 50 beats per minute, and at the peak of their respiratory cycle, the heart rate gets up to about 100 beats per minute, and then comes back down to 50 beats per minute on the exhale. Whereas I've seen some patients with cardiovascular disease or chronic pain go from 70 beats per minute to 73 beats per minute, which would only be an amplitude or heart rate variability of 3 beats per minute, which is extremely low. This is where we might warrant some HRV biofeedback. Now that we've talked about some of the predominant time-domain indices, let's move towards frequency domains as these have become quite popular in recent years. Let's first differentiate between time domain and frequency domain measurements of HRV. As a recap, when we think about time-domain indices, this quantifies the total amount of heart rate variability. Whereas frequency domain measurements will quantify the distribution of absolute or relative power into different frequency bands. Absolute power can be expressed in terms of millisecond square divided by cycles per second, and relative power is expressed as the percentage of total HRV, or we refer to this as normal units. In frequency domain HRV measurement, power is expressed in normal units by dividing the absolute power for specific frequency band by the sum absolute power of the low-frequency and high-frequency bands. When we calculate power in normal units, this will also allow us to directly compare the spectral distribution of HRV bands for two different people. Now, all of this is referring to the algorithms that constitute frequency domains or power. But for the sake of our discussion, I want to see if I can now simplify all of this crazy complex information. Let's think about an EEG. So, this actually measures individual brainwave domains. For instance, when we have the slowest brainwave, which is associated with sleep, this is called delta waves. The next band or wave band would be theta, then alpha, and then beta. This is an example of how the process of something called a power spectral analysis can separate brainwaves into their own component rhythms that operate within different frequency ranges. We can do the same actual thing–we can do the same thing, I should say, with HRV. A great way to think about this is to think about shining a light through a prism. The prism will reflect white light into its component wavelengths. So, through a mathematical process called the fast fourier power spectral analysis, we can break HRV when at time domain into its component wavelengths. And into each of these wavelengths, we can give a little bit more insight into our autonomic functioning. Before I begin talking about each of these wavelengths or frequency domains, I want to know that there is still some controversy regarding the autonomic contributions to some of these domains since these measurements will kind of profoundly vary with testing conditions. One thing to note about HRV frequency bands similar to that of EEG bands is that we are predominantly concerned with the dominant band at the time of assessment. This is because we have activations of all bands at any given time, but we are concerned with what is mostly activated or is considered the dominant domain. Think about EEG again. If you are to hook yourself up to an EEG, you might have one band that is more dominant than the others. So, say, for instance, theta, but this does not mean that you are producing zero delta, zero alpha, or zero beta. Indeed, you are making all of them at once, but one may be more predominant as a wavelength at that time. It's a common mistake for many individuals to believe that we are only making one set of brainwave frequencies within the area of the brain that we are studying. So, I hope that this helps to clarify that just because–like the brain, the heart is not simply making one frequency to the void of others. Yes, it may be presenting with one dominant frequency, but we are still able to measure all of the others as activated during this period. With all that said, there's still a lot of great data that we have gotten from studying frequency domains that I believe are very important for us to cover. We'll start off with the ultra-low-frequency band, which are oscillations less than 0.003 Hertz. This is a frequency band that can be only measured within a 24-hour period. For this band, there is no consensus regarding the mechanisms that generate its power, but we do know that it is indicative of very slow-acting biological processes. Some researchers believe that circadian rhythms may be the primary driver of the ultra-low-frequency band. There's also belief that core body temperature, metabolism, and other bodily systems over a long period of time may contribute to this frequency. There is also disagreement about what branch of the nervous system contributes to the ultra-low-frequency band. So, for the sake of our discussion, until we learn more about this unique frequency band, there's not much more that I want to say about its utilization. So, now, we move to the very low-frequency band, which is the frequency band that ranges from 0.003 Hertz to 0.04 Hertz. In order to record the very low-frequency band, we must record at least five minutes' worth of data. But 24 hours is actually considered the gold standard. Through research, we know that any low values on a 24 clinical HRV recording can predict greater risk or adverse outcomes. However, what we have found that is the very low power frequency is more strongly associated with all-cause mortality than the low-frequency or high-frequency domains. Therefore, as we gain more research on this band, we are finding that the very low-frequency bands may be quite fundamental to health. When researchers have studied very low-frequency bands, band power, they have found that low power in this domain has been associated with rhythmic death, high levels of inflammation, and lower levels of testosterone. They've also found that parasympathetic nervous system activity may contribute to very low-frequency band power since parasympathetic blockade almost completely abolishes it. When researchers have blockaded the sympathetic nervous system, this does not appear to affect the very low-frequency power. So, from a practical standpoint, especially when measuring over 24 hours, this is not a band of the frequency domains that we want to have low. This brings us to some of the more well-known frequency bands. And the first one I want to discuss is the low-frequency band, which ranges from 0.04 Hertz all the way up to 0.15 Hertz. This band requires a minimum recording of two minutes, while this is one of the more commonly used in many phone-based applications and biohacking wearables. Interestingly enough, there is actually disagreement regarding the sources of activity within this band. Formally, this region or frequency band was called the baroreceptor range because it does mainly reflect baroreceptor activity under resting conditions. It appears that low-frequency band power may be produced from both the parasympathetic and sympathetic nervous system and is regulated via the baroreceptors that regulate blood pressure. One of the things that we know about the low-frequency band is that the sympathetic nervous system does not appear to produce rhythms much above 0.1 Hertz, while the parasympathetic nervous system can be observed to affect heart rhythms down to 0.05 Hertz. When we engage in slow respiration rates and slow breathing, vagal activity can easily generate oscillations within the low-frequency band. This is why you hear a lot of individuals say, “To train within the low-frequency band.” Indeed, this can actually be quite simple for most individuals. Breathing at a rate of six breaths per minute has been found to put most people within this low-frequency domain. We might even say that this domain can be representative of autonomic balance. There's a process of breathing, which we call resonance frequency, which is a common biofeedback tool that places the individual within this range. This is something that I'm going to talk about in a little bit when I get into common modalities for enhancing HRV. But for now, know that this is a common range to train autonomic balance in vagal tone. Within the Institute of HeartMath, they actually have identified the single high amplitude peak within this low-frequency domain, and more specifically, at the 0.1 Hertz mark to indicate what they call a state of high coherence. From this model standpoint, coherence is when the heart, mind, and emotions are energetically in alignment and in cooperation. They've identified coherence as when we increase synchronization and harmony between the cognitive emotional and physiological symptoms, which results in efficacious or efficient and harmonious functioning. The idea of the HeartMath Institute and their wearable technology such as their emWave2 and the Inner Balance is to increase heart rate variability and coherence through paced breathing and visualization. The last frequency band and domain that I want to discuss today is the high-frequency band. This is found between the 0.15 to 0.40 Hertz and requires a recording of at least one minute. The high-frequency band can reflect parasympathetic activity, and we also refer to this as the respiratory band because it corresponds to the heart rate variations related to the respiratory cycle. As you may recall, these phasic heart rate changes are known as RSA and may be a pure index of cardiac vagal control. What I should say too, when you inhale, the heart rate is going to accelerate, when you exhale, the heart rate is going to slow. So, when we inhale, our cardiovascular centers will inhibit vagal outflow resulting in the speeding of the heart. And when we exhale, this will restore the vagal outflow and slow the heart due to the release of acetylcholine. When there is total vagal blockage, this will virtually eliminate all of the oscillations found in the high-frequency band and will reduce the power range and the low-frequency band. We see a high correlation between the high-frequency band and the RMSSD time-domain band. When individuals have high-frequency band power, it's correlated with an increase in stress, in panic, in anxiety, and in worry. And it's still important for us to remember that high-frequency power and RSA does not represent vagal tone. Keep in mind that high-frequency power and RSA is very easy for us to manipulate by slowing our respiration rates. A study done in 2017 demonstrated that if you slow your breathing to six breaths per minute, you should observe increased heart rate fluctuations compared with 15 breaths per minute, which is the average human breath rate. It is during this time that the mean heart rate should not appreciably change because vagal tone did not decrease. This is an example of how high-frequency power can index vagal modulation of our heart rate, but it does not represent vagal tone. Another common index for frequency-domain measurement and power is something called the low-frequency to high-frequency ratio. The intent here is to estimate the ratio between sympathetic nervous system and parasympathetic nervous system activity. This measurement is seen typically in wearables like the Polar chest strap and the Elite HRV app. The assumption here for the low-frequency to high-frequency ratio is that low-frequency power may be generated by the parasympathetic nervous system, sympathetic nervous system, and baroreflex mechanisms while the high-power band is produced by the parasympathetic nervous system. So, in this model, a low, low-frequency to high-frequency ratio will reflect parasympathetic dominance. This might be seen when we conserve energy and engage in the tend-and-befriend behaviors. You might consider yourself to have low autonomic arousal and be quite relaxed when this ratio is low. So, to contrast this, when we have a low-frequency to high-frequency ratio, this may indicate sympathetic dominance, which occurs when we engage in the fight-or-flight behaviors or form of parasympathetic withdrawal. One thing to keep in mind about this from a research perspective is that brief recordings of the low-frequency to high-frequency ratio are a little controversial as short-term measurements tend to be poorly correlated with 24-hour values. So, it's in my opinion that examining the research that a five-minute resting baseline of the low-frequency to high-frequency ratio may not be our best estimate of autonomic balance. So, with all of this information on the different frequency bands, how might I use them both personally and clinically? Well, first, you must assess your intent on measuring the frequency domains. So, for instance, am I doing more meditative or resonance frequency training to, in a sense, manipulate HRV so that I can experience an increase in vagal tone or relaxation response? Or am I using it for examining recovery? Depending on my needs for the assessment, I may be examining these numbers from different lenses. Let's take the first example and break it down. Again, I'm going to talk about the concept of resonance frequency training in a few minutes, but if I were utilizing heart rate variability for relaxation, reducing distress, or a way to enhance meditative practices, I would be looking to increase the low-frequency band and integrate what we refer to as coherence. Increased low-frequency band will indicate enhanced vagal activity and activation of the parasympathetic nervous system and autonomic balance. Whereas I would not want to manipulate breathing and respiration such as breathing at my resonance frequency rate if I were assessing overall recovery. This is because manipulating breath rate will almost certainly change your HRV scores. One of the things that I'm most consistently asked about are norms. So, it makes sense to ask this question as we want to be able to provide a basis for comparison for HRV numbers. If you look at any website where there is HRV discussion, there are always individuals posting their HRV data and asking, is this low? Is this normal? and so forth. I want to be able to answer some of these questions here, but please know that we never utilize HRV scores as a means to diagnose. Also, as you have also inferred, HRV changes quite frequently and should not be a metric that you take once and then try to make any type of conclusion. Also, like many other biometrics that we quantify, HRV is one that it's great to have a consistent baseline and then work on training that number in an upward direction. Well, many questions come my way regarding low HRV. I'm also asked questions about high HRV and whether or not this can be problematic, and I'm going to speak about this as well. But let's turn to HRV norms to see if I can dispel some myths and highlight some potential goals. I've already mentioned before that when looking at the marker that is considered the gold standard, which is SDNN, from a cardiac functioning standpoint, we see that happening with a 24-hour recording. Those with less than 50 milliseconds of HRV are considered unhealthy, and those with an HRV from 50 to 100 milliseconds are considered to have compromised health, while those with HRV over 100 milliseconds are considered healthy from a cardiac standpoint. A couple of things on this. First, please remember that these are just standards for cardiac outcomes and are not made to be used from a diagnostic standpoint. There are plenty of other pieces of information that we need in order to notate whether someone has a healthy cardiovascular system or an unhealthy one, not just HRV alone. While this is the gold standard metric, we are all about integrating data. So, second, if you already heard me mention these numbers and you're freaking out because your Oura ring is telling you that you're in the 30s or 20s, you're actually freaking out for no reason. The Oura ring uses the RMSSD data and not SDNN. Lastly, I don't know many individuals who are recording 24 hours with the SDNN marker other than those who are wearing like Holter monitors for a long period of time. So, from a quantification standpoint such as the utilization of wearables, many of us are just really not collecting this data. And this is predominantly clinical. So, I just wanted to provide these numbers initially, as again these numbers are the gold standard for cardiovascular outcomes. Well, there are many different types of time-domain measurements that we mentioned before like the SDNN and SDRR and RMSSD. There are also other ones like the SDANN index. There's the NN50, the PNN50 and so on. But these are not typically ones that you're going to cross paths with unless you're doing clinical biofeedback with a specialist like myself. A majority of these wearables or technology that you would utilize from a consumer standpoint are either going to be via SDNN or RMSSD. That is why I'm going to devote much more time to these. There have been numerous studies looking at identifying norms, but the largest study ever done on normalizing data was done compiling 44 selected studies, which examined over 21,000 adult participants. Some things to keep in mind. First, this analysis included three large populations with a minimum age of 40, which may actually end up explaining their comparatively low HRV scores and can't be generalized to yourself if you're under 40. Well, yeah, because that's the minimum age. And they also didn't factor in other types of variables, things like age, gender, socioeconomic status, and so forth. But here is what they found. The researchers of this large comparative study found the average mean SDNN score in milliseconds to be 50 milliseconds with a standard deviation of 16. They found the average RMSSD to be 42 milliseconds with an average standard deviation of 15. They found the low-frequency to high-frequency ratio in terms of millisecond squared to be 2.8 with a standard deviation of 2.6. Another interesting study that was done in 2015 looked at 2,000 subjects between the ages of 25 to 74. Now, these were noted as healthy adults as they included anyone with cardiac arrhythmia, diseases, those who were on significant medications or pregnant. However, I tend to utilize this information as a basis for my own norm charting. I want to break it down in terms of age and gender and look at two distinctive time domains, both SDNN and RMSSD. I'm about to spit out a lot of data, so just bear with me and make sure that you listen for your own age norms. So, let's start with ages 25 to 34. The study found that males in this age range had an average RMSSD of 39.7 milliseconds with a standard deviation of 19.9 milliseconds, and in SDNN of 50 milliseconds with a standard deviation of 20.9 milliseconds, they found that women had an average RMSSD of 42.9 milliseconds with a standard deviation of 22.8 milliseconds, and a standard deviation, or I should say SDNN, of 48.7 milliseconds with a standard deviation of 19.0 milliseconds. In examining men and women in the age category of 35 to 44, they found that men had an average RMSSD of 32.0 milliseconds with a standard deviation of 16.5 milliseconds, and an SDNN of 14–sorry, 44.6 milliseconds with a standard deviation of 16.8 milliseconds. They found that women in this age category had a standard deviation–sorry, an RMSSD of 35.4 milliseconds with a standard deviation of 18.5 milliseconds and an SDNN of 44.5 milliseconds with a standard deviation of 20.5 milliseconds. In examining the age category of those 45 to 54, they found that men in this age category had an average RMSSD of 23.0 milliseconds with a standard deviation of 10.9 milliseconds and an SDNN of 36.8 milliseconds with a standard deviation of 14.6 milliseconds. They found women in this category to have an average RMSSD of 26.3 milliseconds with a