|
Allergies are a prevalent health concern affecting millions worldwide, triggered by the immune system's hypersensitive response to typically harmless substances. To comprehend allergies fully, it's crucial to delve into the intricate workings of the immune system, the specific mechanisms underlying TH2 allergic responses, and how a holistic approach rooted in addressing the root causes can offer relief. The Immune System: A Complex DefenderThe immune system is our body's defense mechanism against pathogens, toxins, and other foreign invaders. It comprises a sophisticated network of cells, tissues, and organs working together to identify and neutralize threats while maintaining tolerance to self. The TH2 allergic response is a specific immune reaction characterized by the activation of T-helper 2 (TH2) cells and the release of pro-inflammatory cytokines in response to exposure to allergens. This response is distinct from other immune responses, such as the TH1 response, which plays a role in combating intracellular pathogens. TH2 Allergic Response: Unraveling the MechanismsIn TH2-mediated allergies, the immune system overreacts to innocuous substances, such as pollen, pet dander, or certain foods. While pollen, dust mites, pet dander, and certain foods are common allergens that can induce allergic reactions in susceptible individuals, exposure to environmental toxins and pollutants can also contribute to allergic sensitization and exacerbation of symptoms. Environmental toxins such as air pollutants, industrial chemicals, pesticides, heavy metals, and volatile organic compounds (VOCs) have been associated with an increased risk of allergies and asthma. These substances can irritate the respiratory tract, disrupt the immune system, and promote inflammation, making individuals more susceptible to allergic responses. For example, air pollutants like ozone, nitrogen dioxide, sulfur dioxide, and particulate matter have been linked to respiratory allergies and asthma exacerbations. Exposure to indoor pollutants such as mold, tobacco smoke, volatile organic compounds (VOCs) from household products, and formaldehyde from building materials can also trigger allergic reactions and worsen symptoms in allergic individuals. Furthermore, certain environmental toxins have been shown to disrupt the normal functioning of the immune system, leading to dysregulation of immune responses and increased susceptibility to allergies. For instance, exposure to endocrine-disrupting chemicals (EDCs) like bisphenol A (BPA) and phthalates during critical periods of development has been implicated in the development of allergic diseases later in life. This exaggerated response involves the activation of TH2 cells and the release of pro-inflammatory cytokines, such as interleukin-4 (IL-4), interleukin-5 (IL-5), and interleukin-13 (IL-13). Upon exposure to an allergen, antigen-presenting cells (APCs) process and present the allergen to TH2 cells, initiating an immune cascade. TH2 cells then stimulate B cells to produce allergen-specific immunoglobulin E (IgE) antibodies, which bind to mast cells and basophils, priming them for future encounters with the allergen. Subsequent exposure to the allergen triggers the cross-linking of IgE antibodies on mast cells and basophils, leading to the release of inflammatory mediators, such as histamine, leukotrienes, and cytokines. This cascade of events culminates in the classic symptoms of allergies, including itching, sneezing, nasal congestion, and inflammation. Summary: th2 Allergy response
Upon re-exposure to the allergen, cross-linking of IgE antibodies on mast cells and basophils triggers the release of inflammatory mediators, such as histamine, leukotrienes, and cytokines. This cascade of events leads to the classic symptoms of allergy, including itching, sneezing, nasal congestion, and inflammation. 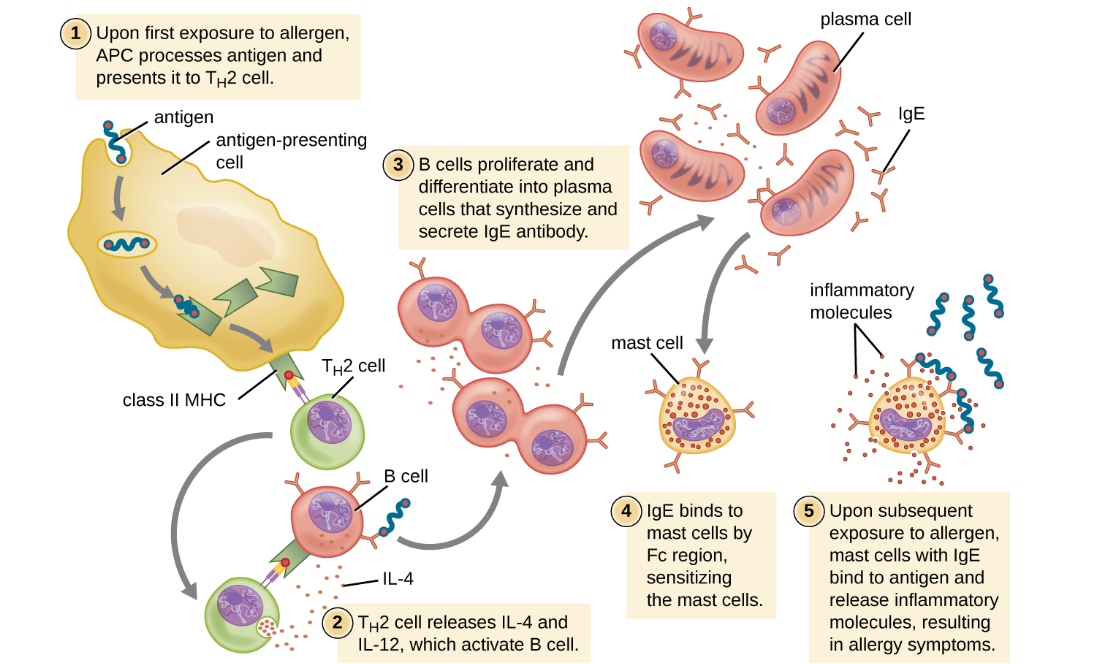 On first exposure to an allergen in a susceptible individual, antigen-presenting cells process and present allergen epitopes with major histocompatibility complex (MHC) II to T helper cells. B cells also process and present the same allergen epitope to TH2 cells, which release cytokines IL-4 and IL-13 to stimulate proliferation and differentiation into IgE-secreting plasma cells. The IgE molecules bind to mast cells with their Fc region, sensitizing the mast cells for activation with subsequent exposure to the allergen. With each subsequent exposure, the allergen cross-links IgE molecules on the mast cells, activating the mast cells and causing the release of preformed chemical mediators from granules (degranulation), as well as newly formed chemical mediators that collectively cause the signs and symptoms of type I hypersensitivity reactions. Relation to TH1 and Other Immune ResponsesThe TH1 response is involved in combating intracellular pathogens, such as viruses and certain bacteria. It is characterized by the activation of T-helper 1 (TH1) cells and the production of interferon-gamma (IFN-gamma) and other cytokines that promote cellular