standard deviation of 13.6 milliseconds and an SDNN of 36.9 milliseconds with a standard deviation of 13.8 milliseconds. The next category were males and females ranging from 55 to 64 years of age. For males in this category, they found an average RMSSD of 19.9 milliseconds with the standard deviation of 11.1 milliseconds and an SDNN of 32.8 milliseconds with a standard deviation of 14.7 milliseconds. For women in this category, they found an average RMSSD of 21.4 milliseconds with an average standard deviation of 11.9 milliseconds and an SDNN of 30.6 milliseconds with a standard deviation of 12.4 milliseconds. Lastly, in the oldest category that they studied, which were those aged 65 to 74, they found that males in this age category had an RMSSD of 19.1 milliseconds with a standard deviation of 10.7 seconds and a standard deviation or SDNN of 29.6 milliseconds with a standard deviation of 13.2 milliseconds. Lastly, they found that women in this age category had an RMSSD of 19.1 milliseconds and a standard deviation of 11.8 milliseconds and an SDNN of 27.8 milliseconds with a standard deviation of 11.8 milliseconds. So, wow, there is a lot of information. I hope that this puts some people at ease as I get questions all the time about Oura ring measurements and whether they are too high or too low. And now, I highly encourage you to check out these numbers again if you have questions about how you compare with those within your age category and for your gender as well. What is great about the studies is that they do also show comparisons in the low-frequency and high-frequency bands, and then the low-frequency and the high-frequency ratio. This was a study performed by Voss and their colleagues in 2015. The last thing that I want to say about HRV norms, something that I get quite a lot of questions about is in regards to high HRV scores. As I noted before, while it is important to modern HRV from a norm standpoint, it is equally if not more important to self-quantify in an effort to compare HRV scores to yourself. This means establishing a baseline and then making comparisons not just to norms, but making comparisons to your own baseline. Now, the research is not clear on whether or not there's a ceiling to HRV scores. In other words, there's no definitive research to demonstrate that having a high HRV score compared to a low HRV score or compared to the norm has negative effects. However, it has been proposed that individuals with significantly high HIV scores may not be pushing themselves as hard as they could. Again, this is quite a subjective statement, but it is something to note. Some theorize that high HRV scores may be an indication that you could push yourself a little bit harder on your workouts, and I'm not sure I quite buy into this, but it's worth further exploring. My opinion in conclusion though is I would still, even from a personal standpoint and clinical standpoint, would like to see higher HRVs when compared to lower HRV scores. The only time that a high HRV score can be extremely problematic is if we find there is arrhythmia or some other cardiovascular problem that is contributing to long durations of time between the heartbeats. So, for example, if someone is having some arrhythmic heartbeats, they may end up skipping beats, which will result in what looks like an elevated HRV when in fact, this is more representative of dysfunction and a disorder. So, in instances like this, a high HRV can be problematic. Normally, with arrhythmias, there are going to be additional symptoms that the individual is experiencing that would warrant a stress test or an echocardiogram to determine dysfunction. So, now that we've taken a deep dive into the HRV metrics and norms, I think that it's time for us to discuss specific techniques and tactics for HRV training. I like to split this into two sections. First would be specific HRV biofeedback techniques, and the second would be HRV hacks. Some people believe that the most important metric to change is their resting HRV score, which what I would argue is highly important. But something that I would argue that is much more important than your resting HRV would be your ability to quickly and efficiently tap into your parasympathetic response. The ability to modulate HRV quickly holds substantial benefits for the individual, especially when compared to resting HRV. Well, resting HRV can be a great representation of overall health, recovery, and well-being. I'm not nearly as concerned with making substantial changes in that area as I am with parasympathetic efficiency. One thing I must say, and honestly, there is no easy way around this, in order to truly know what changes are taking place from an HRV perspective, you need to be quantifying it with some form of wearable or device. However, all the techniques that I'm going to share with you do not require HRV measuring devices in order for them to be effective. The greatest thing about biofeedback is that it's not a piece of equipment that is the change agent. Indeed, the change agent is inherently in the ways that we change our physiology. I think that it's important for us to remember this because we get so caught up in all these really cool and expensive biohacking wearables, but in the end, this is just information and not the mediator of change itself. So, if you have some expendable income, I'm going to talk about a few devices that I really like and how I utilize them practically. Many of these are fairly reasonable in price. I don't expect you to go out and buy a $15,000 piece of biofeedback equipment as this is something I would use like clinically. So, you wouldn't want to go out and do that for yourself necessarily. You would have no clue what you're doing unless you had that training. What I use on a day-to-day basis for my own personal HRV training are much less expensive devices, though I must say it is really nice to have the ability to practice on clinical biofeedback whenever I want. But trying to carry around all that equipment is a bit of a hassle when I can just throw on my Oura ring. So, the first tactic to HRV training and HRV biofeedback that I want to discuss is what I considered the most important or something that I believe each and every person who is doing HRV training should learn. And this is something called resonance frequency training, which is an assessment tool and technique created by Paul Lehrer. This entails you determining the exact resonance frequency of your cardiovascular system. This frequency is a manipulation of your respiration rate, which has a significant impact like we talked earlier on your heart rate due to the stimulation of the baroreflex. At this respiration rate, there is significant effects due to maximized respiratory sinus arrhythmia and baroreflex gain. The idea behind resonance frequency training is to breathe at a rate that causes the heart rate to go up and down in phase with your own respiration rate. At this rate, respiratory gas exchange is efficiently maximized. And what researchers have determined is that when you engage in regular practice of resonance frequency techniques, it has been shown to provide clinically significant improvements in a variety of symptoms and disorders such as chronic pain, asthma, depression, COPD, food cravings, and hypertension, just to name a few. What Dr. Paul Lehrer and his colleagues found is that when a person breathes at their resonance frequency rate, which is typically between four and a half and six and a half breaths per minute, the cardiovascular system will resonate, much like the sound of a vibrating string in a box above the violin, creating this big reverberating sound. Again, when breathing at this resonance frequency rate, the baroreflex system is stimulated and strengthened. Again, this is that blood control and emotional regulation control mechanism. And we find this to be at its most efficient rate when we're breathing at the resonance frequency rate. Remember too, when our blood pressure goes up, the baroreflex causes the heart rate to go down. And this is what causes that rhythm and that heart rate fluctuation. From a clinical standpoint, there are a couple of things that we are looking at in assessing resonance frequency. First, we are looking at something called phase convergence with breathing. And what this means is that we want to see that the heart rate and respiration rate are in phase or in agreement with one another. Basically, do the lines trace the same pattern? Where you start breathing, the heart rate follows the breath all the way to the peak, and as you exhale, the heart rate should decline with this line pattern. The next thing is looking at heart rate amplitude. We're going to choose the resonance frequency rate that has the highest amplitude to remind you is the highest heart rate minus the lowest heart rate within a respiratory cycle. Then we want to see which breath rate maximizes the low-frequency amplitude peak. Basically, which breath rate has the most power in the low-frequency domain? Given all these factors, we then calculate our own resonance frequency. Now, you are only going to really be able to do this if you have a more advanced HRV measuring device, such as a Polar chest strap with the Elite HRV or clinical biofeedback. The most accurate results are going to be by going to see a biofeedback practitioner. The good thing though is that we know through research that we all have, probably all have a resonance frequency in between four and a half to six and a half breaths per minute. As a safe bet, I will typically tell people to breathe at around six breaths per minute if they do not have access to this testing metric. Research has indicated that this is the strongest way to coach and train vagal tone and increase HRV. The idea behind this is that the more frequently we train using our resonance frequency training, the more easily we can tap into the low-frequency band. Something interesting about this type of training is that elite athletes have utilized this in order to get into the zone before a serve, like in tennis, or before a golf swing, or before a pitch is thrown in Major League Baseball. If we train the style of breathing and pace of our breathing on a daily basis, our body is going to most easily adapt and we are going to be able to tap into the state and maximize HRV within two to three breaths. Again like anything, this is going to take consistent practice. I might also mention that there are a few ways to practice this style of breathing. Of course we need to be able to pace our breathing, but also there are some suggestions on how we breathe mechanically. First is for us to exercise a diaphragmatic breath. This is where we inhale through our nose and allow our lungs and stomach to expand so that it can push the diaphragm towards the pelvic floor. I like to use some visual imagery to demonstrate this. When we inhale, I want you to think of your lungs and stomach like operating like a balloon would. As you bring air in through your inhalation, you will imagine that you are filling the balloon with air, allowing it to expand to about 80%. Don't overinflate the balloon. Once you're at this point, you will then exhale slowly and quietly and deflate the balloon. Sometimes I like to think about myself gently pulling my belly button towards my spine. I'm not tugging or trying to allow the air to be pushed out, I want to allow this to feel as effortlessly as possible. When this occurs, we are able to stimulate the vagus nerve that innervates the posterior section of your lungs. This will also help to maximize respiratory gas exchange for an increased oxygen and nutrient delivery. Then depending on who you ask, you can either exhale through pursed lips like you're blowing through a straw, or you can simply just breathe back through your nose. That's typically my suggestion. It's imperative to breathe or inhale through your nose as this will actually maximize nitric oxide delivery and vasodilation, which are very important in increasing HRV. One of the biggest training tools that I will use and that I find to be best is to breathe as quietly and as gently as you can. I do not want to try to see, or I should say–yeah, I do not want to try to see if I can inhale as much air as I can as possible. I will actually want to just focus more on the slow quiet diaphragmatic breaths. And sometimes I'll even create what feels more like a hypoxic environment in my body. And this is similar to the work of Patrick McKeown, who wrote “The Oxygen Advantage.” If you're breathing this way and training this way, the research suggests that you need to perform this for about 20 minutes two times a day. And I like to utilize this strategy when I'm engaging in meditation or just as a separate health strategy. So, that's resonant frequency training. Now, of course, there are many other breathwork techniques that you can utilize, but I found this one to be quite effective both personally and clinically. The key features to this style of breathing is to remember to breathe low, to breathe slow, and to breathe quietly. Again Patrick McKeown, who, like I mentioned earlier, the author of “The Oxygen Advantage,” recommends to breathe so quietly as if you are not trying to move any hairs within your nostrils. So, have that visualization as you take a breath in. Another way to maximize HRV is through the process of meditation. Indeed, numerous research studies have indicated that engaging in different meditative techniques such as visualization or guided imagery meditation and mindfulness meditation can significantly improve overall HRV. This is likely due to the fact in correlation of slow respiratory patterns when engaging in these exercises. But also that mediation, or meditation I should say, brings about a sense of calm and safety, which is likely due to vagal tone or vagal nerve stimulation. I tend to like to pair breathwork in meditation as I'm always looking to maximize efficiency and time in my day. These techniques, when I combine them with my utilization of biofeedback wearables, has been found to be the most effective way for me to enhance HRV. If you're looking in the wearables and self-quantification scene, you likely already know of many wearables for determining HRV. I have found some to be really good and I have found some that have left me quite disappointed. I like checking HRV in different ways. So, first, I like checking the resting or that static HRV state. This is going to give me an HRV that is not manipulated by respiration and is a better representation of my overall nervous system recovery. Remember, it's actually quite easily–or I should say it's actually quite easy to manipulate HRV via breathing slowly and diaphragmatically. As such, I do like to measure HRV when I don't have the opportunity to manipulate the results, and the perfect place and time for that is sleep. Now, I know that I've already mentioned the use of my Oura ring, which I found to be one of the most accurate ways to measure HRV non-invasively. There are also other devices such as the WHOOP band and the Biostrap that can provide accurate results. I tend to like something that's a little less invasive physically such as a ring over a wrist strap. However, you need to go with your own preference. Also, whatever device that you end up getting, you need to make sure that you're basing your norms on the metrics of the device that you're using. For instance, if you use your Apple watch, which Apple watch does calculate HRV, their measurement is SDNN, while the Oura ring uses the RMSSD metric. So, each morning, I take off my ring and then put it on the charger to get it off airplane mode, and I'll check a few metrics in regard to sleep. I'll look at body temperature and then I'll look at heart rate variability. I'll always look at my HRV numbers in comparison to both my own, as well as the normative population. The great thing about self-quantification is that we can establish a baseline for ourselves and then make general comparisons to that baseline. While it's important for you to compare yourself to norms, it is equally, or maybe more important for you to have a baseline comparison for yourself. I utilize this number for my ring to give me a good representation as to my overall level of recovery. Your nervous system is not going to lie. If your HRV is significant low, say one to two standard deviations below your average, then that may give you the information about whether or not you should train that day or how hard you should train. Let me give you a personal example of how I've utilized this. I typically play tennis two to three days a week. My average ring score is about 110 to 115 milliseconds. If my HRV score the following morning is 80 or below, I will typically take it a little bit easier on physical exertion that day. Interestingly enough, our autonomic nervous system recovers fairly quickly, but research has also indicated that HRV can be a great measurement of recovery in order to prevent injury or re-injury. I have used this as a reliable means to avoid injury. And I've also found that when I have overreached or overtrained and my HRV measurements told me I was already doing that, then this has resulted in me engaging in more injury or being more prone to injury. One thing to also keep in mind is that decreased HRV is highly associated and correlated with increased heart rate. For instance, we know that a heavy night of drinking alcohol can cause the heart rate to go up. And in turn, this will end up resulting in a decreased HRV. So, if you notice that your HRV is significantly lower on nights that you consumed alcohol, that is why. Now, if I'm doing more HIV biofeedback training and to increase my HRV from an emotional or psychological or stress-based standpoint, then there are numerous devices that you can use for feedback for, in the moment, HRV scores. Some popular ones include the emWave2 and Inner Balance by the HeartMath Institute. And as I indicated earlier, the intent behind these devices from HeartMath is increased coherence, which is very similarly associated to resonance frequency. Both of these devices utilize PPG or photoplethysmography, which I mentioned earlier, and our devices that typically go on the ear lobe or on the finger and look at overall blood volume fluctuations through infrared lights that shine through the muscular tissue. This is a great and accurate means of measurement, as well as easy and efficient to determine HRV. The only way, or I should say the other way is through ECG or electrocardiogram, which is a little more complicated, but in my opinion, is the most reliable due to the minimization of artifact. You can use these devices to help coach you in different breathing techniques and meditative techniques to increase HRV. You can see HRV waveforms begin to establish after just a few minutes of breathing in a coached pattern. And what's going on here is a strengthening of your overall autonomic nervous system, an enhancement in autonomic balance and vagal stimulation that is increasing acetylcholine production that helps to regulate the speed of your heart. Most people will say that they feel the effects of this HRV training within a matter of minutes. And because I've trained on these types of devices for so long, I can enhance my own HRV within a matter of about two or three breaths, and this demonstrates strong and specific and efficient control of my autonomic nervous system, something that you can do as well with training. And I like these devices because they are very accurate and user-friendly. There are other training devices such as the Biostrap and WHOOP that can be paired with their own app. But there are also devices that I found to be the most accurate and effective devices for HRV biofeedback. One of them is the highly popular and well-known Elite HRV app and the Polar chest strap. This isn't actually an ECG device that instead of measuring the blood flow and the blood volume pulse, such as the devices I mentioned earlier, this will actually measure the electrical output of the heart. Now, these are a little bit more invasive, something that you can clip on your finger or your ear, but I like them because their accuracy and ability to reduce artifacts, and as you remember, artifacts are like those false beats. Many of the wearables do not remove false beats, which can lead to very inaccurate data. The Polar H7 chest strap with either the NatureBeat or the Elite HRV app is a great way to go, but I actually have one app or one device that is not as well-known, but I've found it to be without a doubt my favorite device that I've ever worn for heart rate variability training. The device that I'm talking about is by a company called Lief Therapeutics, L-I-E-F Therapeutics. This is a wearable ECG device that attaches to two separate electrodes and is placed right below the left chest, similar to the position where you would place a full ECG. This device is very lightweight and will track HRV throughout the day. The great thing about this device is that it will help you to establish your own baseline, and then throughout the day, it will detect when your HRV has fallen significantly below your baseline. You will then receive haptic vibrating feedback in a vibrating pattern to let you know that your HRV is low. And once you fill this haptic feedback, it will then provide you with different vibrating patterns consistent with whatever breathing pattern you have indicated to the app that is your preferred respiratory rate. So, for instance, in my resonant frequency, it's five breaths per minute, which might actually is. On the phone application, I can tell it that when my HRV has fallen significantly lower than my baseline, to start a breathing pattern at that rate. There will then be two distinct feedbacks from the haptic engine that I will experience at this time. When there is no vibration on the device, this is telling me to start my inhalation. When the device begins to vibrate, I will exhale until the vibration is complete. I will do this until I've gotten my HRV back up to baseline. After a period of time wearing the Lief device, I have found that I am able to increase my level of self-awareness and also my ability to more quickly regulate myself HRV that I have seen kind of multiple benefits with this thing. This is so much so that I'm able to pinpoint now when my advice will begin to vibrate even before it begins vibrating. My level of self-awareness regarding my stress response in HRV has become so heightened due to this device that I don't even need it anymore, but I still use it because–well, I've found that it's just the best HRV biofeedback device I've ever used. The application also has multiple guided meditations, abilities to track HRV on a daily and weekly basis, the ability to train with paced breathing, the ability to feel your own heartbeat from the haptic feedback engine and much more. You can find more about this company if you go to getlief.com, L-I-E-F. But I cannot stress how much I've used this device and found benefit, as well as how many of my patients have utilized this device and found significant benefit as well. This is the device that I have all of my personal clients buy for coaching and the one that I personally use. My last comment on HRV wearables is to gain–or I should say to again remind you to be aware of the potential inclusion of artifact data. This is something that can significantly skew your results and should be assessed and taken into consideration before assessing HRV. One way to help mitigate the effects of artifact collection is to make sure that you are sitting at a table or sitting in a stable position and that you are just completely still during readings, especially during short-term readings. I generally also check my HRV at the same time each day, and even in the same place each day to get readings that are as reliable and as consistent as possible. There are plenty of other ways to increase your overall HRV. One of the ways that I have found to be the most effective increasing the resting HRV is through the use of cold exposure. So, cold exposure, as many of you know, is a hormetic stressor that results in acute sympathetic state arousal. As such, this is the perfect time for us to induce a parasympathetic state during the cold exposure and during cold recovery. What you may notice initially is a significant decrease in HRV immediately following the cold exposure, and this of course is common. However, because our body wants to reenter a state of homeostasis, the reparative process will result in higher HRV. I have found that through the use of either cold plunges or hot to cold contrast showers, I've been able to modulate my HRV pretty significantly with these techniques. I also like the idea of cold exposure at night. So, quality sleep is also a way to increase HRV. And tracking HRV alongside sleep is a valuable system of this quantification. What you will find is that the lower your heart rate goes due to more deep and restorative sleep, the higher your HRV will be. And as I mentioned before, one of the things that helps me sleep immensely from a recovery standpoint and overall quality of sleep standpoint is by using a mechanism to cool my bed, such as the Ooler system or the chiliPAD. I've noticed significant enhancements in overall HRV when cooling my core temperature down with a cold shower as well before bed, and then I use the chiliPAD system at night when I sleep. Hands-down, the most robust research for increasing overall HRV aside from HRV biofeedback for stress reduction is physical exercise. Now, given this audience, I know I do not need to go into the benefits of exercise, but many research studies have looked at how exercise can enhance each HRV both from a cardiac standpoint and from an autonomic balance standpoint. If you haven't already gathered, we have to remember that there is a dose-response curve with exercise. As Ben always says, we're looking for the minimal effective dose of exercise, and this is true for exercise effects on HRV. We indeed know that if we continually and consistently overtrain, this is going to lead to increased chance for injury and has a highly predictable correlation with low HRV. We can use both a low HRV to demonstrate overall recovery or lack thereof, but we also know that continued overtraining will result in the continued lowering of HRV. For instance, in one study looking at the effects of moderate exercise versus heavy endurance exercise on nocturnal HRV, that's the resting HRV, researchers found that heavy endurance athletes such as marathon runners had significant low-frequency power during heavy training and after a marathon. In this study, we actually see decreased HRV during the nocturnal hours after both moderate exercise and marathon completion. But we see statistically significant reductions in HRV for those who are engaging in heavy endurance exercise when compared to those engaging in moderate exercise. This isn't surprising that we would see a reduction in HRV for those engaging in moderate exercise, but it does go to show that there is significant HRV reduction after heavy or intense exercising. One strategy that I utilize personally is the uses of HIIT training or high-intensity interval training and Tabata sets. Because these are types of workouts that are more effective in stimulating our body's need to adapt, they can also increase HRV in the long run. Now, as a general rule of thumb, if my HRV is significantly lower on the day, I will never utilize this type of training. I will almost always avoid doing so in an effort to avoid overtaxing my nervous system. When they examined the usage of high-intensity interval training, this is researchers, versus moderate intensity continuous training on HRV, the individuals–I should say individuals who are considered physically inactive, they found that HIIT training was significantly superior to moderate intensity continuous training and improving HRV. One study that really stood out to me was examining the effects of physical exercise on HRV in patients with cancer diagnosis. They found that these individuals with cancer diagnosis that engaged in exercise actually enhance their overall HRV and cardiac autonomic regulation. And it was concluded that because of the association of higher HRV parameters and prolonged survival in cancer patients, exercise to increase HRV in these individuals can be a highly effective treatment strategy. So, it's my guess that we're going to see more studies on the efficacy of exercise on HRV as time goes by. Another tactic that I utilize on a daily basis for increasing HRV is compassion and meditative practices. So, numerous studies have indicated that engaging in a meditation practice can increase HRV by reducing the fight-or-flight response and increasing our safety response. I found this as a highly useful strategy for myself and for my patients and have seen demonstrable effects for increasing HRV with this type of practice. One study examined the use of gratitude journaling on HRV and other inflammatory biomarkers and individuals with heart failure. They found that these individuals that participated in gratitude interventions had reduced inflammatory biomarkers and increased parasympathetic HRV responses when they were engaging in the gratitude task. While the results did not indicate a significant difference in HRV after journaling, there were notable benefits during the time of journaling. And inflammation biomarkers were significantly changed and maintained after intervention, which is really cool. This is why I believe that it's important for us to engage in mindfulness-based exercises and gratitude exercises each and every day as this can have valuable benefits to our sense of safety and well-being. The last thing that I will say that this could be a podcast in and of itself is that there are plenty of dietary considerations. Now, I could get into one diet over the other, whether it's carnivore versus omnivorous diet on HRV. And there's really not a lot of great data to support one or the other specifically for HRV. However, we do know that a whole foods anti-inflammatory dietary pattern is going to be significant benefit on HRV when compared to the standard American diet. As we know, there is a significant reduction in inflammatory markers and stress that can significantly enhance HRV. So, the takeaway from this, which you may already know, is to find what dietary patterns work best for you and watch HRV scores as you manipulate what you're eating. One thing to note about fasting, as many individuals ask about what fasting does to HRV, interestingly enough, we have data to demonstrate that short-term fast or time-restricted eating can significantly enhance HRV in the long run. However, do not be surprised if you see significant reductions in HRV when you are engaging in an extended fast. You have to remember, a fast is a form of hormetic stress, and therefore, in the temporary, can reduce HRV scores. However, as the body repairs and returns to homeostasis, we tend to see HRV increase. In the end, if we break HRV optimization down in its most simplistic form, we are truly looking to tell our brain in our body that we are safe. One of the most famous researchers on HRV modulation is Dr. Stephen Porges that I mentioned earlier, who created “The Polyvagal Theory.” In this theory, Dr. Porges proposes competing roles for the unmyelinated fibers in the vagus nerve and the newly more evolved myelinated nerves. Now, he theorized that the evolution of the autonomic nervous system was central to the development of emotional experience and effective processes involved in our social behavior. As human beings, we are not limited to fight, flight, or freezing behavioral responses. We can self-regulate and initiate pro-social behaviors, which may be referred to as those tend-to-befriend behaviors when we do encounter stressors. This is what Dr. Porges calls the social engagement system. And the theory suggests that the system depends on the healthy functioning of the myelinated vagus nerve, which works like that vagal break. From this perspective, we can only activate the myelinated vagus when our nervous system perceives that we are safe. When we engage in social safety, we perceive this as a mutual process, one that involves eye contact, close proximity, and trust. This myelinated vagus enables us to self-regulate, calm ourselves, and inhibits the sympathetic outflow of the heart. The myelinated vagus also allows us to engage the prefrontal cortex and executive functions where we can be attentive and mindful when we encounter daily stressors. This will inhibit the myelinated vagus and produce what is called vagal withdrawal. This will then interfere with our attentiveness and our level of social engagement. According to this theory, quality communication and pro-social behaviors can only be effectively engaged when our defense circuits are inhibited. So, how do we increase HRV in the most consistent and effective manner? We must have a perceived sense of psychological and physiological safety. We are constantly evaluating our environment for threats as a way to maintain our safety both physically and psychologically. When this occurs for days, weeks, years, or decades, this can result in an overarching schema of continued concerns of our lack of safety or lack of trust and others, and ultimately, social disengagement or withdrawal. These isolated behaviors and distortions in our cognition have significant impact on our stress physiology, heart rate variability, and can directly play a role in our perceived sense of meaning and purpose in life. This brings it all together. When our nervous system perceives safety, we activate the myelinated vagus nerve system, and this is a way to conserve and rebuild energy stores to socially bond with others and engage in executive functioning like self-regulation and planning. When our nervous system perceives danger, we activate the sympathetic nervous system and inhibit the unmyelinated vagus resulting in the fight, flight response or active avoidance. If we perceive that our life is at threat and that the fight, flight, or active avoidance response system will not succeed, then we'll actually activate our unmyelinated vagus, which will result in passive avoidance through behaviors like immobilization, feigning death, fainting or shutting down completely. This threat to our survival is what Dr. Stephen Porges believes activates the unmyelinated vagus and results and subsequent disorders like PTSD. This again is why safety security and trust is needed to maximize health outcomes from a mind, body, and spiritual perspective. So, there you go. Man, we have taken a deep dive into all things HRV, but we've only scratched the surface. My hope is that this information was useful and resulted in you learning the ins and outs of why HRV and the self-regulation of HRV is of vast importance for physical and mental health. If this metric of quantification has not been of importance to you in the past, I sure hope that you now see why it should be. In my guess, like anything in the field of science, we're going to learn more and more about this metric and the usefulness of it as we expand the field of research. I hope this podcast has highlighted how important this metric of HRV is and why it should be important for us to consider finding a coach that can help you increase your parasympathetic efficiency quickly, as this is one of the strongest ways to mitigate stress, to improve recovery and enhance performance and longevity. Thank you, Ben, for providing me with your platform to share my passion on heart rate variability and self-regulation. Like I mentioned earlier, you can also find all the shownotes at BenGreenfieldFitness.com/hrvpodcast. And you can check me out at drjaywiles.com, or at my practice which is thrive-wellness.com. Take care, everybody, and have an awesome day." References
Greenfield, B. (2020). [Transcript] - A Deep Dive Into HRV: How To Use Heart Rate Variability To Optimize Your Sleep, Stress, Recovery, Performance, Nervous System Balance & Much More! - Ben Greenfield Fitness - Diet, Fat Loss and Performance Advice. Retrieved 13 March 2020, from https://bengreenfieldfitness.com/transcripts/transcript-what-is-heart-rate-variability/
Hydrogen comes in two “flavors”: regular hydrogen, which is actually called protium, and deuterium. Deuterium has all of the same properties as hydrogen, except that it's twice as big and heavy. This is due to an added neutron paired with the proton in the nucleus. Because of this, deuterium is also referred to as "heavy hydrogen," and it actually behaves quite differently from regular hydrogen in chemical reactions and in our bodies. In nature, deuterium helps things grow. For example, deuterium is biologically necessary for growth in babies, teenagers, and developing plants and animals. But once you stop growing, having too much deuterium in your cells can result in mitochondrial dysfunction and lead to premature aging, metabolic problems, and disease. Deuterium is like thick, gluggy oil - when you put thick oil into an engine, the engine sputters, makes strange noises, and eventually breaks. Nature has put systems in place to deplete deuterium and protect the nanomotors, or "little engines," in our cells’ mitochondria from coming into contact with this thick oil. However, the side effects of a modern life - pollution, global warming, processed foods, less healthy lifestyles, etc. - have resulted in many people having way too much deuterium inside their cells. This results in an inability to effectively deplete deuterium and the destruction of our nanomotors. This starts a vicious cycle of deuterium building up and breaking more of our nanomotors. Fewer nanomotors means less energy and more sickness and disease. While deuterium is a natural and essential element, its presence has increased in the modernized environment within the food, atmosphere, and water. Deuterium levels is food will vary based o where that food is grown - deuterium is highest in the equator and in low elevations. Foods high in fat, as well as green plants, including algae and spirulina, which contain high amounts of chlorophyll, are lower in deuterium than fruits, roots, and underground vegetables. As it turns out, GMO foods tainted with glyphosate, as well as processed, synthetically made foods, possess high amounts of deuterium. There are various lifestyle practices that have led to increased deuterium levels including a lack of sleep, particularly deep REM sleep. In addition, breathing shallow and fast via the mouth and chest also contributes to elevated levels of deuterium. Researchers have demonstrated that elevated of deuterium can contribute to:
Learn More About Deuterium Depletion References Understanding Deuterium - The Center for Deuterium Depletion. (2019). Retrieved 24 December 2019, from https://www.ddcenters.com/about-deuterium-2-2-2/
Dr. Rhonda Patrick discusses the differences between different forms of DHA in terms of bioavailability and transport into different cells. She talks about why a specific type of DHA (DHA in phosphatidylcholine) is more readily transported into the brain because it forms DHA-lysophsophatidylcholine. Krill oil and salmon roe both have a slightly higher concentration of DHA-lysophosphatidylcholine. She also talks about astaxanthin, a carotenoid that is unique to krill oil, and has potent antioxidant activity and prevents the oxidation of DHA and EPA.