immunity. In a healthy immune system, there is a delicate balance between TH1 and TH2 responses. Imbalances, such as excessive TH2 activity or insufficient TH1 activity, can lead to immune dysfunction and increased susceptibility to infections, autoimmune diseases, or allergies. Regulatory T cells (Tregs) play a critical role in maintaining immune balance by suppressing excessive immune responses, including both TH1 and TH2 responses. Dysfunction of Tregs can contribute to immune-related disorders. In addition to TH1 and TH2 responses, the immune system employs various other mechanisms to combat pathogens and maintain homeostasis, including innate immunity, antibody-mediated immunity, and cell-mediated immunity. Understanding the interplay between different immune responses, including the TH2 allergic response and the TH1 response, is crucial for comprehending immune-related disorders and developing targeted therapeutic interventions. Balancing immune function and modulating specific immune pathways can help mitigate allergic reactions and restore immune equilibrium. Conventional approachesTH2 allergies are a common debilitation of quality of life for many individuals. While conventional over-the-counter pharmaceutical drugs are often used to manage symptoms, they frequently mask the underlying issue without addressing the root cause and can come with undesirable side effects. For example, Benadryl has been observed to result in birth defects and infant mortality. Common Pharmaceutical Drugs for Allergies:
Allergy supplement stack: A Natural alternativeFor those seeking alternatives to pharmaceutical drugs, a stack of naturally occurring compounds designed to supplant their use has emerged. This stack includes: 1. Whole Food Vitamin C: Known for its antioxidant properties and immune system support, whole food vitamin C can help regulate the immune response and reduce inflammation associated with allergies. 2. N-Acetyl Cysteine (NAC): NAC is a precursor to glutathione, a powerful antioxidant that helps combat oxidative stress and regulate the immune system. It has been shown to reduce inflammation and improve respiratory function in individuals with allergies. 3. Guduchi (Tinospora Cordifolia): A traditional Ayurvedic herb, guduchi has been used for centuries to support immune function and reduce allergic reactions. It possesses anti-inflammatory and immunomodulatory properties, making it beneficial for managing allergies. 4. Bromelain: Derived from pineapple, bromelain is a mixture of enzymes known for its anti-inflammatory and mucolytic properties. It can help alleviate nasal congestion and respiratory symptoms associated with allergies. Pharmacologic Effects of Allergy Supplement Stack:
Holistic Approach to Allergies: addressing the root causeIn contrast to conventional approaches that often focus solely on symptom management with pharmaceutical drugs, holistic modalities rooted in functional medicine address the underlying imbalances contributing to allergic responses. Here's how:
By addressing the root causes of allergies and promoting overall health and resilience, a holistic approach rooted in functional medicine offers a comprehensive solution for individuals seeking lasting relief from allergic symptoms. In conclusion, allergies represent a multifaceted challenge stemming from immune dysregulation and environmental triggers. By embracing a holistic approach rooted in functional medicine principles, individuals can effectively manage allergies, restore immune balance, and reclaim vitality and well-being. referencesKim, Hyon-Jeen, et al. “Nrf2 Activation by Sulforaphane Restores the Age-Related Decrease of TH1 Immunity: Role of Dendritic Cells.” Journal of Allergy and Clinical Immunology, vol. 121, no. 5, 1 May 2008, pp. 1255-1261.e7, www.jacionline.org/article/S0091-6749(08)00148-6/fulltext, https://doi.org/10.1016/j.jaci.2008.01.016
Engwerda, C. R., et al. “Bromelain Modulates T Cell and B Cell Immune Responses in Vitro and in Vivo.” Cellular Immunology, vol. 210, no. 1, 25 May 2001, pp. 66–75, pubmed.ncbi.nlm.nih.gov/11485354/, https://doi.org/10.1006/cimm.2001.1807. Singh, S. M., Singh, N., & Singh, V. (2009). Immunomodulatory and anti-tumor actions of Tinospora cordifolia (Guduchi). Natural Products: Chemistry, Biochemistry and Pharmacology, 114, 35-43. Belwal, T., Devkota, H. P., Hassan, H. A., Ahluwalia, S., Ramadan, M. F., Mocan, A., & Atanasov, A. G. (2018). Phytopharmacology of Acerola (Malpighia spp.) and its potential as functional food. Trends in food science & technology, 74, 99-106. Gilboa, Suzanne M., et al. “Use of Antihistamine Medications during Early Pregnancy and Isolated Major Malformations.” Birth Defects Research Part A: Clinical and Molecular Teratology, vol. 85, no. 2, Feb. 2009, pp. 137–150, https://doi.org/10.1002/bdra.20513. Accessed 10 Dec. 2019.
0 Comments
|
This portal contains research, news, information, observations, and ideas at the level of self in an effort to address lifestyle applications.
Archives
June 2024
Categories
All
|






 RSS Feed
RSS Feed