Transcript:
"Welcome for everybody. Boy this is a great group. What a great day to be doing something like this. I mean it's raining, right? Okay, so you can't be out in your garden. You can't be doing anything else like that. So how many of you guys have come to one of these events before? Alright, good. So you know that it's a lot of fun and we're gonna be doing a lot of good things. How many have ever heard me speak before? None of you? Wow! Oh a couple down in the front, okay. So if that's the case, then let me tell you a little bit about who I am and what I do. So my name is Dr. Sherry Tenpenny. I am the probably known as the international expert on vaccine injuries and problems associated with vaccines. I've been involved with this for 17 years and about 30,000 hours of my life, in terms of research and speaking and traveling around the world giving talks like this. My first career was as a board-certified emergency physician. I was the director of an ER for 12 years, then I moved to Cleveland, Ohio in 1996 and I opened an integrative medicine practice for which I'm always proud to say we've had people from all 50 states in about 17 foreign countries to come to our clinic to get well and get off their pharmaceutical drugs. So I got involved with this serendipitously, like a lot of things do. I got a notification in the mail in September of 2000 from the National Vaccine Information Center meeting in Washington DC and it was supposed to be in September of that year and it was really inconvenient for me to go. And I actually went so far as to call them and say, "When is your next meeting? Because I don't think I can come this time." And they said, "Well, we're a small nonprofit. We're not sure we're gonna have another one." Okay so every time I went to throw that brochure away off my kitchen counter, it just kind of made its way back onto the kitchen counter. So I was single at the time and I thought oh I know, this is it Lord, this is where I'm supposed to be to meet the guy. So I made it a reservation. I went down to the meeting and it wasn't about the guy. It was about the topic and I sat through four days of non-stop lectures, which I think it was the only conference I've ever been to in my entire life that I sat through all of the lectures and took copious notes and heard researchers and PhDs and doctors and parents talk about vaccines and vaccine injuries. There was about 700 people in that conference. A lot of people that were there with their vaccine injured children in wheelchairs and and I all I could think of as while I was there was, "How did I miss this as part of my education as a physician?" You know, I've been in medicine at that this at that time for 15 years. I was the director of an ER. I gave out tetanus shots like they were some special kind of candy. I was I you know I've had my integrative medicine practice now for almost five years. I grew up in a chiropractic family - three generations of chiropractors. I wasn't vaccinated as a kid. None of my cousins or any of their kids were vaccinated, so it was never on my radar because I had age-appropriate measles mumps rubella, chickenpox and I had pertussis twice, and I'm 59 and here to talk about it. Nobody died. We get so terrorized into these infections, that we need to change the language about that because we call them diseases. And everybody gets all weirded out and scared like somebody's gonna die over these normal childhood infections, that were supposed to come at age appropriate levels, somewhere mostly between the ages of six and nine that left you with a lifetime of immunity. Not only so that you could be healthy as you were went into your 40s, 50s, 60s, 70s and 80s but that you could pass that health on to your children. So that's how I got involved with this. And after that meeting I went home and I started saying "Well, where do you start? Where do I start looking at this? I know! I'll start with the CDC." So I started going to the CDC documents and read the general recommendations of vaccinations - the 1998 version of that, which was such a poorly written paper and such poor documentation. It was a 42 page paper. I still have it by the way. And I thought, this this can't be what this entire industry is built on. This really can't be it. So from there I started reading all of the mainstream medical literature. The Pediatric Infectious Disease Journal, Vaccine, JAMA, New England Journal of Medicine, and it's all in there. The problems associated with vaccines are in the mainstream medical journals. Physicians just choose to flip right by it because it isn't anything they're interested in reading. So that's how I kind of came to this and and each thing that I read it became almost like an addiction because I kept thinking, "I must be missing something. What am I missing? Why can't I find why this is so important?" And the deeper down the rabbit hole I went and the more information that I found, the more shocking it was to me. And I went back to Kathy Williams, who's one of the cofounders of the National Vaccine Information Center, and said, "Surely if people just knew how vile that stuff was that's coming through the vial, they would like stop and run the opposite direction so fast it, they would look like the roadrunner and be gone. We would implode this industry in like a nanosecond." Once people understood that there were cells from aborted fetal tissue, and aluminum, and mercury, and formaldehyde, and stray viruses that can cause cancer in these things they're given to their children. Surely as soon as they know that it will stop. Well, you know, 17 years later we have more vaccines than ever. We have mandates breathing down our neck. We want everybody in the government to take away our rights. So that's why I do this. And that's why, you know, when Patrick heard me talk and I spoke at his meeting last year he said he wanted me to come up and give this information to all of you on this lecture on vaccines 101, because we want to try to boil it down into bite-sized pieces (which by the way they're going to be passing around a clipboard for you guys, if you want to be part of my email list and the information we sent out. Please just put your name and your email in a way that I can actually read it, because it doesn't do any good to write it down if I put an R and it's supposed to be an S into my database.) We're pretty active. My Facebook page has two hundred and seventeen thousand people. We just started a course called mastering vaccine info foundational course and online training. We've got almost a hundred people enrolled in that. It will reopen for enrollment in March if you want to be on the waiting list for that. Just let me know because it goes through everything in a way that's bite-sized pieces about twenty minutes of content, and then the Thursday night Facebook live discussion group to teach you how to take the language in those modules to become a confident parent, an intelligent leader (in your home in your community), and an articulate activist. And that's what we're trying to train everybody to do. So let's get started with this. There are some basic assumptions behind the entire industry of vaccination. In fact, when I got started with this in September of 2000... (the) You know, if you think about the the pharmaceutical industry is like a big pie diagram, and a piece of the pie is like cancer drugs, hypertension drugs. You know all these different drugs that they do which is all their book of business - their lines of things that they market and sell. At that point in time, the little teeny tiny pie diagram of the vaccine industry was about a five billion dollar a year industry. Now they're approaching fifty four billion. And why is that so important to know? If you vaccinate a hundred people, at least fifty percent of them are going to have a serious side effect. Then you get taken to all of these doctors and all of these tests to find out that was it the vaccine. Probably not, it was because you had this underlying pathology that was just going to automatically pop up just exactly when you got the vaccine. And then they've got this entire trillion dollar book a business to sell you all these drugs to manage the side effects that you just got from the vaccines. So the vaccines are actually the economical pharmaceutical industries loss leader. How many of you guys in here have businesses? Or your husband does? Or you know whatever, you have businesses. So you know what a loss leader is, right? A loss leader is like I'm gonna give away a t-shirt for free. It says on the door, I'm there on the sign on your door: free t-shirt, come inside. So you get people to come in for the free t-shirt. So while they're in your store, you can sell them the thousand dollar Armani suit. Well the vaccines are the economic loss leader. Do it for free, mandate it, get your flu shot at every Walgreens, Walmart, every grocery store. I got a thing the other day and somebody there, they took a picture of it. It said if you get your flu shot today at Giant Eagle we'll give you 10% off your groceries. So everywhere they're pounding people with these vaccines. It's their economic loss leader. It doesn't cost them anything, it costs them pennies, and then they've got a trillion dollar book of business to sell you once you start having side effects: asthma, allergies, eczema, ADD, ADHD, ear infections in kids, insulin-dependent diabetes, [and many other] autoimmune diseases. They have an entire textbook now on vaccines and autoimmune diseases. All of those things start happening. So now we can drive. It's the driver of the entire industry and these are some of the assumptions that vaccines are safe. We're gonna go through that in a little more detail. That vaccines are effective, meaning they protect you and keep you from getting sick. That we as physicians and you as a consumer, when you hear the word effective automatically goes into your head you think, "oh that keeps me from getting sick." That's not what effective means in the vaccine industry. Vaccines have very few side effects except for the fact of the vaccine injury compensation program, that went into effect in 1986 and the vaccine adverse event reporting system has year-to-date been paid out over $3.2 billion and vaccine injury claims through the government program and they estimate that's less than 10% of people have actually been injured. $3.2 billion in vaccine injuries. They are and every time you read any sort of a paper you hear anybody on the pro-vaccine advocate side, or you hear anybody in the government talk about vaccines, this is what they always say: that there's no significant public health advances of the 21st century. After all we saved the world from smallpox and polio, didn't we? We go into that great detail in my course because actually we didn't and we've spent billions of dollars for nothing on this polio eradication but that's another talk for another day. So what about our vaccine safe? And what is the meaning of a safe vaccine? Well it's not really what you think. The Webster's dictionary of safe says, "giving protection (which is what we think it should be, you know if you have a security system in your house that keeps you safe) involving no risk." Hmm no risk. Every bet package insert on every vaccine talks about the risk of vaccination. They are trustworthy and unable to cause trouble or damage. Well we've already said that vaccine injury compensation program is as paid out $3.2 billion and all of these vaccine injuries that compound one upon each other creates the business driver for the pharmaceutical industry so we know that they caused damage. So by definition they break the definition of what safe is supposed to be. So the real problem then comes become with vaccine safety studies. How do they come to the conclusion that they can put in a package insert, which is specifically designed for information for your doctor that your doctor is supposed to know? How do they design these studies and come to the conclusion that they are safe? Well there's four specific problems and problem number one is that safety studies do not use a true placebo group. And if you take anything away from this talk today I want you to remember this because in conventional medicine the double-blind placebo-controlled study is the gold standard for safety. If they're bringing to market say a new medication for say hypertension they would give you guys over here the real drug and you guys over here the sugar pill. And they would want to see a the real drug compared to the sugar pill what were the levels of side-effects, what kind of reactions did people have, did it really bring down your blood pressure as compared to this group over here that just got the sugar pill. And when they double-blind it, what that actually means is that the person that you come in to see to participate in the study when I give you a pill or I give you a pill, I don't know whether I'm giving you the real drug or if I'm giving you the sugar pill - I'm just giving you a pill. And then keeping track of your symptoms so that's a double-blind study I don't know which one which. Which of you are getting what. And placebo means it's compared to something that's totally inert. In vaccine studies they never use a true placebo. And that started all the way back with the polio trials back in 1954 when they did this mass vaccination of the Salk injectable polio vaccine and they said it was really unethical to give these people a vaccine and to give you nothing if we have to give a shot. So one of the two arms of the trial actually gave the placebo as a tetanus shot. So it started way back when that if you're gonna get a shot you ought to have something of value. And so then we get the side effects of the polio vaccine compared to the side effects of the tetanus shot. If this has the same amount of side effects as this then we say it has the same amount of side effects and reactions as the placebo, which was another vaccine, that's not a placebo. And now when the package inserts, they don't even call it a even try to get away with calling it a placebo anymore. What they call this tetanus shot, this other one that they give you, they call it a "comparator." We're going to compare the side-effects of the new vaccine compared to the side-effects of a vaccine that we already know what those side effects are supposed to be and if the new vaccine has the same amount of side effects as one that we know is supposed to be there then we say this new one is safe. There's no true placebo ever. And when I go to talk to doctors and nurses that are in the hospital and they don't have any of this information when I drop that little factoid of saying that there is no true placebo used when they just define safety and a safety trial - I would see it's kind of like a cartoon it's like their head cracks like an eggshell - like what do you mean that's the gold standard for all investigational medicine. Not in the vaccine world, it's not. What they use instead they consider because they consider it unethical to give a vaccine to one group and hold from another group. Therefore the placebo should have some benefit - it should be a vaccine. So can you see already where the whole idea that vaccines are safe starts to fall apart from the implementation of the safety studies. It just they've never really had a safety study. Problem number two is that studies don't use inert substances as a placebo - like a sugar pill should be, is inert. Well if we're going to compare one vaccine to another vaccine is this vaccine over here inert? No. because it has its own its own side-effect profile. So the placebo use is often another vaccine like I said with a known safety product profile. If the experimental vaccine has the same number and types of effects as the placebo vaccine, than the experimental vaccine is said to be safe as the placebo. And you see that in all the package inserts you see that in the published medical literature, in the Pediatric Infectious-Disease Journal, or in JAMA, in the New England Journal, they'll say it was safe as placebo. Then you dig through the study to try to find out what the placebo was, sometimes they list it and sometimes they don't. Sometimes you have to go to the FDA and look at the original trials to find out what the placebo was, but most of the time it was another vaccine. Another example, is that in the Gardasil trials that they actually used an injection of aluminum as the placebo. Gardasil has, well it used I used to say has the highest amount of aluminum of any vaccine, but the there's new vaccines that have come out that have larger amounts of aluminum. The Gardasil 4 that came out in 2006 had 250 micrograms of aluminum. Now Gardasil 9 that came out a couple of years ago and because it's become the one that they give everyone around the world has 500 micrograms of aluminum. And we're going to see in a few minutes that the new meningitis B vaccine has 1500 micrograms of aluminum, which is a big deal. So this is where in Gardasil.. You know what Gardasil is? Gardasil is the vaccine that they want to give all the girls, to say "one less girl." Yeah when they say one less girl I always what goes in my mind is one less girl able to have children in the future is what the rest of that sentence should be because Gardasil hasn't been shown to cause testicular atrophy in male mice and stop periods and atrophy of the uterus and female mice. So Gardasil is this vaccine that they that was only tested on 12,000 girls before they started administering it to 9 to 12 year old girls of age back in 2006. Most vaccine clinical trials on an international basis have tens of thousands of people this one was only tested on 12,000. They were followed for only six months, when in vaccine trials they usually find them for a follow things for about four years. And in medication trials they follow em for longer than that. The observation for adverse events was 15 days. How long does it take for an autoimmune reaction to form? Months! They only followed this because all they were looking for was acute allergic reactions, swollen arm, sick to their stomach, headache. They only followed it for 15 days. The average age for developing cervical cancer is somewhere between 38 and 42, and the placebo that was used was a shot of aluminum, and Gardasil has aluminum in it. So each Gardasil dose has 225 micrograms of aluminum and when about 25% experienced the injection and pain after the Gardasil and about 16% had pain after the shot of aluminum, the conclusion was Gardasil was declared to be as safe as the placebo. Which is pretty common. I mean this is just one example that I could give you of the 56 vaccines that are currently approved in the US market and there are almost 310 in the developmental pipeline. Now some of the vaccines in the developmental pipeline are specific indicators. A lot of them are in the cancer segment because what they're trying to do is come with DNA vaccines, to manipulate your DNA and genetics. Nothing could go wrong with that, right? Nothing could possibly go wrong with a DNA vaccine to change your genetics permanently and then pass that on to your children. But all of the vaccines and then they are coming up with specific indicator vaccines like there's a vaccine under development for cocaine addiction, one for hypertension, one for periodontal disease. Hmm so they're trying to eliminate dentists? I mean I don't know, but these are the sorts of things that are in development down the way. And so this was the vaccine that came to market that currently there are seven countries around the world that are about to ban the use of Gardisil and the international equivalent which is called Cervarix, because of all the deaths and chronic long-term disability that's being caused by this vaccine. So if you've got kids that are coming up teenagers, please get educated about this vaccine. And if there were any of them that you were gonna refuse - I mean in my opinion you should refuse all of them - but if you were going to refuse any absolutely do not allow your kids to get this vaccine. Because they're giving it to boys now too. They started that about five years ago. Primarily because they wanted to double their market share they felt like they were missing out on half the population. And because we know that those dirty little nine-year-old boys are going to be having sex with those promiscuous nine-year-old girls, and they're going to be sharing their HPV viruses back and forth. Because that's the age group that you have to give this because if you give it after you've had intercourse it doesn't work. 100% of the female population.. Well let me say that again. They estimate somewhere between around 98% of the entire female population has an HPV infection sometime in their life. I mean the cervix is an external organ, right? It's like your nose, it's an external organ. And about 98% of people actually have that infection sometime in their life and somewhere close to 97.5% of people who have the infection, clear in two years or less. So we're actually giving a vaccine because less than two percent of all humanity gets this vaccine and it doesn't or gets the virus and it doesn't go away within two years and maybe, maybe not causes cancer. But we're going to vaccinate the entire global population and destroy the lives of hundreds, if not thousands of teenagers, for really something that can be prevented with a pap smear. This is all the different concentrations of aluminum now, and we know that aluminum causes Alzheimer's. We're pretty sure that Alzheimer that aluminum contributes to other types of neurological conditions. Aluminum is once it's injected it stays in the muscle for an extended period of time and it's really not cleared from the body. So poison for poison in the last decade many studies and animal models have repeatedly demonstrated that aluminum can inflict immune-mediated diseases, autoimmune, neurological, and skin disorders. But yet we've got all of those vaccines that have a have aluminum in them including the hepatitis B vaccine that's given at birth. So if you get a vitamin K shot and a hepatitis B vaccine at birth, you get 330 micrograms of aluminum injected into your baby before they're two days old. And so then if they have problems down the road, how do you know? Because now the doctors will say, "Well, they were just born that way." Were they? Or was it all that gunk that you injected into them as soon as they landed on the planet. So, now what about some fewer problems with safety studies. So, so far we've said what there's no placebo, they don't use an inert substance. Problem number three, vaccine trials usually include three injections to create an antibody response. So they give the first one, they say that Prime's the pump. The second one locks in immunity, and the third one we want to take those antibodies to the moon. We want to make them sure that we make them as high as we possibly can because they all degrade and go away with time because it's false fake immunity. It's not even immunity it's a vaccination it's not giving your kids are you an immune response. It's injecting foreign matter into your body to create an antibody that we somehow think is going to protect you which it doesn't. So the vaccine trials the babies experience the side effects after the first dose he or she has dropped out from the trial and the data is analyzed on those that are remaining in the trial at the end. And the negative consequences of side-effects are left out. So what's let's boil that down into some really simple terms. Let's say that there were a thousand babies in this clinical trial and after the first vaccine a hundred of them dropped out because of side effects, and after the second vaccine another hundred dropped out because of side effects, and after the third vaccine another hundred of them dropped out because of side effects. When they look at the results and they look at the safety of the of this particular vaccine, they do the analysis on the 700 that were left. They don't even talk about the other 300 that dropped out, except to say a study investigators feel that none of the side effects were attributable to the vaccines. None of the side effects were attributable to the vaccines. For any of those 300 that dropped out. And so with a stroke of a pen in any vaccine safety or efficacy study they just wipe it out. Gone. Deleted. Hit the cutting room floor. Does not apply. And then they look at the with the rest of the analysis and say well it was the safest placebo. So now we go to claim stage for clinical trials. Stage one is bringing it to market. Stage two is small trials. Stage three is those thousand people (babies) we talked about. Now we just release it on humanity, that's stage four clinical trials. And they call it post marketing surveillance, to see how many people die or have serious consequences once we've unleashed it on humanity. And then everybody that reports a side effect or a problem, they go well we don't know if we can trust that report, it was just spontaneously reported, and maybe they were lying, maybe it had nothing to do with the vaccine. So it's all negated. Anything that is not just safe and effective is just one way or another deleted from the entire industry. So what was problem number three? They only analyzed the you know when people drop out side effects they aren't taken into consideration. And problem number four which i think is also a really serious complication, is when they when they set up a clinical trial, they only enroll healthy children or healthy and adults. I mean if you are a child and you have asthma, allergies, seizure disorders, autoimmune problems, you're not allowed into the vaccine study. You're not allowed in there. Same thing as if you're an adult. So you have to be like a healthy adult, and no medications, no underlying conditions that we know of. So now we'll do the studies on you so children with chronic illnesses are excluded even though those are the children who are most advocated to receive the vaccine after it comes to market. Or the adult that's most advocated to receive it. So if you if your children have say asthma and they were excluded completely from this new vaccine, say a new flu shot, once that new flu shot gets approved, your pediatrician will hammer you over the head to give your kid with asthma this new shot because oh my god you can't let them get sick. And so if you get this vaccine it's going to keep them from getting sick and they are the most susceptible because they do have an underlying condition, even though the clinical trials never included any of those kids to begin with. So this is just one example this was Prevnar 7, they now have Prevnar 13. So if you get a Prevnar 13 shot, that's like getting 13 vaccines in one needle. And you get five of those, at two, four, six months, one year, and they sometimes give a booster at five years of age. And this is what it says right from the study, right? Healthy infants were randomized one-to-one meaning you had 800 healthy kids and you've divided them into two groups to receive either Prevnar 7 or a meningitis C vaccine. Huh there's that comparator of another vaccine. To get it at two, four, six months, and somewhere between twelve and fifteen months of age. Children with sickle cell, known immunodeficiency, and any serious chronic progressive disease, a history of seizures, a history of either of either type of pneumococcal or meningococcal meningitis were excluded. But when Prevnar came to market the number one target were kids with those conditions: chronic ear infections, immunodeficiencies, sickle-cell, so kids that don't have a spleen, they were the ones who were absolutely advocated to get this vaccine, even though they were never tested in any of the clinical trials against kids who were chronically ill. I love this, this is my favorite quote. Figures don't lie, but Liars do figure. So they can take any statistic they want, and twist it around and manipulate it, cut out the kids that have side effects, you know don't take don't include kids that were sick, you know never use a true placebo. Use something like a shot of aluminum, that's good enough. So they can really figure it around whatever they want. So what are those takeaways? Safety studies don't prove safety. In fact, the US Supreme Court has actually ruled that vaccinations are unavoidably unsafe. Unavoidably unsafe by the US Supreme Court. The one size fits all vaccination schedule is dangerous and it's unproven and I think it's a fraud. Every vaccine is different, every combination in that vaccine is a little bit different, and every time it gets injected into you or your children.. I mean there's like 300 people in here how many different sets of genes do we think we have in here? 300, right? Because you're all came.. Even if you have twins, the genetics can be a little bit different. And if you've got two or three kids well think about how they behave at dinner. Do they all behave the same? No. do you think their genetics are exactly the same? They are not. So every vaccine is different with animal cells, DNA albumin, everything that's injected. So every vaccine, remember this, every vaccine is a true experiment. It's experimenting with you, what's happening inside of you, and what's happening to your children. Every human being is ejected with a different genetic constitution. So the takeaway from that section, really no placebo, distorted data, and every vaccine is a true experiment. Isnt this happy? I'm just celebrating now. Are you learning something new? Yes good, okay. Are vaccines effective? Well let me see, is that really not what we think. Webster's dictionary defines effective as, "adequate to accomplish a purpose producing an intended or expected result." Makes sense doesn't it? Something is going to be effective and fulfilling a specified function. Well how does that apply to vaccines? Okay because are vaccines effective? Well by that definition yeah they really are. Because what is happening when they research vaccinations, is they are injecting foreign matter into the body, into the muscle, and at some point in time in the future, weeks, sometimes months later, they take a blood test to see if that foreign matter caused your body to generate an antibody. And if it did then it fulfilled a specified function. It did what it was supposed to do, it created an antibody. So yes vaccines are effective from that perspective, but the presence of an antibody is doesn't guarantee you from getting an illness. So effective is not a synonym for protective or protection. Remember that. Every time you hear safe and effective. That sounds like a robot. To me safe and effective, safe and effective, it's never been proven to be safe and effective, means that foreign matter was injected into a body and it created an antibody. It doesn't mean it's going to keep you from getting sick. So all this massive push about flu shots, then we're going to talk about this afternoon this whole thing about flu shots, of how it protects you less, if you believe that it works, protects you, it works it works less than 14% of the time. And we're going to go into that in detail this afternoon. So remember this this is an important takeaway effective does not mean protection. How would you like to build new neural connections so that you can align your thoughts, emotions, and behaviors with what you ultimately want to achieve? You're in luck. You are innately endowed with the ability to train your brain to become an elite performer (if that's what you desire to do). Your Mental World For a moment, imagine your brain as if it is it's own planet. Your "neural planet" has a population of some 85 billion neurons. Just as people in close proximity interact with one another, neurons communicate to each other via synapses and neurotransmitters. A synapse is an electrochemical junction between two nerve cells, in which impulses pass by diffusion of chemicals, also referred to as neurotransmitters. If you took a consensus of your mental world, neurons of different sizes would be visible all over. Neurons that fire together look somewhat like a social gathering occurring. From a bird's-eye view, you would be able to see "remote villages" variably exchanging conversation, "towns" making more connections, and "large metropolitan areas" continuously in contact. Synapses vary in size because the frequency of neural communication dictates the size and efficiency of their pathway. Infrequently used trails can become freeways and vice versa. This connection between neurons, and clusters of neurons, is the essential function of the brain. Every time you think, feel, act, emotionalize, or remember, you reinforce existing brain neural connections or create new ones. There are neural patterns for everything, from standing to reading this page. The innumerable patterns in which your brain cells connect and share information reflects your brain's capacity to perform. Neuroplasticity: The Brain's Ability to Change ItselfThe old scientific paradigm held that you can't teach an old dog new tricks. Fortunately, the old paradigm has evolved and incorporated the science of neuroplasticity, which suggests the brain can change and it can happen at any time. Like plastic, neurons can mold into new forms, creating new connections. Any time you learn a new skill, the brain is changing by making new neural connections. Whether it is learning to play an instrument, speaking a new language, discovering a new route home, eating whole foods, and so much more, your brain begins to change itself. Learning is forging new connections. Remembering is maintaining and sustaining those connections. And just like a relationship, the more communication that occurs, the more bondage that takes place. Neurons are the same way. What is really fascinating, is that you can change your brain, not only by doing, but also by thinking. Researchers have demonstrated that the act of focusing and being present through meditation changes the brain in many ways. Neuroplasticity is the brain's ability to change itself, and it's the innate ability that you can harness to help you attain your goals. Continental Shift: Three Ways Neuroplasticity WorksYou are able to reshape your brain using the same principles that your brain was built - neurons firing and wiring, syncing and linking together. There are three ways that neuroplasticity can change your mind:
More neurons, more connections, and more efficient connections. These are the three ways to exponentially transform your life. But, there is a caveat. As an adult, some of your neuroplasticity is turned off. But once again, you're in luck, you can turn it back on. Teaching Old Dogs New TRicks: Turning On NeuroplasticityAs an infant, the brain is a sponge, absorbing what it can in an effort increase the chances of survival. As you age, your neuroplasticity slows down as new memories and skills are created; habitual patterns begin to direct most of your daily activities, and novel ideas get pushed to the back burner. As an adult, learning processes, beliefs, and behaviors become, more or less "fixed" within the neural pathways of the brain. This means the plasticity switch is predominately in the "off" position, to varying degrees in each individual. One person may be so set in their ways that to try to get them to see things from a new perspective is like talking to a brick wall. Whereas another person may be more flexible and is able to take all sides into consideration. In either case, neuroplasticity can work at any age, so in the case of that brick wall, the only thing holding them back is themselves. They're not old dogs who can't learn new tricks, they're just uninformed, or perhaps unwilling. Here are six time-tested principles to turn on neuroplasticity:
Here are some more ways to activity neuroplasticity:
Clearly more is better. Neuroplasticity is a ongoing process, and if you are committed to being the best version of yourself, then it is a lifelong process. References Assaraf, J. (2018). Innercise. Cardiff, CA: Waterside Press.
Dr. Joe Dispenza is teaching the world how to empower and heal our mind through meditation and mindfulness. His studies have proven that when well practiced these tools can put us on the path to understanding and breaking deep-rooted bad habits and even heal illnesses. The author of Becoming Supernatural explains how to stop your mind from controlling you on this episode of Impact Theory with Tom Bilyeu.
Transcript: It's a scientific fact that the hormones of stress downregulate genes and create disease. Long-term effects. Human beings because of the size of the neocortex, we can turn on the stress response just by thought alone. As I think about our problems and turn on those chemicals. That means then our thoughts could make us sick. So if it's possible, that our thoughts could make us sick then it is possible then our thoughts could make us well? The answer is absolutely yes. Everybody welcome to Impact Theory. Our goal with this show and company is to introduce you to the people and ideas that will help you actually execute on your dreams. Alright today's guest is a New York Times bestselling author and one of the most sought-after speakers in the world. He's lectured and given advanced workshops in more than 30 countries across five continents all with the aim of helping people better understand and unlock the power of their mind. His expertise is the intersection of the fields of neuroscience, epigenetics and quantum physics and he's partnered with other scientists across multiple disciplines to perform extensive research on the effects of meditation using advanced technologies such as epigenetic testing brain mapping with EEG s and gas-discharge visualization technology. Through his work he is endeavouring to help advance both the scientific community and the public at large as understanding of mind derived health optimization, a topic he covered extensively in his groundbreaking book, You Are The Placebo. His teaching has had such a profound impact on the way that people perceive a wide range of brain related topics around mindfulness and well-being. [that] He's a faculty member at the quantum University in Hawaii the Omega Institute for holistic studies in New York and the Kerr Paulo Centre for yoga and health in Stockbridge, Massachusetts. He's also an invited chair of the research committee at life University in Atlanta, as well as a corporate consultant where he delivers his lectures and workshops for businesses. So, please help me in welcoming the man who has appeared in such films as Heal, People Versus the State of Illusion and Unleashing Creativity, the author of the recent book Becoming Supernatural, Dr. Joe Dispenza. Thanks for being here. So, diving into your world and how you perceive the sense of self and the way that you marry science to - the way that we form memories the way that we live in a perpetual state of reliving our past and things like that. It's really, really incredible and I want to dive into the whole notion of you sort of being a habitual construct like what? What is that? What is the habit of you? Well a habit is a redundant set of automatic unconscious thoughts, behaviors and emotions that's acquired through repetition. The habit is when you've done done something so many times that your body now knows how to do it better than your mind. So if you think about it, people wake up in the morning, they begin to think about their problems. Those problems are circuits, memories in the brain, each one of those memories are connected to people and things at certain times and places. And, if the brain is a record of the past, the moment they start their day, they're already thinking in the past. Each one of those memories has an emotion. Emotions are the end product of past experiences. So the moment they recall those memories of their problems, they all of a sudden feel unhappy, they feel sad, they feel pain. Now how you think and how you feel creates your state of being. So the person's entire state of being when they start their day is in the past. So what does that mean? The familiar past will sooner or later be predictable future. So, if you believe that your thoughts have something to do with your destiny and you can't think greater than how you feel, or feelings have become the means of thinking, by very definition of emotions you're thinking in the past. And for the most part you're going to keep creating the same life. So then people grab their cell phone they check their WhatsApp. They check their texts. They check their emails. They check Facebook. They take a picture of their feet. They post it on Facebook. They tweet something, they do Instagram. They check the news and now they feel really connected to everything that's known in their life. And then they go through a series of routine behaviors. They get out of bed on the same side. They go to the toilet. They get a cup of coffee. They take a shower, they get dressed, they drive to work the same way. They do the same things. They see the same people, that pushed the same emotional buttons, and that becomes the routine and it becomes like a program. So now they've lost their free will to a program, and there's no unseen hand doing it to them. So when it comes time to change the redundancy of that cycle becomes a subconscious program. So now 95% of who we are by the time we're 35 years old is a memorized set of behaviors, emotional reactions, unconscious habits, hardwired attitudes, beliefs and perceptions that function like a computer program. So then person can say with their five percent of their conscious mind. I want to be healthy. I want to be happy. I want to be free, but the body's on a whole different program. So then how do you begin to make those changes? Well, you have to get beyond the analytical mind because what separates the conscious mind from the subconscious mind is the analytical mind and that's where meditation comes in, because you can teach people through practice how to change their brainwaves, slow them down. And, when they do that properly they do enter the operating system where they can begin to make some really important changes. So most people then wait for crisis or trauma or disease or diagnosis, you know, they wait for loss some tragedy to make up their mind to change and my message is, "Why wait?" You can learn and change in a state of pain and suffering or you can learn and change in a state of joy and inspiration. I think right now the cool thing is that people are waking up. That's really interesting. And where I found the the deepest hooks into how powerful this can be for somebody is when you talk about trauma and you've talked about how people experience a traumatic event, but they then basically rehearse it and how that then has this knock-on effect. So, what is that? Why do people find it so hard to get past trauma? Well, the stronger the emotional reaction you have to some experience in your life, the higher the emotional quotient, the more you pay attention to the cause, and the moment the brain puts all of its attention on the cause, it takes a snapshot and that's called a memory. So long-term memories are created from very highly emotional experiences. So what happens then is that people think neurologically within the circuitry of that experience and they feel chemically within the boundaries of those emotions. And so when you have an emotional reaction to someone or something most people think that they can't control their emotional reaction. Well, it turns out if you allow that emotional reaction, it's called a refractory period to last for hours or days, that's called the mood. I say to someone, "Hey, what's up think?" "I'm in a mood," "Well, why are you in a mood?" "Well I had this thing happen to me five days ago and I'm having one long emotional reaction." If you keep that same emotional reaction going on for weeks or months that's called temperament. Why is he so bitter? I don't know. Let's ask him. Why is he so bitter? "Why are you bitter?" "Well, I had this thing happened to me nine months ago." And if you keep that same emotional reaction going on for years on end that's called a personality trait. And so learning how to shorten your refractory period of emotional reactions is really where that work starts. So then people when they have an event what they do is they keep recalling the event because the emotions of stress hormones the survival emotions are saying pay attention to what happened, because you want to be prepared if it happens again. Turns out most people spend 70% of their life living in survival and living in stress. So they're they're always anticipating the worst-case scenario based on a past experience and they're literally, out of the infinite potentials in the quantum field, they're selecting the worst possible outcome and they're beginning to emotionally embrace it with fear and their conditioning their body into a state of fear. Do that enough times, the body has a panic attack without you. You can't even predict it because it's programmed subconsciously. So then you say to the person, "Why are you this way?" And they'll say, "I am this way because of this event that happened to me 15 or 20 years ago," and what that means from biological standpoint is that they haven't been able to change since that event. So then the emotions from the experience tend to give the body and the brain a rush of energy. So people become addicted to the rush of those emotions and they use the problems and conditions in their life to reaffirm their limitation, so at least they can feel something. So now when it comes time to change you say the person, "Why are you this way?" Well, every time they recall the event they're producing the same chemistry in their brain and body as if the event is occurring, firing and wiring the same circuits and sending the same emotional signature to the body. Well, what's the revelant behind that? Well, your body is the unconscious mind. It doesn't know the difference between the experience that's creating the emotion and the emotion that you're creating by thought alone. So the body's believing it's living in the same past experience 24 hours a day, seven days a week, 365 days a year. And so then when those emotions influence certain thoughts, and they do, and then those thoughts create the same emotions, and those same emotions influence the same thoughts, now the entire person's state of being is in the past. So then the hardest part about change is not making the same choice as you did the day before a period. And the moment you decide to make a different choice get ready because it's going to feel uncomfortable, it's going to feel unfamiliar. So why does it feel so uncomfortable? Is it because of the neurons that fire together wire together? So there's like an easiness to that loop. (Just because, literally, and you've talked very eloquently about this the way that the neurons connect in the brain how rapidly. I've seen you show footage of how rapidly those connections happen, which is pretty incredible." Is that what makes it so discomforting for people? I think that the bigger thing is that as we keep firing and wiring those circuits, they become more hardwired. So there you have a thought and then the program runs but it's the emotion that follows the thought. If you have a fearful thought you're gonna feel anxiety, the moment you feel anxiety your brains checking in with your body and saying, " Yeah, you're pretty anxious." So then you start thinking more corresponding thoughts equaled how you feel. Well, the redundancy of that cycle conditions the body to become the mind. So now when it comes time to change, a person steps into that river of change and they make a different choice in all of a sudden they don't they don't feel the same way. So the body says, "Well, you've been doing this for 35 years." Well, you're gonna just stop feel suffering and stop feeling guilty and stop feeling shameful and you're not gonna complain, or blame, or make excuses, or feel sorry for yourself. The body's in the unknown. So the body says I want to return back to familiar territory. So the body starts influencing the mind then it says, "Start tomorrow, you're too much like your mother. You'll never change. This isn't gonna work for you. This doesn't feel right." And so if you respond to that thought as if it's true, that same thought will lead to the same choice, which will lead to the same behavior, which will create the same experience, which produce the same emotion. I want to talk about that notion. Give me a little more detail. We mean by the body becomes the mind or the unconscious mind. What do you mean by that exactly? Well, those are two different things. Your body is your unconscious mind. In a sense, if you're sitting down and you start thinking about some future worst-case scenario that you're conjuring up in your mind and you begin to feel the emotion of that event, your body doesn't know the difference between the event that's taking place in your world, outer world, and what you're creating by emotion or thought alone. So most people then, they're constantly reaffirming their emotional states. So when it comes time to give up that emotion they can say, "I really want to do it," but really the body is stronger than the mind because it's been conditioned that way. So, the servant now has become the master and the person all of a sudden once they step into that unknown, they'd rather feel guilt and suffering because at least they can predict it. Being in the unknown is a scary place for most people because the unknown is uncertain. People say to me, "Well, I can't predict my future. I'm in the unknown." And I always say, "The best way to predict your future is to create it. Not from the known but from the unknown. What thoughts do you want to fire and wire in your brain? What behaviors do you want to demonstrate in one day? The act of rehearsing mentally, closing your eyes and rehearsing the action. The rehearsing the reaction of what you want. The action of what you want by closing your eyes and mentally rehearsing some action. If you're truly present, the brain does not know the difference between what you're imaging and what you're experiencing in 3D world. So then you begin to install the neurological hardware in your brain to look like the event has already occurred. Now your brain is no longer a record of the past. Now, it's a map to the future. And if you keep doing it, priming it that way, the hardware becomes a software program and who knows you just may start acting like a happy person. And then I think the hardest part is to teach our body emotionally what the future will feel like ahead of the actual experience. So, what does that mean? You can't wait for your success to feel empowered. You can't wait for your wealth to feel abundant. You can't wait for your your new relationship to feel love, or your healing to feel whole. I mean that's the old model of reality of cause and effect, you know waiting for something outside of us to change how we feel inside of us and when we feel better inside of us. We pay attention to whatever caused it. But what that means then is that from the Newtonian world that most people spend their whole life living in lack, waiting for something to change out there. What do you mean the Newtonian world? Newtonian world is all about the predictable. It's all about predicting the future. But the quantum model of reality isn't is about causing an effect. The moment you start feeling abundant and worthy you are generating wealth. The moment you're empowered and feel it, you're beginning to step towards your success the moment. You start feeling whole, your healing begins. And when you love yourself and you love all of life, you'll create an equal. And now you're causing and effect and I think that's that the difference between living as a victim - In your world saying "I am this way because of this person or that thing or this experience. They made me think and feel this way." When you switch that around you become a creator of your world and you start saying, "My thinking and my feeling is changing an outcome in my life." And now that's a whole different game and we start believing more that were creators of reality. So, how do we go from, "Okay, I have this negative emotion. It's controlling my life. It's got me in this cycle of I think about this emotion, which triggers a chemical reaction, which trains my body to feel that way, which makes it easier more likely I will do it again, and so now I'm in this vicious cycle." And it's unconscious right. You said, "Does your thinking create your environment, or does your environment create your thinking," which I thought was really, really interesting. So, how do we then go from that, like mechanistically, to begin this visualization process of something that's empowering, its me in a different state, it's my future self. Is it meditation? What does that look like? If you're not being defined by a vision of the future, then you're left with the old memories of the past and you will be predictable in your life. And, if you wake up in the morning and you're not being defined by a vision in the future as you see the same people and you go to the same places and you do the exact same thing at the exact same time, it's no longer that your personality is creating your personal reality. Now your personal reality is affecting or creating your personality. Your environment is really controlling how you think and feel unconsciously, because every person every thing every place every experience has a neurological network in your brain. Every experience that you have with every person produces an emotion. So some people will use their boss to reaffirm their addiction to judgment. They'll use their enemy to reaffirm their addiction to hatred. They'll use their friends to reaffirm their addiction to suffering. So now they need the outer world to feel something. So, to change them is to be greater than your environment, to be greater than the conditions in your world and the environment is that seductive. So then why is meditation the tool? Well, let's sit down. Let's close our eyes. Let's disconnect from your outer environment. So if you're seeing less things is less stimulation going to your brain if you're playing soft music or you have earplugs in, less sensory information coming to your brain. So you're disconnecting from environment if you can sit your body down and tell it to stay like an animal stay right here. I'm gonna feed you when we're done. You can get up and check your emails. You can do all your texts, but right now you're gonna sit there and obey me. So then, when you do that properly and the you're not eating anything or smelling anything or tasting anything, you're not up experiencing and feeling anything, you would have to agree with me that you're being defined by a thought, right? So when the body wants to go back to its emotional past, and you become aware that your attention is on that emotion, and where you place your attention is where you place your energy, you're siphoning your energy out of the present moment into the past and you become aware of that. And, you settle your body back down in the present moment because it's saying "Well, it's eight o'clock. You normally get upset because you're in traffic around this time and here you are sitting and we're used to feeling anger and you're off schedule. Oh, it's 11 o'clock and usually check your emails and judge everybody." Well, the body is looking for that that predictable chemical state every time you become aware that you're doing that and your body is craving those emotions and you settle it back down into the present moment, you're telling the body it's no longer the mind, that you're the mind. And now your will is getting greater than the program. And if you keep doing this over and over again, over and over again, over and over again, just like training a stallion or a dog, it's just gonna say, "I'm gonna sit." And the moment that happens, when the body's no longer the mind, when it finally surrenders, there's a liberation of energy. We go from particle to wave, from matter to energy, and we free ourselves from the chains of those emotions that keep us in the in the familiar past and we've seen this thousands of times. In fact, we can actually predict it now on a brain scan. That's so interesting. Let's go a little bit harder on metacognition, the notion that you don't have to believe everything you think. I love the way that you talk about that. Hmm. Yeah, and we have a huge frontal lobe. It's 40% of our entire brain, and most people when they have a thought they just think that that's the truth. And, I think one of my greatest realizations in my own journey was just because you have a thought, it doesn't necessarily mean it's true. So if you think 60 to 70 thousand thoughts in one day, and we do, and 90% of those thoughts are the same thoughts as the day before and you believe that your thoughts have something to do with your destiny, your life's not gonna change very much. Because the same thought leads to the same choice, the same choice leads to the same behavior, the same behavior creates the same experience, and the same experience produces the same emotion. And so then, the act of becoming conscious of this process, to begin to become more aware of how you think, how you act, and how you feel, it's called metacognition. And so then, why is that important? Because the more conscious you become of those unconscious states of mind and body, the less likely you're gonna go unconscious during the day. And that thought is not gonna slip by your awareness unchecked. It means to know thyself. And the word meditation means to become familiar with. So as you become familiar with the thoughts the behaviors and the emotions of the old self, you're retiring that old self as you fire and wire new thoughts and condition the body into a new emotional state. If you do that enough times, it'll begin to become familiar to you. So it's so important. Just like a garden, if you're planting a garden, you've got to get rid of the weeds. You got to take the plants from the past year and you got to pull them out. The rocks that sift to the top that are like our emotional blocks, they have to be removed that soil has to be tenderized and broken down. We have to we have to make room to plant the new garden. So primarily, we learn the most about ourselves and others when we're uncomfortable, because the moment you move into that uncomfortable state, normally a program jumps in. When that program jumps in, it's because the person doesn't want to be in the present moment and engage it consciously. So when you teach people how to do that with a meditative process, turns out that when they're in their life, they're less likely to emotionally react. They're less likely to be so rigid and believe the thoughts they were thinking. They're more aware of when they go unconscious back into a habit, and that is what starts the process of change. And, so we have to unlearn before we relearn. We have to break the habit of the old self before we reinvent a new self. We have to pre-synaptic connections and sprout new connections. We have to unfire and unwire and refire and rewire. We have to unmemorize emotions that are stored and then recondition the body that to a new mind into a new emotion. Like the deprogram and reprogram, that's the act, and it's a two-step process. Yeah, I like the way that you call that out as an action. There was another thing that you said that I thought was really powerful, about how insights themselves are essentially inert, they don't do anything. What what then do we do with an insight? How do we take a breakthrough moment and make sure that it's not just a breakthrough moment? Like I guarantee people watching right now are having like a hundred aha moments. For sure, that was definitely the case for me as I was researching you and when you said that I was like and that's the danger that you have the aha and then nothing. Yeah, and it is a danger, because then people will will shrink back into mediocracy and they'll use the insight to excuse them from taking a leap. They'll say, "Yeah, you know, I have a chemical imbalance in my brain. Yeah, my father was really overbearing, he was a perfectionist. That's why I am the way I am." You know people, they come up with stuff to excuse themselves. The insight is actually giving them permission to stay limited. And it's an amazing idea because they'll say to you that they really want to get over their anxiety. But let's ok. Let's take your ex-husband. Let's put him in a straitjacket. Let's duct tape them and shoot them to the moon know what I mean. What are you gonna do now? You still have to make those changes. And so then the person's enemy dies or they're something shifts in their life and that person's gone, they'll find another person to hate. This is just how we function as human beings. We just slide another reason to feel those emotions. So I think I think when people start to understand this, you know, I think knowledge is power. But knowledge about yourself is self empowerment. So how much of this is really learning to just bifurcate the world into (there's) negative emotions that have negative neurochemistry - associated with, and you said that in those states if you're living in a perpetual state of stress hormones and things like that illness is like a step away and then just the other side of that is understanding - (but there's) [and] this whole other side of positive energy, which happiness, joy, empowerment - whatever that you know neurochemical cocktail is, but that when you're on that side your immune system is more likely to function well. Is that just sort of bringing it down to like a really base level. Yeah, that's sort of one of the biggies. Well, let's talk about it in terms of survival or creation As I said 70% of the time people live in stress and living in stress is living in survival. Now, all organisms in nature can tolerate short-term stress, you know a deer gets chased by a pack of coyotes, when it out runs the Coyotes it goes back to grazing and the event is over. And the definition of stress is when your brain and body are knocked out of balance, out of homeostasis. The stress response is what the body innately does to return itself back to order. So you're driving down the road, someone cuts you off, you jam on the brakes, you may give them the finger and then you settle back down and the event is over and boom now everything's back back to normal. But what if it's not a predator that's waiting for you outside the cave, but what if it's your coworker sitting right next to you and all day long you're turning on those chemicals because they're pushing all your emotional buttons. When you turn on the stress response, and you can't turn it off, now you're headed for a disease because no organism in nature can live an emergency mode for that extended period of time. It's a scientific fact that the hormones of stress down regulate genes and create disease, long term effects. Human beings, because of the size of the neocortex, we can turn on the stress response just by thought alone, I can think about our problems and turn on those chemicals. That means then our thoughts could make us sick. So if it's possible that our thoughts could make us sick, is it possible that our thoughts could make us well? The answer is absolutely, yes. So then what are the emotions that are connected to survival? Let's name them, anger, aggression, hostility, hatred, competition, fear, anxiety, worry, pain, suffering, guilt, shame, unworthiness, envy jealousy. Those are all created by the hormones of stress. And psychology calls them normal human states of consciousness, I call those altered states of consciousness. So then we tend to remember those traumatic events more because in survival, you better be ready if it happens again. And in one's survival gene is switched on you could have ten really great things that happen to you in your day and you just have one bad thing that happens and you cannot take your attention off that unhappy thing because the survival gene is switched on. It's really interesting. How does epigenetics come into play in all this. What's actually happening? You've talked pretty profoundly about proteins and like really at a deep level how we're signalling to our genetics to create these kinds of changes. What does that actually look like? Well, epigenetics. Epi means above the gene. And many years ago after the DNA helix was discovered by Watson and Crick, they said the blueprints of life, you know, all diseases are created from genes. It turns out less than 5%, more like 1%. of people on the planet are born with a genetic condition like type 1 diabetes or Tay-sachs disease or sickle cell anemia. The other 95 to 99 percent are created by lifestyle and by choices. You can take to identical twins with the exact same genome, one dies at 51, the other one dies at 85, same gene different environment. So, all of a sudden they said, "We lied. That was wrong. It's not genes that create disease. It's the environment that signals the gene that creates disease." Well, ok, but that's not the whole truth too because you could have two people working side by side in the same factory, one gets cancer after being exposed to a carcinogenic for 25 years, both working for 25 years, he other one has no cancer at all. So there must be some internal order that would cause one person to not get it while another one does. So is it possible then, if the environment signals the gene, and it does, and the end product of an experience in the environment is called an emotion, can you signal the gene ahead of the environment by embracing an elevated emotion? We've done the research on this where we measured 7,500 different gene expressions in a group of people. It came to an advanced event for four days. And we had them doing a seated meditation, a walking meditation, a laying down meditation, a standing meditation. And at the end of four days, just four days, the common eight genes that were upregulated, two genes to suppress cancer cells and tumor growth; two genes for neurogenesis the growth of new neurons in response to novel experiences; and learning the gene that signals stem cells to go to damaged areas and repair them; the gene for oxidative stress was upregulated. We started seeing all these genes that are very, very healthy to cause the body to flourish. Imagine if people were doing that for three months. We also measured telomeres - the little shoestrings on the end of DNA that tell us our biological age. We asked people to do the work meditation five out of seven days for 60 days. Measure their telomeres that determine their biological age. sixty days later, seventy four percent of the people lengthen their telomeres, 40 percent significant change, twenty percent a very remarkable change. That means that they got a little bit of their life back if it lengthened by ten percent. They got 10% of their life back. That's incredible. Before I ask my last question tell these guys where they can find you online. Sure. My website is just https://drjoedispenza.com. You can follow us on Facebook, Twitter, Instagram, we're all over. And then my final question. What's the impact that you want to have on the world? I think that the end game for me is to empower people to such a degree that they realize that they need less things outside of them to make them happy, less things outside of them to regulate their moods and their behaviors, and that they begin to use the kind of the power that we all have access to, and into really, and to change the world, to make a difference so that there's more peace, here's more wholeness, there's more connection. That we support and love each other, and we serve better. And I think that we have to start for the most part if everybody's working on themselves. And trying doing their best to present the greatest ideal of themselves to the world, I think the world would be a better place. And so, that's my passion and I'm witnessing it happening now the more than I ever thought I would. That was incredible Joe. Thank you so much for being here and amazing having you. Meditation is the practice of being in the here and now. Researchers have long observed that meditation, or the sense of presence, has the ability to:
Meditation has the ability to fundamentally change the way you live. Researchers have observed individuals who meditate and have discovered that the human mind wanders nearly half of the day. Moreover, research suggests that a wandering mind is a better predictor of happiness, independent of financial security. In essence, if your mind is wandering, you are much less likely to be happy. The sense of the present moment determines happiness. Meditation develops two important skills to help keep the mind from wandering. The first is the ability to remain focused and attentive. The second, is the ability to recognize when the mind wanders so that it can gently be returned to the present moment. An crucial concept to grasp before diving into meditation is the relaxation response. In the modern world, stress is chronic. The modern world is deluged with a vast amount of information and moves at such as fast pace, and this places everyone experiencing it in a state of stress. This often results in a surge of cortisol and adrenaline, hormones released by the adrenal glands, which activates the sympathetic nervous system, also known as the fight or flight response. As a result, the mind turns outward, seeking to evaluate and resolve anything that is the source of the stress. Unless you are relaxed, out of fight or flight, you cannot meditate. Activation of the parasympathetic nervous system must occur (the mind must be turned inward) in order to practice meditation. This balance can be achieved by learning the relaxation response. Relaxation is the first step to meditation. The key to the relaxation response is noticing what happens in your body when the response is activated. What physiologic cues are revealed to you when you are relaxed? It is different for everyone. Some may experience a release of tension in the shoulders, others in the neck, many in the jaw. What is important is knowing when your body is relaxed and is ready to begin meditating. In 1975, Herbert Benson wrote the book "The Relaxation Response". As a cardiologist, he noticed that many of his patients who had high blood pressure felt worse with the medications that he prescribed. Patients simply visiting him made matters worse. Benson discovered that stress was the culprit and relaxation was the cure. Benson reluctantly began working with transcendental meditation meditators because they claimed to be able to reduce their blood pressure. He observed that they were in fact correct. The meditators were able to successfully reduce their heart rate, metabolic rate, and breath rate. Benson coined this effect the "relaxation response". After researching this phenomena more he discovered that the relaxation response could be triggered easily, quickly, and anywhere. Just as stress can be triggered in a variety of ways, so too can relaxation, including meditation. Benson later discovered four key components underlying the relaxation response:
Eventually, Benson later discovered that only the last two are required, a mental device and an allowing attitude, to activate the relaxation response. This means that anyone can tap into the relaxation response anywhere and anytime. ReferencesBenson, H., & Klipper, M. (2000). The relaxation response. New York: HarperCollins.
Fredrickson, B. L., Cohn, M. A., Coffey, K. A., Pek, J., & Finkel, S. M. (2008). Open hearts build lives: Positive emotions, induced through loving-kindness meditation, build consequential personal resources. Journal of Personality and Social Psychology, 95(5), 1045-1062. http://dx.doi.org/10.1037/a0013262 How many hugs have you had today? Neuroeconomist Paul Zak, also known as "Dr. Love," recommends at least eight hugs a day to feel happier and more connected, as well as nurture relationships. As psychotherapist Virginia Satir said: "We need 4 hugs a day for survival. We need 8 hugs a day for maintenance. We need 12 hugs a day for growth." There may very well be a "hug threshold" that allows your body to produce ample amounts of oxytocin, which is released in response to physical touch such as breast-feeding, orgasm, hugs, snuggling, holding hands, partner dance, massage, bodywork, and prayer. The neuropeptide oxytocin, released by your pituitary gland, is a naturally occurring hormone in the body with incredibly powerful, health-giving properties. This "love hormone" is also a key reason why the simple act of hugging is such an incredible way to enhance bonding with others but also boost your physical, and emotional, health. How Hugging Makes You Healthier Hugging increases levels of oxytocin, a neurotransmitter that acts as a hormone. This, in turn, has been observed to have beneficial physiological effects on your cardiovascular health and emotional happiness. One group of researchers observed, for example, a reduction in blood pressure among adults following a brief episode of warm contact with their partner. A 20-second hug, along with 10 minutes of hand-holding, reduces the harmful physical effects of stress, including its impact on your blood pressure and heart rate (Grewen, Anderson, Girdler & Light, 2003). This makes sense, since positive physical contact as hugging and reduces cortisol, increases oxytocin, and lowers systolic blood pressure in stressful situations (Holt-Lunstad, Birmingham & Light, 2008). But researchers suggest there is even more to it than that. The skin contains a network of tiny, egg-shaped rapidly adapting mechanoreceptors called Pacinian corpuscles with a large receptive field that can sense pressure and vibration and which are in contact with the brain through the vagus nerve. The vagus nerve winds its way through the body and provides input and receives sensation from the heart, liver, and digestive tract. (Freberg, 2006). The vagus nerve is also connected to oxytocin receptors. One theory is that stimulation of the vagus triggers an increase in oxytocin, which in turn leads to the cascade of health benefits. A 10-second hug a day can lead to biochemical and physiological reactions in your body that can significantly improve your health. Hugging has been observed to stimulates your nervous system while decreasing feelings of loneliness, combating fear, increasing self-esteem, defusing tension, and showing appreciation. According to researchers, hugging has been observed to (Forsell & Åström, 2012):
The effects of connection There's no doubt that physical touch of all kinds feels good. Whether it is a hug or a handshake, physical touch has a powerful effect on the human psyche resulting in us feeling happy, regardless if you are the toucher or touchee; connection, big or small, results in happiness. Yet, many people are touch-deprived. One poll found that one-third of people receive no hugs on a daily basis while 75 percent said they wanted more hugs. Findings such as these, coupled with the emotional and health benefits of human touch, have led to the emergence of cuddle therapy centers, where people can pay for a lunchtime cuddle. However, some have questioned whether or not physical contact from strangers has the same impact as those from someone you know and trust. While cuddling with a spouse or partner has been shown to boost satisfaction in relationships, some researchers have observed that hugs are only beneficial if trust is involved. Neurophysiologist Jürgen Sandkühler, Head of the Centre for Brain Research at the Medical University of Vienna actually cautioned against worldwide "free hugs" campaigns (where strangers offer hugs to others), saying that this may be perceived as threatening and actually increase emotional burden and stress. However, significant benefits have been found from cuddling with a pet, which shows hugs don't have to only be between humans to be beneficial to your heart and overall health. The Importance of Hugging On average, people spend on hour a month hugging. That doesn't seem like much, but when you consider that the average hug is 3 seconds long, that adds up to be a lot of hugs. And if you had any doubt about the importance of touch, consider that children who lack physical connection have delays in walking, talking, and reading. The act of hugging has a near-immediate impact on health, lowering your heart rate and inducing a calming effect while also leading to a more upbeat mood. Touch is described as a universal language that can communicate distinct emotions with startling accuracy. Researchers observed that touch alone can reveal emotions including anger, fear, disgust, love, gratitude, and sympathy, with accuracy rates of up to 83 percent (Hertenstein, Holmes, McCullough & Keltner, 2009). Hugging is a way to encourage your body to release oxytocin, and the more oxytocin your pituitary gland releases, the better able you are to handle life's stressors. Moreover, oxytocin quite likely plays a role in why pet owners heal more quickly from illness, why couples live longer than singles, and why support groups work for people with addictions and chronic diseases. Oxytocin has also been found to reduce the cravings of drug and alcohol addiction, as well as for sweets. It even has a positive influence on inflammation and wound healing. Even beyond this, regular hugs have the added benefit of:
Do You Need a Hug? Often making a concerted effort to hug the people close to you is one of the best ways to get more hugs in return. This can include your spouse, children, and other family members along with close friends. But even if you're not currently in a life situation conducive to getting daily hugs and producing enough of your own oxytocin on a regular basis, the good news is there are some alternatives you can use to help you deal in a healthy way with your emotional response to stress and anxiety. With the already known and still-to-emerge health and quality of life benefits to be derived from the natural release of oxytocin in your body, your best course of action is to make sure you're cultivating warm, loving, intimate relationships, no matter what stage of life you're in. Additionally, if you have a pet, just a few minutes petting your dog or cat can promote the release of your body's "happiness" hormones, including oxytocin. Since touch anywhere on your body, as well as positive interactions and psychological support, are known to increase oxytocin levels, you might also consider:
References Chillot, R. (2013). The Power of Touch. Retrieved from https://www.psychologytoday.com/us/articles/201303/the-power-touch
Forsell, L., & Åström, J. (2012). Meanings of Hugging: From Greeting Behavior to Touching Implications. Comprehensive Psychology, 1, 02.17.21.CP.1.13. https://doi.org/10.2466/02.17.21.CP.1.13 Freberg, L. (2006). Discovering biological psychology (2nd ed.). Wadsworth: Cengage Learning. Grewen, K., Anderson, B., Girdler, S., & Light, K. (2003). Warm Partner Contact Is Related to Lower Cardiovascular Reactivity. Behavioral Medicine, 29(3), 123-130. https://doi.org/10.1080/08964280309596065 Hertenstein, M., Holmes, R., McCullough, M., & Keltner, D. (2009). The communication of emotion via touch. Emotion, 9(4), 566-573. https://doi.org/10.1037/a0016108 Holt-Lunstad, J., Birmingham, W., & Light, K. (2008). Influence of a “Warm Touch” Support Enhancement Intervention Among Married Couples on Ambulatory Blood Pressure, Oxytocin, Alpha Amylase, and Cortisol. Psychosomatic Medicine, 70(9), 976-985. https://doi.org/10.1097/psy.0b013e318187aef Mercola, J. (2014). How Hugging Makes You Healthier and Happier. Retrieved from https://articles.mercola.com/sites/articles/archive/2014/02/06/hugging.aspx Richardson, J. (2014). 9 Reasons You Need To Be Giving and Receiving Hugs Everyday. Retrieved from http://preventdisease.com/news/14/012314_9-Reasons-Need-Giving-Receiving-Hugs-Everyday.shtml Zhivotovskaya, E. (2012). Oxytocin: Go Out and Touch Someone. Retrieved from https://positivepsychologynews.com/news/emiliya-zhivotovskaya/2012032321636 What can we all do to overcome the stress and anxiety that seems to pervade our news and daily interactions these days? In other words, how do we keep ourselves peaceful, healthy and thriving in these chaotic times we find ourselves in?
In this interview, Rosemary Gladstar shares a handful of herbs that can be used to keep your body centered and at peace – including one slightly controversial plant if you’re feeling adventurous. What is most striking about this interview is the deep wisdom that the legendary medicine woman shares. Her perspective is one worth listening to. The stress-healing herbs Rosemary mentions are:
|
The Awareness domain contains research, news, information, observations, and ideas at the level of self in an effort to intellectualize health concepts.
The Lifestyle domain builds off intellectual concepts and offers practical applications.
Taking care of yourself is at the core of the other domains because the others depend on your health and wellness.
Archives
May 2024
Categories
All
|

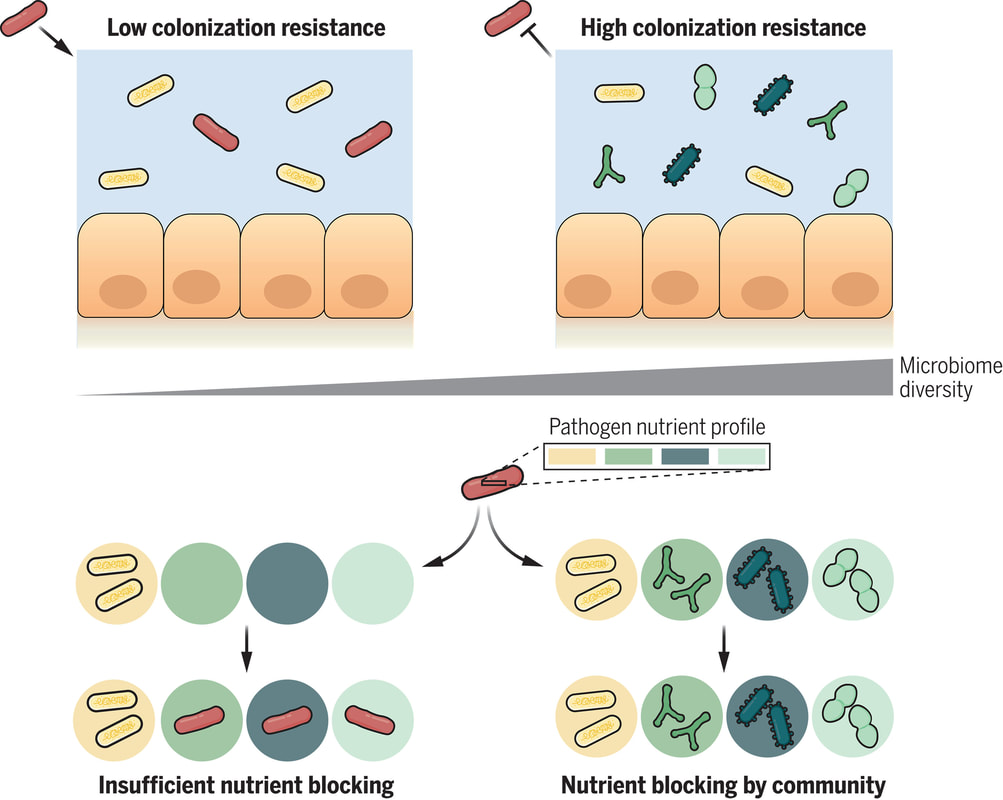

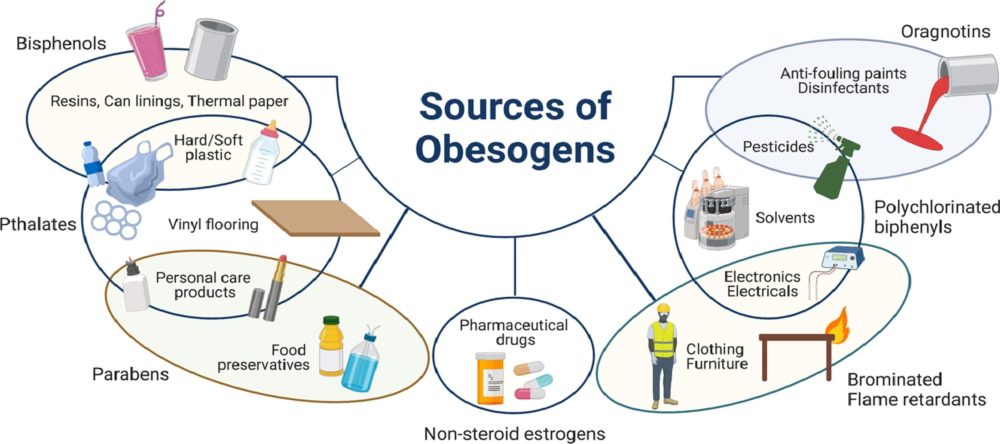

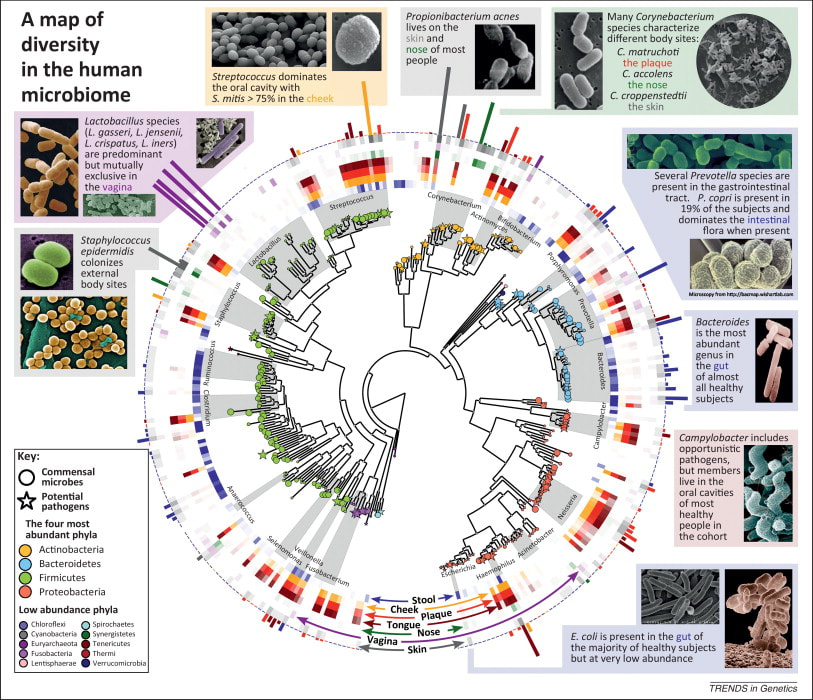

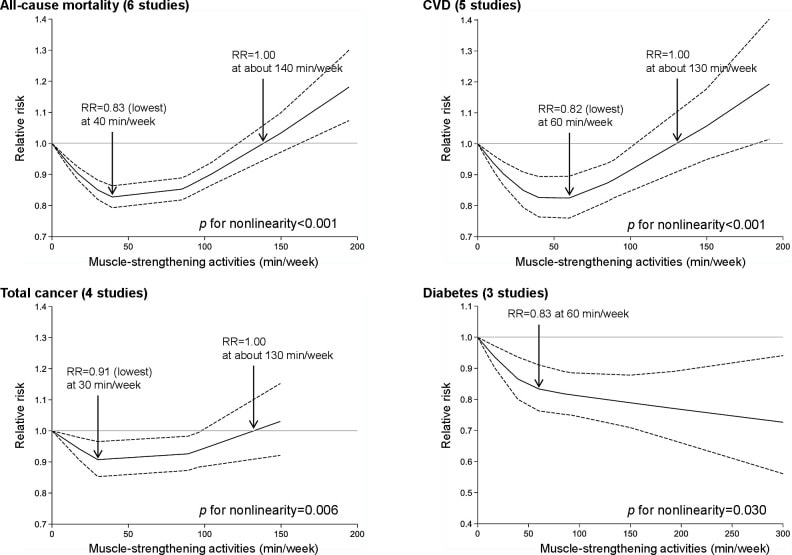
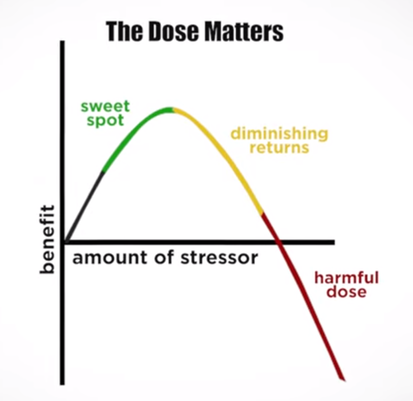
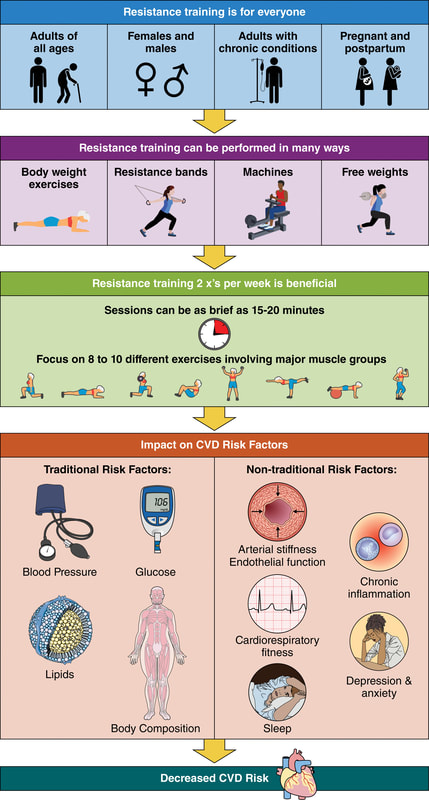
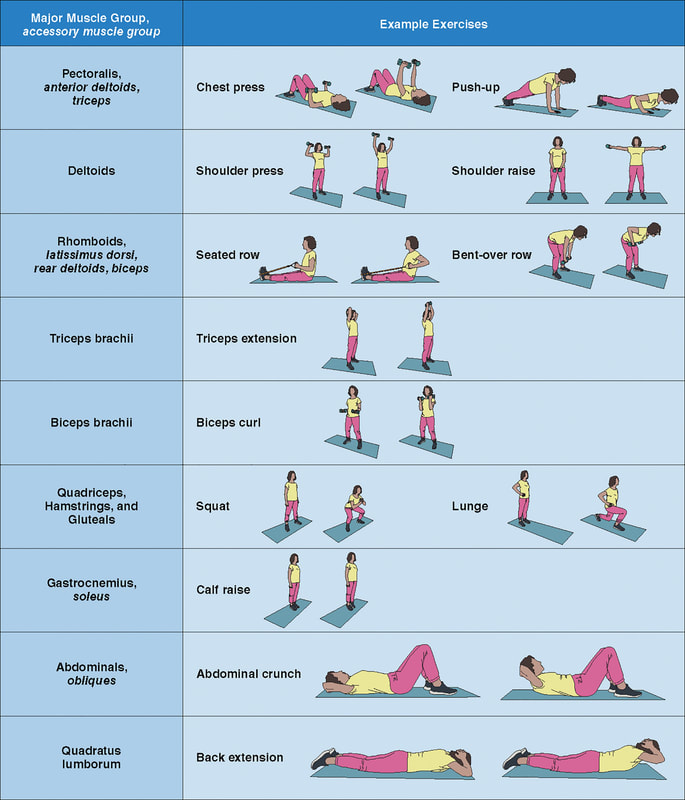
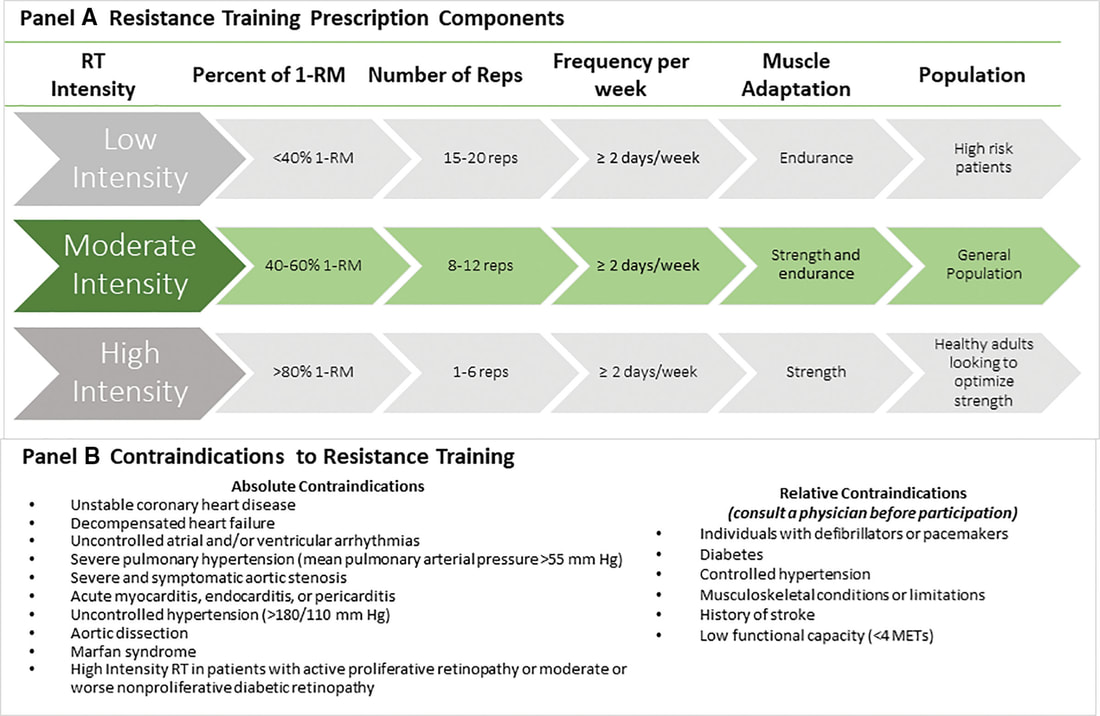

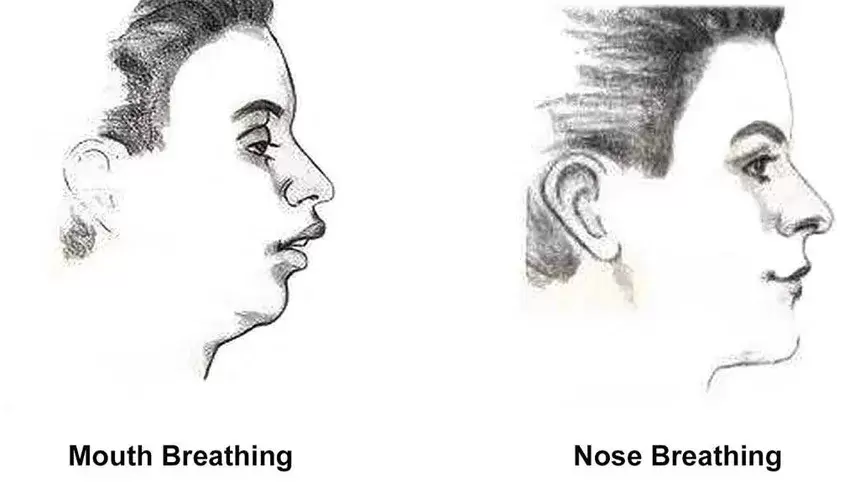
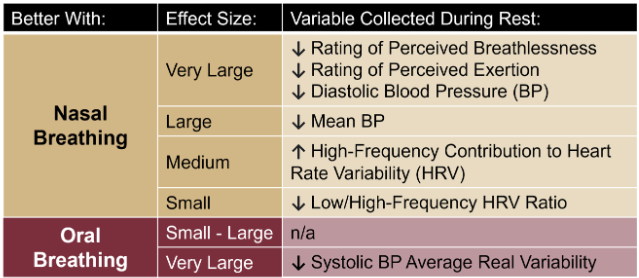
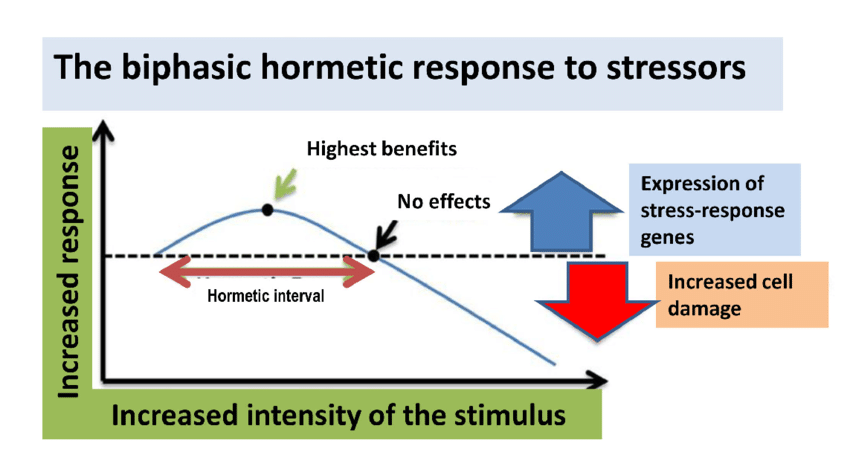
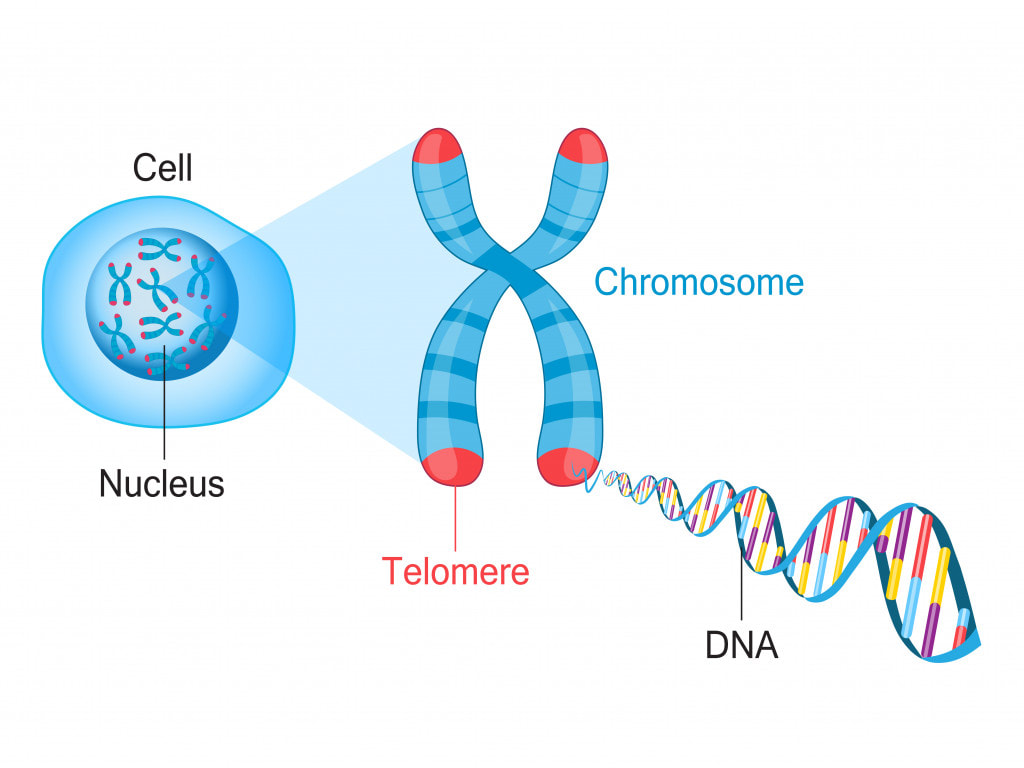




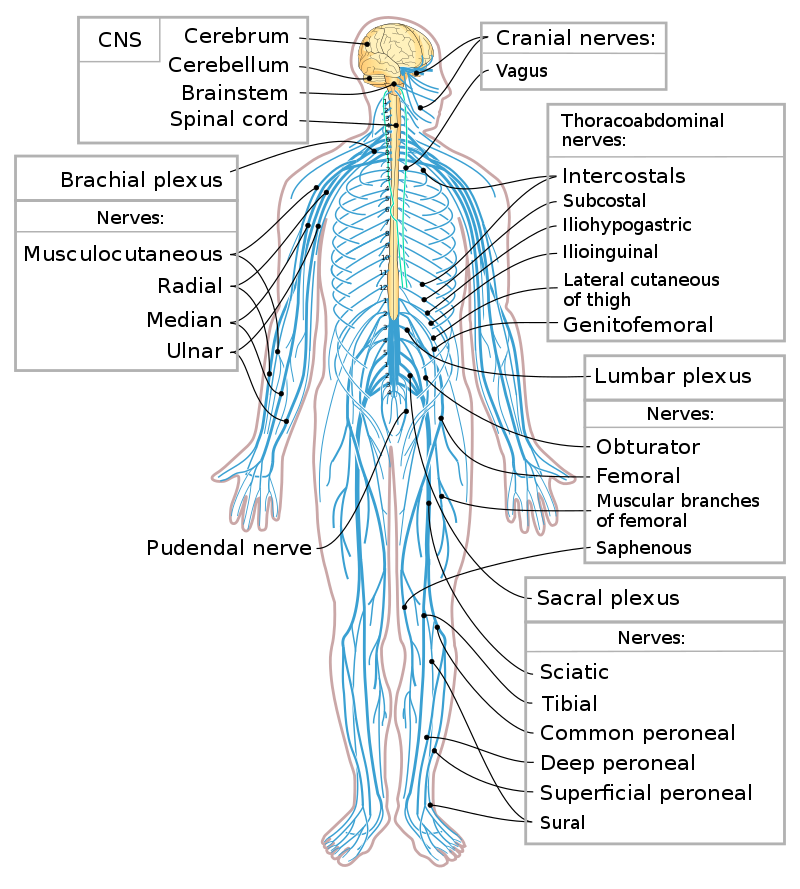
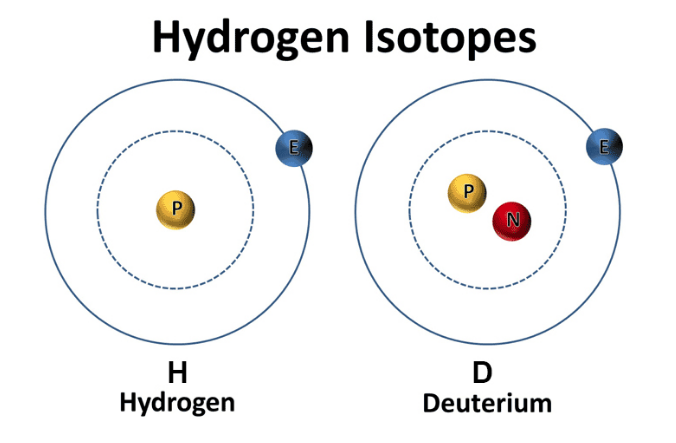
 RSS Feed
RSS Feed

